 |
A 20-year-old white male presented with a sudden loss of vision in his left eye that occurred two days prior. He reported going to a college party on Friday night and waking up the next day with a dark spot that had a red tinge in the center of his vision.
His past ocular and medical histories were unremarkable.
On examination, his best-corrected visual acuity was 20/20 OD, 20/200 OS. Extraocular motility testing was normal. His confrontation visual fields were full-to-careful finger counting OU, and the pupils were equally round and reactive to light; there was no afferent pupillary defect. On Amsler grid testing, he had a central scotoma OS.
His anterior segment exam was unremarkable. Tensions by applanation measured 14mm Hg OU. On dilated fundus exam, the right eye was completely normal. In the left eye, there was a small cup with good rim coloration and perfusion. In the macula, there was a hemorrhage (Figures 1 and 2). The vessels and peripheral retinal were normal. We performed an OCT and OCT-A, which are available for review (Figures 3 and 4).
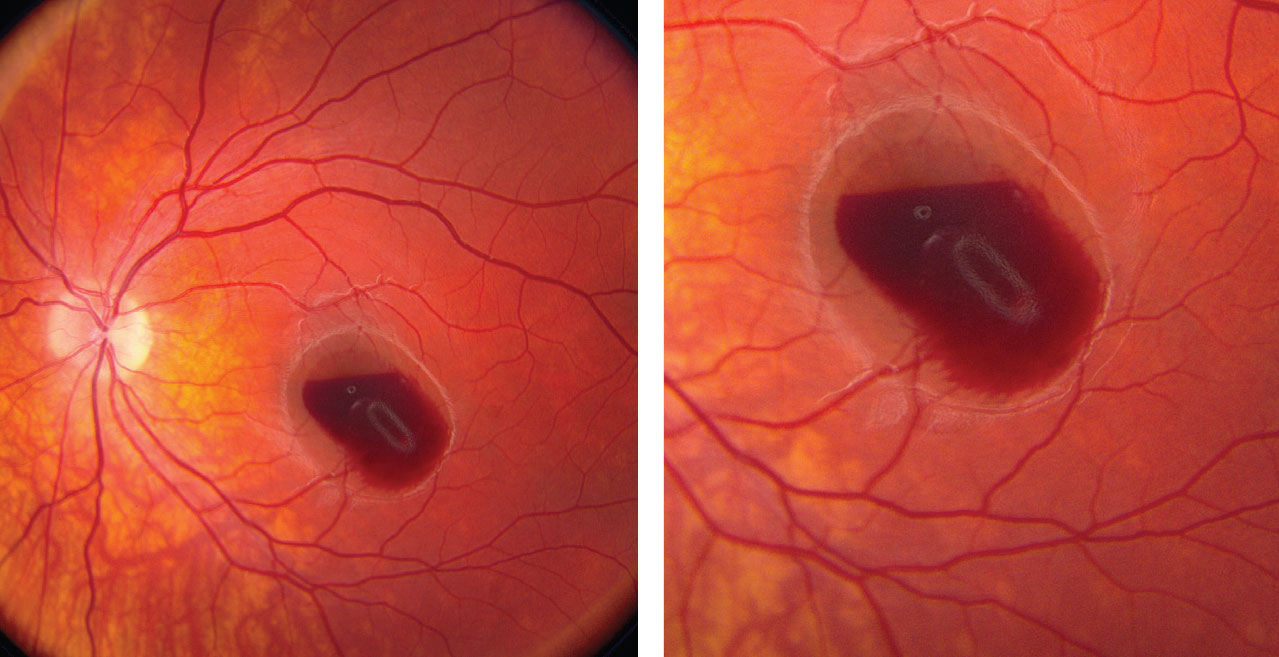 |
| Figs. 1 and 2. These fundus photos of the left eye show a retinal hemorrhage involving his macula. Where is the anatomic location of the blood? Click image to enlarge. |
Take the Retina Quiz
1. What is the correct diagnosis?
a. Idiopathic choroidal neovascularization (CNV).
b. Hemorrhagic central serous retinopathy.
c. Retinal arterial macroaneurysm (RAM).
d. Valsalva retinopathy.
2. Where is the blood located?
a. Subretinal space.
b. Between RPE and sensory retina.
c. Sub–internal limiting membrane (ILM).
d. Pre-retinal.
3. How should this patient be managed?
a. Observation.
b. Anti-VEGF injection.
c. YAG membranotomy.
d. Pars plana vitrectomy.
4. What is the long-term prognosis?
a. Excellent with treatment.
b. Excellent with close observation.
c. Good with continued anti-VEGF injections.
d. Likely will develop disciform scar formation.
For answers, see below.
