 |
With primary open-angle glaucoma (POAG) being one of the leading causes of blindness worldwide, there is continual effort to explore and develop new modalities to treat this condition.1 Although the pathophysiology of glaucoma is a multifactorial and complex mechanism leading to retinal ganglion cell (RGC) damage, managing intraocular pressure (IOP) is the only modifiable risk factor at this time.1-3 This is made possible through topical or surgical processes that enhance aqueous outflow and thus lower IOP. First-line topical therapies include prostaglandin (PG) analogs, due to their efficacy and ease of administration.
More recently, the supplementation of nitric oxide (NO) has made PGs even more efficacious, introducing a new avenue for the potential treatment of glaucoma.4 In conjunction with PGs, which target uveoscleral aqueous outflow, NO is implicated in structures that are responsible for aqueous outflow using the predominant conventional pathway.1,2 NO augments the IOP-lowering effect and has neuroprotective and ocular perfusion properties.1-5.
Background
NO is a signaling molecule found throughout the body and in multiple organs. It is lipophilic, allowing it to readily cross the cell membrane and reach numerous targets. As such, NO is responsible for various physiological processes, including smooth muscle relaxation, vasodilation, blood pressure regulation and vascular homeostasis. Endogenous NO is produced from the enzyme nitric oxide synthase (NOS) and is available in three distinct isoforms, each with different functions that affect the corresponding ocular structures.2
The first and most important isoform is endothelial NOS (eNOS), which was first studied in the cardiovascular system as a vascular regulator. Within the eye, eNOS is an important molecule involved in the conventional aqueous outflow pathway and its primary structures, the trabecular meshwork (TM) and Schlemm’s canal. Expression of eNOS in these locations aids in increasing outflow facility and thus lowers IOP. Moreover, studies have shown that gene polymorphisms of eNOS are associated with an increased risk of POAG development.2
The second isoform is neuronal NOS (nNOS). This form is expressed anteriorly in the ciliary body, particularly the non-pigmented epithelium, and posteriorly in the optic nerve head and retina. Within the retina, it is expressed by the amacrine cells, photoreceptors and RGCs. It has been postulated that the nNOS variant is responsible for controlling ocular blood flow as well as acting as a messenger between cells within the inner neural retina, such as RGCs.2
Finally, inducible NOS (iNOS) is available only in pathological conditions such as inflammation and ischemia. Increased levels of iNOS have been found in POAG patients with visual field loss. This isoform may also play a role in mediating pressure-induced NO release.2
 |
|
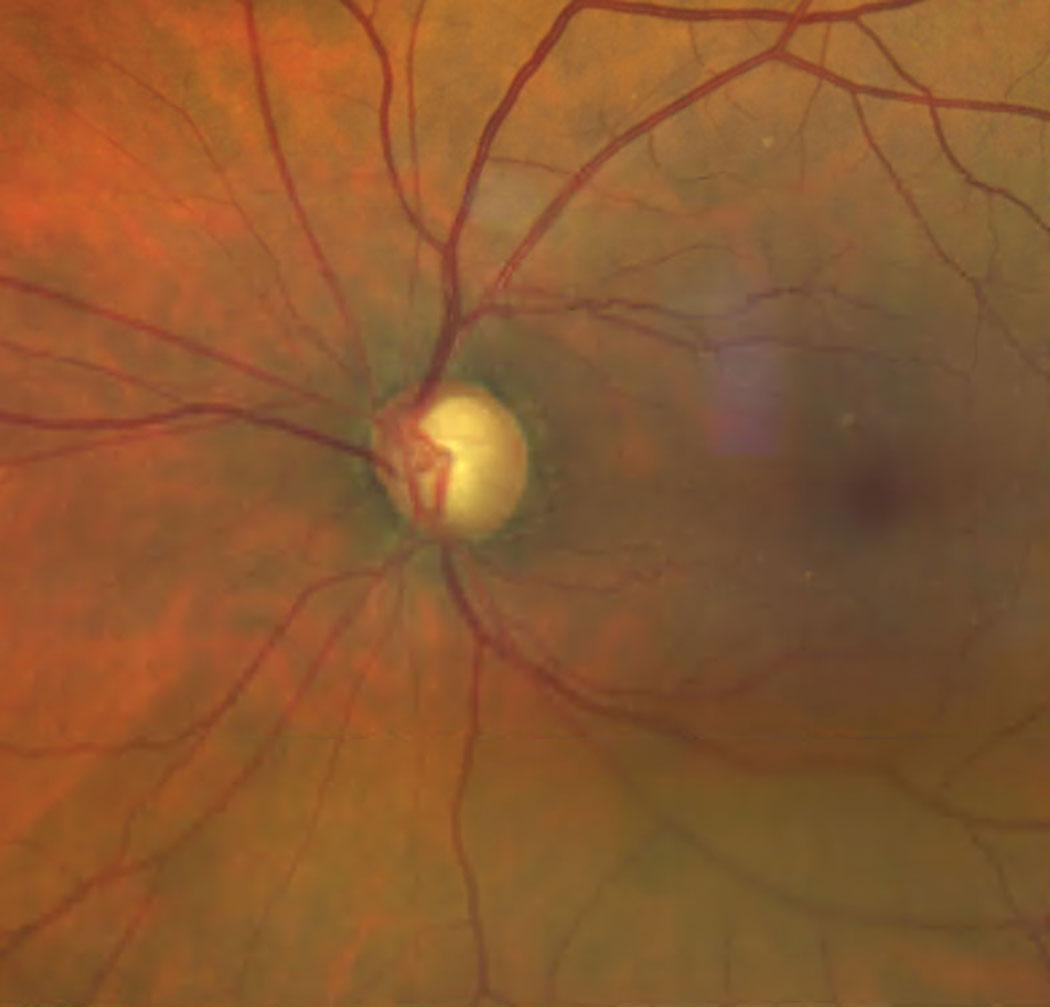
NO is a viable treatment option for eyes with POAG. Click image to enlarge. |
Benefits
NO offers patients several clinical perks, including the following:
• IOP regulation. When IOP is elevated in healthy eyes, the subsequent narrowing of Schlemm’s canal and stress on the system causes a cellular response where NO is released in higher quantities. This response leads to an increase in canal permeability and a decrease in TM contractility, allowing for the normalization of IOP.2 The effect on the TM also impacts diurnal IOP fluctuations, which are dampened with a healthy TM.1 In patients with ocular hypertension or POAG, this response to IOP and stress is absent, highlighting the role of NO inhibition in glaucomatous pathology.2
