Proliferative diabetic retinopathy (PDR) can occur without diabetic macular edema (DME). A recent study examined potential associations of demographic, medical, ophthalmologic and OCT characteristics with DME development and types of DME in patients with PDR. The findings were presented earlier this week at the 2021 ARVO virtual meeting by John O’Fee, a medical student of the Roski Eye Institute at the Keck School of Medicine of USC.
“Though DME and PDR commonly present together, they can present without one another, which is weird because they share VEGF as a common factor,” Mr. O’Fee said during the presentation. “Vitreous fluid in eyes with DME and/or PDR has significantly elevated VEGF levels. One would think then that eyes with just PDR are filled with VEGF in the vitreous, as are eyes with just DME. But for some unknown reason in these eyes, either PDR or DME don’t develop. There hasn’t been much reported in the literature on this apparent discrepancy, but one study found over 20% of eyes with PDR lacked DME.”
“We thought comparing PDR patients with and without DME may identify factors that advance our understanding of DME and its types in eyes with PDR,” he continued. “This may indicate potential improvements in treatment.”
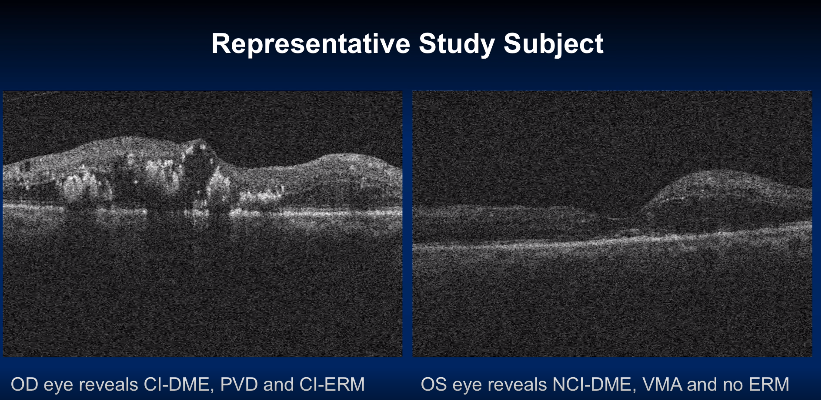
Mr. O’Fee and his colleagues conducted an observational, retrospective case series of PDR patients at retina clinics in an acute-care teaching hospital from December 2018 to October 2020. DME, vitreomacular interface (VMI) and epiretinal membrane (ERM) were measured by OCT and clinical documentation. They classified VMI status as vitreomacular adhesion without traction (VMA), vitreomacular traction (VMT) or macular posterior vitreous detachment (PVD).
They excluded eyes that had received previous retinal laser or intravitreal injection of a pharmacotherapeutic agent less than a year from the OCT date, eyes that had undergone previous intraocular surgery and eyes with comorbid ophthalmic disorders associated with DME.
A total of 293 eyes of 210 patients with PDR (66.2% DME, 33.8% no DME) met the inclusion criteria. “When comparing general characteristics, we observed that eyes with DME had significantly worse visual acuity,” Mr. O’Fee said. “We observed no significant differences in gender, age, diabetes duration, medication type, hemoglobin A1C levels and early, high-risk or previously untreated PDR.”
When comparing eyes with PDR with and without DME, the researchers found significant differences in average visual acuity, retinal thickness, cube volume and dialysis status. No significant differences in ERM and VMI status were found between the two groups.
 |
| Image courtesy of John O'Fee, ARVO 2021 |
The 90 eyes with center-involved DME (CI-DME) were significantly more likely to have PVD than non-CI-DME eyes. The researchers reported that CI-DME eyes had the following vitreomacular interface status: 44.4% with VMA, 7.8% with VMT and 47.8% with PVD. Eyes with non-CI-DME had the following VMI status: 67.3% with VMA, 1.0% with VMT and 31.7% with PVD.
They also reported 82.2% of CI-DME eyes had ERMs, and of these eyes, 44.9% had CI-ERM. CI-DME eyes were significantly more likely to have ERM and CI-ERM than non-CI-DME eyes.
“Our findings suggest ERM or other vitreomacular abnormalities perifoveally may contribute to CI-DME formation specifically, but not to DME in general,” Mr. O’Fee said. “Further prospective studies using standardized and multimodal imaging techniques may help to confirm this finding, provide additional insights into the relationship between PDR and DME.”
O’Fee J, Juliano J, Moshfeghi AA. Factors associated with diabetic macular edema development in patients with proliferative diabetic retinopathy. ARVO Meeting 2021. |

