 |
Q:
My 56-year-old patient presented with a “droopy” eyelid and double vision that could only be relieved by squinting. How should I proceed with my differential?
A:
David J. Baptiste, OD, of El Paso, Texas, recently saw a patient who was at home under quarantine because she is a healthcare worker and was exposed to the coronavirus. On day eight, she contacted Dr. Baptiste after noting ptosis of her left upper lid and was concerned that it was related to COVID-19. Dr. Baptiste had just seen the patient for her annual eye exam three weeks prior and only noted s/p monovision LASIK with 20/20 vision OD distance and J1 OS for near. Interestingly, she had just reduced the dosage of her Plaquenil (hydroxychloroquine, Sanofi-Aventis) that she was taking for rheumatoid arthritis.
“Following our COVID-19 protocols, we saw her as an emergency patient in-office in order to assess her concerns,” Dr. Baptiste notes.
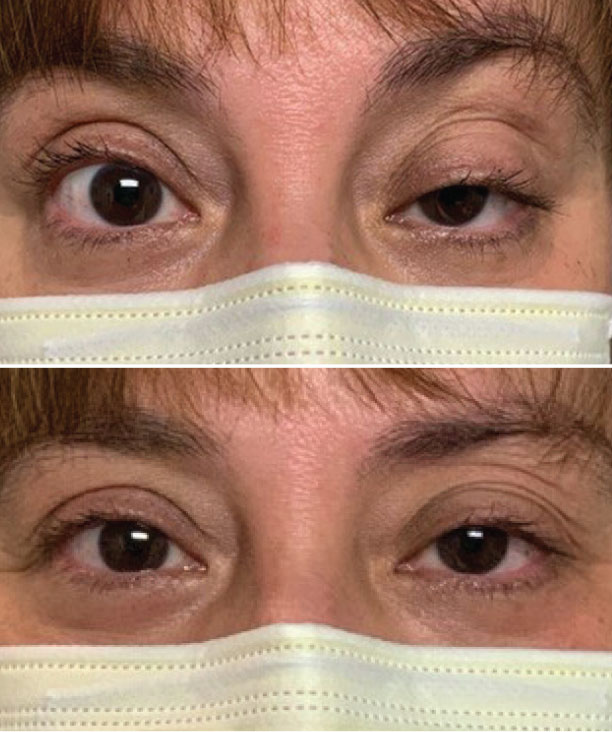 |
| Figs. 1 and 2. The ice pack test can help diagnose MG associated with lid ptosis. Click image to enlarge. |
The Three Amigos
According to Dr. Baptiste, there are three conditions that the optometrist should initially consider: Bell’s palsy or facial nerve palsy, cranial nerve (CN) involvement or myasthenia gravis (MG).
Bell’s palsy, sometimes referred to as idiopathic facial palsy, is a form of temporary facial weakness or paralysis, usually on one side. “It results from CN VII (facial nerve) dysfunction and the etiology is usually unknown,” Dr. Baptiste notes. Bell’s palsy has recently been reported as one of the growing number of neurological complications from COVID-19.1
The patient’s diplopia complaints caused Dr. Baptiste to consider the involvement of the cranial nerves III, IV and VI, leading to a check of extraocular muscle (EOM) function. Other than the ptosis, there was no facial asymmetry. Dr. Baptiste ruled out motility restrictions and anisocoria, and there were no confrontation field defects and no afferent pupillary defect.
Conduct an Ice Pack Test
Dr. Baptiste’s final consideration, since it can mimic many EOM palsies, was MG. With the significant onset of ptosis, performing the ice pack test was an easy way to gather evidence to support a diagnosis.
“Place an ice-filled bag over the affected eyelid for two to three minutes,” Dr. Baptiste says. The transient resolution of the ptosis occurs because the cold temperature decreases the breakdown of acetylcholine at the neuromuscular junction. The patient’s lid droop improved to almost equal the opening of the palpebral fissure of the fellow eye (Figures 1 and 2).
What’s Next?
Dr. Baptiste then referred the patient to a neurologist to rule out MG. Blood work was drawn and an MRI with contrast was performed. The MRI was normal, and all ordered labs were myasthenia gravis seronegative. The test for COVID-19 was also negative.
Despite the results, the neurologist felt strongly that it was ocular myasthenia, supported by the ice pack test.
The patient was started on a course of Mestinon (pyridostigmine, Bausch + Lomb), after which the ptosis intermittently improved. Oral prednisone was eventually added to her regimen, resulting in further resolution. The neurologist told the patient he could not predict if the ocular myasthenia would progress to generalized MG.
The patient has joined a Facebook MG support group where many said that it took them years to be diagnosed. “Thanks to you, I discovered the diagnosis quickly, and for that I am grateful,” the patient wrote to Dr. Baptiste.
| 1. Elkhouly A, Kaplan A C Noteworthy neurological manifestations associated With COVID-19 infection. Cureus 12(7): e8992. |