• Ocular perfusion. In addition to the effect on aqueous outflow dynamics, NO has been implicated in optic nerve head perfusion. NOS inhibition has been found to impair blood flow to the optic nerve in POAG patients compared with healthy controls.2 This mechanism of glaucomatous damage due to vascular dysregulation is well-established and can be, in part, explained by NO. The molecule is a vasoactive factor that is produced by the vascular endothelium and is important for maintaining basal flow within the retina and optic nerve head. In cases of elevated IOP, NO aids in autoregulation, which may explain its role in the development or exacerbation of POAG.2
• Neuroprotection. NO has been shown to exhibit both neurotoxic and neuroprotective properties. While elevated levels have been implicated in diseases such as Alzheimer’s and even in RGC degeneration, activation of NO has also been shown as an inhibitor of apoptotic cell death. In animal models, NO donor compounds have elicited potential neuroprotective properties.2 The ocular perfusion properties of NOS promote vasodilation and vascular permeability, contributing to possible neuroprotection.5
Treatment
Currently, the only FDA-approved topical agent for the treatment of glaucoma that makes use of NO is Vyzulta (latanoprostene bunod 0.024%, Bausch + Lomb). The drug is a NO-donating derivative of latanoprost. Clinical trials demonstrated clear superiority of this agent compared with PGs alone, as well as with other topical treatments. This should come as no surprise, as the combination of ingredients acts on both routes of aqueous outflow.4 Furthermore, studies have demonstrated that even high dietary nitrate intake was associated with up to a 21% reduced risk of incident POAG. This includes NO sources from dark, leafy green vegetables (lettuce, kale, broccoli, spinach), celery, potatoes and onions.3,6
Takeaways
Appropriately managing patients with POAG is imperative to preserving visual function. With IOP remaining the only modifiable risk factor, it is important to familiarize yourself with newly available options, research and factors in determining treatment efficacy.
Dr. Labib graduated from Pennsylvania College of Optometry, where she now works as an associate professor. She completed her residency in primary care/ocular disease and is a fellow of the American Academy of Optometry and a diplomate in the Comprehensive Eye Care section. She has no financial interests to disclose.
1. Aliancy J, Stamer WD, Wirostko B. A review of nitric oxide for the treatment of glaucomatous disease. Ophthalmol Ther. 2017;6(2):221-32. 2. Wareham LK, Buys ES, Sappington RM. The nitric oxide-guanylate cyclase pathway and glaucoma. Nitric Oxide. 2018;77:75-87. 3. Reina-Torres E, De Ieso ML, Pasquale LR, et al. The vital role for nitric oxide in intraocular pressure homeostasis. Prog Retin Eye Res. 2021;83:100922. 4. Impagnatiello F, Bastia E, Almirante N, et al. Prostaglandin analogues and nitric oxide contribution in the treatment of ocular hypertension and glaucoma. Br J Pharmacol. 2019;176(8):1079-89. 5. Galassi F, Renieri G, Sodi A, et al. Nitric oxide proxies and ocular perfusion pressure in primary open angle glaucoma. Br J Ophthalmol. 2004;88(6):757-60. 6. Ramdas WD. The relation between dietary intake and glaucoma: a systematic review. Acta Ophthalmol. 2018;96(6):550-6. |

