 |
A 64-year-old Hispanic female presented for evaluation of a sudden onset of painless vision loss that started eight days earlier. While she was immediately evaluated and treated at a local hospital, her visual outcome did not improve. In fact, in the eight days since her hospital visit, additional symptoms began to manifest. These included bilateral temporal headaches with fluctuations in severity as well as diffuse scalp tenderness. She denied any pain from prolonged chewing and did not report any bouts of weight gain or recent fevers. Her medical history is positive for hypertension for the past decade, which is currently controlled with amlodipine.
On examination, best-corrected visual acuities were hand movements OD and 20/20 OS, with a prescription of -1.50 +1.00 x 180 OD, -1.75 +1.00 x 005 OS. Her extraocular motility for both eyes was full and extensive. Confrontation visual fields revealed a generalized depression of the right eye, while the left eye was full. Her pupils were equal, round and slowly reactive to light with a 3+ afferent pupillary defect in the right eye.
Color vision measured with Ishihara plates was severely reduced for the right eye only (0/10 OD, 10/10 OS). Her intraocular pressures were measured at 17mm Hg OD and 18mm Hg OS using the Tonopen (Reichert). Anterior segment health revealed 1+ nuclear sclerotic cataract in both eyes. A dilated fundus examination was performed and is available for review (Figure 1). Fluorescein angiography (FA) was also performed and images are available for review (Figure 2).
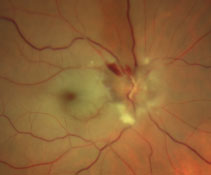 |
| Fig. 1. This magnified, widefield image shows our patient’s right eye. |
Take the Retina Quiz
1. How would you characterize the images from the fluorescein angiogram at 29 seconds?
a. Patchy choroidal filing.
b. Silent choroid.
c. Delayed arterial filling.
d. Neovascularization of the disc.
2. How would you describe the macular changes in the right eye?
a. Serous detachment of neurosensory retina.
b. Beaten metal appearance.
c. Cherry red spot.
d. Neuroretinitis.
3. Which condition is most consistent with the fundus appearance of the right eye?
a. Branch retinal vein occlusion.
b. Branch retinal artery occlusion.
c. Central retinal artery occlusion.
d. Stargardt’s macular degeneration.
4. What is the most likely underlying cause of the patient’s right fundus findings?
a. Elevated intracranial pressure.
b. Hypertension/atherosclerosis.
c. Giant cell arteritis.
d. Hereditary.
5. What is the most appropriate treatment for this patient?
a. Counsel on proper blood pressure control and refer back to the PCP.
b. Immediate initiation of oral antibiotics.
c. Immediate initiation of IV and oral steroids.
d. Prescribe Diamox (acetazolamide, Teva).
Diagnosis
Based on the history and clinical presentation, the patient was diagnosed with a central retinal artery occlusion of the right eye, most likely secondary to giant cell arteritis (GCA). Lab studies were ordered which revealed an elevated erythrocyte sedimentation rate (ESR) value at 62mm/hr and an elevated CRP value at 2.6mg/L. In addition, CBC with differential revealed an elevated white blood cell count.
She was immediately sent to the hospital, where she was placed on intravenous methylprednisolone and monitored over night. The patient was discharged the next morning with a prescription of 80mg of oral prednisolone. On follow-up lab testing, she had a marked reduction in the ESR level from 62mm/hr to 17mm/hr and a reduction in the CRP value from 2.6mg/L to 1.1mg/L. While her vision did not improve, the bilateral temporal headaches and scalp tenderness significantly subsided upon initiation of the steroid treatment.
