 |
An intact and stable tear film is necessary for many vital functions. Among other things, it provides comfort and clarity that is often reduced in dry eye disease. While the relationship between tear composition and dryness is well-established, we often neglect the other microscopic yet essential components of the tear film that serve to protect our eyes from infection and damage. Besides comfort and a smooth refractive surface, the tear film is also our eye’s first line of defense, protecting us from pathogenic invasion.1
 |
| Schirmer’s test can help detect reduced aqueous production, indicating the need for clinical management. Click image to enlarge. |
Parts of the Whole
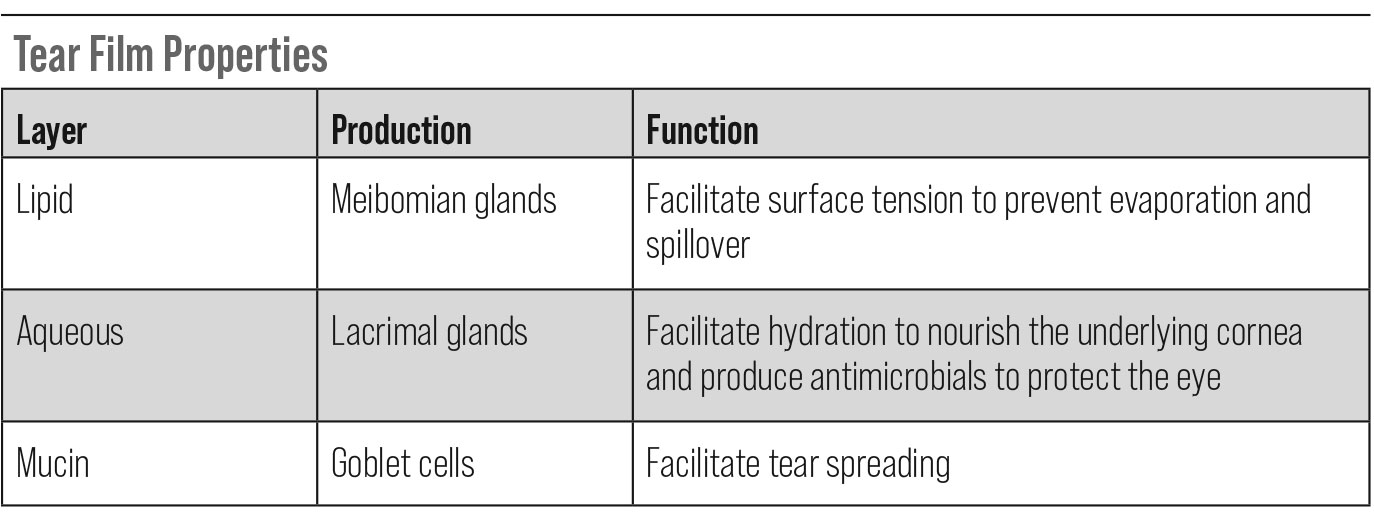
The tear film is a heterogenous, clear covering over the anterior surface of the eye. It serves as a barrier between the cornea and conjunctiva and the external environment.1 The tear film is composed of three distinct layers, which all contribute to its various functions.
The first, most outermost layer is the lipid layer, which is secreted by meibomian glands. This portion of the tear film provides surface tension necessary to prevent tear evaporation and keep the ocular surface smooth and well lubricated, while also preventing spillover onto the lid margin.2,3
The middle portion is the aqueous layer, which is produced by the lacrimal glands. This is a critical layer in that it is not only responsible for lubrication, hydration and nourishment of the underlying avascular cornea, but it also contains several molecules that serve as antimicrobials, protecting the eye from various external pathogens.
Finally, the innermost layer is the mucin layer of goblet cells, which assists in wettability and spreads tears with each blink.3
Since the eye is readily exposed to the external environment on a daily basis, it is subject to the invasion of many pathogens, including bacteria and fungi. Some of these common microorganisms of the ocular surface include the bacteria Staphylococcus aureus and epidermis, Streptococcus pneumonia and Pseudomonas aeruginosa. Fungal infections are usually caused by Aspergillus, Candida and Fusarium organisms. These pathogens are often implicated in bacterial or fungal keratitis associated with trauma or poor contact lens hygiene. In defense of these potential infections, blinking and reflex tearing flush out the tear film, while the tear film itself contains various antimicrobial defense proteins.2
One of the most common antimicrobial substances in the tear film is lysozyme.2,4,5 This is secreted by the lacrimal glands and found in the aqueous layer, functioning to destroy bacterial cells through the breakdown of peptidoglycan within the cell wall.5 It is mainly effective against gram-positive bacteria and constitutes approximately 20% to 30% of the total proteins found in tears.2 Lysozyme exhibits antifungal properties as well, as it is able to break down chitin, a component in fungal cell walls.2,5 One study also described its anti-HIV activity.2 In addition, decreased levels of lysozyme in the tear film have been reported in dry eye disease, herpetic disease and beta-blocker usage.4
Another abundant and important protein in the tear film is lactoferrin.2,4,5 This substance is also found in the aqueous layer and secreted by the lacrimal glands. Lactoferrin indirectly works as an antimicrobial by binding iron and undermining bacterial metabolism and growth.2,5
Similarly, lipocalin also binds molecules that transport iron and are produced by many types of bacteria and fungi, interfering with these harmful organisms’ iron uptake abilities. It is abundant in reflex tears and produced by the lacrimal glands.2
While the origin and exact mechanism is unknown, alpha-lysin is found in tears in higher quantities than those that are present in the aqueous and plasma, functioning to damage bacterial cell membranes.5
In addition to these proteins, there are immunoglobulins and antioxidants present in the tear film, both of which contribute to the antimicrobial activity of the ocular surface. Namely, secretory immunoglobulin A (sIgA) is the most copious and multifactorial in purpose. Its presumed mechanism of action is to coat microbes, preventing adherence to host cells and further neutralizing and lysing bacteria, viruses and parasites.2,5
As the eye is also subject to oxidative stress and damage due to constant environmental exposure, antioxidants such as ascorbic acid, uric acid, L-cysteine and L-tyrosine also protect the ocular surface by acting as free radical scavengers.1
 |
| Click table to enlarge. |
Takeaways
The functions of the tear film are many, and this covering’s antimicrobial properties are often under-appreciated. All of these microscopic components serve to combat harmful pathogens every day. A disruption in this composition is seen in many ocular surface disease processes, which should be considered when assessing the risk of potential ocular infection.
Dr. Labib graduated from Pennsylvania College of Optometry, where she now works as an associate professor. She completed her residency in primary care/ocular disease and is a fellow of the American Academy of Optometry and a diplomate in the Comprehensive Eye Care section. She has no financial interests to disclose.
1. Chen Y, Mehta G, Vasiliou V. Antioxidant defenses in the ocular surface. Ocul Surf. 2009;7(4):176-85. 2. McDermott AM. Antimicrobial compounds in tears. Exp Eye Res. 2013;117:53-61. 3. Cwiklik L. Tear film lipid layer: a molecular level view. Biochim Biophys Acta. 2016;1858(10):2421-30. 4. Wizert A, Iskander DR, Cwiklik L. Interaction of lysozyme with a tear film lipid layer model: a molecular dynamics simulation study. Biochim Biophys Acta Biomembr. 2017;1859(12):2289-96. 5. Davidson HJ, Kuonen VJ. The tear film and ocular mucins. Vet Ophthalmol. 2004;7(2):71-7. |