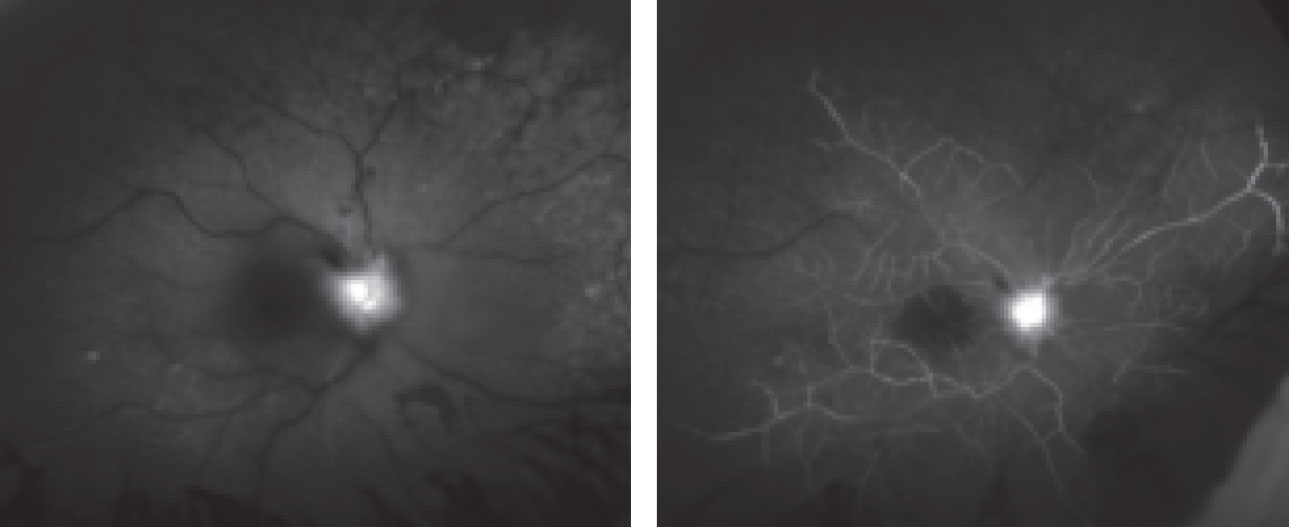 |
| Fig. 2. This fluorescein angiogram shows the patient’s right eye at 29 seconds (at left) and five minutes. |
Discussion
Central retinal artery occlusion (CRAO) is an ocular emergency whereby patients present with sudden, profound, painless monocular vision loss.1 In fact, 80% of affected individuals have a final visual acuity of counting fingers or worse.2
CRAO is classically described as a blockage of the central retinal artery responsible for supplying blood, nutrients and oxygen to the inner retinal layers of the eye. In the acute phase, 90% of CRAO cases will present with diffuse retinal whitening and a classic central cherry red spot.3 The cherry red spot is indicative of a thin and relatively transparent macula that reveals the underlying choroid.3 Additional signs of a CRAO include optic disc edema (in 22% of cases), optic disc pallor (39%) and arterial attenuation (32%).3 Unfortunately, this ischemic event causes irreversible retinal damage and profound vision loss with only mild visual recovery upon treatment.2
Diagnosis of this condition is prompted from sudden, painless vision loss coupled with the presence of diffuse retinal whitening and in most cases, a central cherry red spot.4 FA will show a delayed transit time followed by a patchy choroidal appearance and delayed arterial filling.5 This can be seen on the FA of our patient where even at 29 seconds you can see the fluorescein dye only beginning to fill the arteries (Figure 2). In a normal patient, this happens within 10 seconds.
Blockage of the central retinal artery may be caused by emboli, vasculitis or spasms.4 Major risk factors for a central retinal artery occlusion include hypertension, diabetes, hyperlipidemia, carotid occlusive disease and cardiac valve disease.4 Less common, but equally important, risk factors (especially when no emboli are present) include GCA, collagen vascular disease, oral contraceptive use, sickle cell disease and syphilis.4
CRAO can also be classified based on the presence and extent of retinal ischemia.6 Non-arteritic CRAO accounts for a majority of cases and is typically caused from atherosclerotic disease.6 Arteritic CRAO, on the other hand, is not as common and is defined based on a large area of retinal ischemia (typically more than 10 disc diameters).6 For the purposes of this case, direct examination supported by the FA findings confirmed arteritic CRAO of the right eye as the correct diagnosis.
The most common cause of arteritic CRAO is GCA, a systemic vasculitis that affects medium and large-sized blood vessels in adults 50 years and older.2 Systemic symptoms of GCA include fevers, temporal headaches, scalp tenderness, jaw claudication, temporary or sustained vision loss, problems with coordination, myalgias and difficulty swallowing.2 Ocular manifestations of GCA include retinal, choroidal and optic nerve edema/ischemia, diplopia, eye pain or symptoms of cranial neuropathies.2
A GCA diagnosis is based largely on symptoms and physical examination. Additional testing includes lab work-up and a temporal artery biopsy.2 Our patient underwent a temporal artery biopsy, which came back negative. This, however, cannot be solely used to confirm or deny the presence of GCA.
Conducting a medical work-up on patients suspected of having GCA is critical. Lab testing identifying inflammatory markers such as ESR, CRP and white blood cell counts, in conjunction with a temporal artery biopsy, becomes crucial for an accurate diagnosis of GCA. Elevated ESR and CRP levels are 97% specific for GCA.2 In fact, CRP levels above 2.5mg/L are highly diagnostic of GCA.2
Treatment and Management
CRAO is an ocular analog of a cerebral stroke.1 Immediate management is crucial to prevent further vision loss and systemic complications. Treatment options depend on the underlying cause of the CRAO and can include carbogen inhalation, acetazolamide infusion, ocular massage, anterior chamber paracentesis and various vasodilators.5
While such treatment can be attempted, none of these modalities definitively alter the natural history of the condition.6 In fact, patients who have experienced a CRAO are left with a guarded visual prognosis and minimal improvement in visual acuity from the initial encounter.4 An exception to the rule would be for those patients who have a cilioretinal artery supplying the macula as it allows for visual improvement to 20/50 or better in 80% of eyes.4
GCA-related CRAO is typically treated with a high dose of oral steroids (typically 60mg to 80mg) or intravenous steroids followed by a course of orals.2 While damage done by a GCA-related CRAO may not be reversible, aggressive treatment is needed to prevent further vision loss and protect the good eye from a subsequent ischemic attack.2
Our patient was treated with intravenous methylprednisolone followed by a course of 80mg of oral prednisolone, which is currently being slowly tapered. Patients with CRAO need to be evaluated on a monthly (if not sooner) basis for at least the first three months to check for potential neovascularization of the retina, iris or angle.7 The reported prevalence of neovascularization after an episode of CRAO varies from 2.5% to 31.6%.7 Such complications can cause further vision loss in the affected eye and possibly lead to neovascular glaucoma (i.e., the 90-day glaucoma).6
Dr. Jayasimha is an optometric resident at Bascom Palmer Eye Institute in Miami.
Retina Quiz Answers:
1) c; 2) c; 3) c; 4) c; 5) c.
1. Beatty S, Eong K. Acute occlusion of the retinal arteries: Current concepts and recent advances in diagnosis and management. J Accid Emerg Med. 2000;17(5):324-9. 2. Schmidt D, Schulte-Mönting J, Schumacher M. Prognosis of central retinal artery occlusion: local intraarterial fibrinolysis versus conservative treatment. 2002;23(8)1301-7. 3. Farris W, Waymack J. Central retinal artery occlusion. State Pearls. www.ncbi.nlm.nih.gov/books/NBK470354. October 27, 2018. Accessed November 15, 2018. 4. Weingeist T. Central Retinal Artery Occlusion (CRAO). Eye Rounds. webeye.ophth.uiowa.edu/eyeforum/atlas/pages/CRAO/index.htm. October 23, 2014. Accessed November 15, 2018. 5. Sim S, Ting D. Diagnosis and management of central retinal artery occlusion. EyeNet. www.aao.org/eyenet/article/diagnosis-and-management-of-crao. August 2017. Accessed November 15, 2018. 6. Varma D, Cugati S, Lee A, Chen C. A review of central retinal artery occlusion: Clinical presentation and management. Eye (Lond). 2013;27(6):688-97. 7. Chacko J, Chacko J, Salter M. Review of giant cell arteritis. Saudi J Ophthalmol. 2015 Jan-Mar;29(1):48-52. |