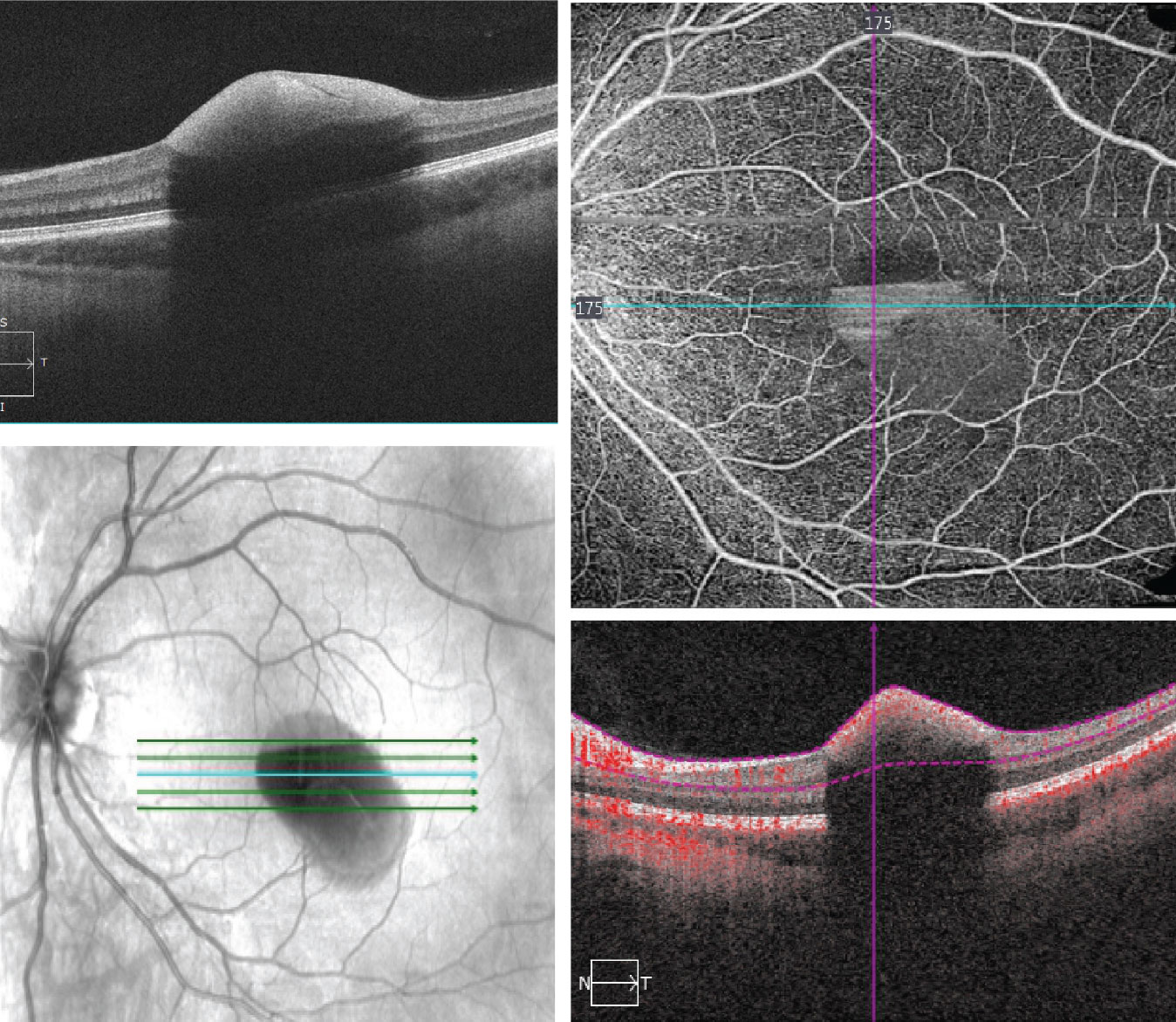 |
| Figs. 3 and 4. The SD-OCT (left) and OCT-A (right) of the left eye. The OCT-A is an 8mm x 8mm superficial cut through the macula. What does it show? Click image to enlarge. |
Diagnosis
Our patient has a classic presentation of Valsalva retinopathy. This condition is a rare retinopathy that is characterized by a preretinal hemorrhage in the macula due to the Valsalva maneuver. Valsalva occurs when a person tries to exhale air forcibly with a closed glottis (windpipe) so that no air goes out through the mouth or nose.
When this occurs, there is a sudden increase in intrathoracic or intra-abdominal pressure. This Valsalva maneuver occurs during various day-to-day activities that cause straining, such as coughing, sneezing, vomiting, exercise and blowing on musical instruments, among others.1
Discussion
In addition to the sudden increase in intrathoracic/intra-abdominal pressure, there is also raised central venous pressure in the head and neck. Because there are no valves in the venous system beyond the heart, the sudden rise in venous pressure leads to the rupture of perifoveal superficial retinal capillaries that cause the preretinal hemorrhage.
The exact anatomic location of the hemorrhage in our patient is not completely clear. On clinical exam, we know that the blood is anterior because it obscures the underlying retina and the top of the hemorrhage is flat or horizontal, almost having a boat shape. This is classic for a preretinal hemorrhage. However, to be even more specific, it’s difficult to know if the blood is under the ILM (sub-ILM) or between the posterior vitreous face and sensory retina. Even with SD-OCT it can be difficult to discern.2
In our patient, the posterior vitreous face appears intact, and, as you follow the OCT line scan, it is contiguous with the ILM. The blood appears posterior and indicates that it’s below the ILM.
The natural history of Valsalva retinopathy is good, as the vast majority of patients make a complete return to normal vision after the blood resolves. However, this can be a slow process that can take up to several months. One treatment option becoming more common is Nd:YAG laser membranotomy. During this, the laser makes an opening in the posterior hyaloid or ILM so the blood can escape into the vitreous, settling inferiorly and clearing the visual axis.3 In some instances subretinal or vitreous hemorrhage can occur necessitating surgical intervention. Pars plana vitrectomy may be indicated for patients with significant retinal hemorrhages or dense vitreous hemorrhage.4
Even though the clinical presentation for our patient is classic for Valsalva retinopathy, his history is not. When we tried to elicit a history of performing any strenuous activities that could result in Valsalva maneuver, he didn’t recall any. Even though he had been to a party the night before, he didn’t vomit or remember having any kind of hard cough or sneeze. We also questioned him about engaging in vigorous sexual activity, as Valsalva retinopathy has also been reported during orgasm.5 He denied this as well.
We elected to follow-up our patient to determine if the hemorrhage would spontaneously resolve. At the follow-up visit a month later, he was still 20/200. Even though the hemorrhage was smaller, there was still significant involvement in his macula. As he was getting anxious that vision was not getting better, we scheduled him back in one month with a retina specialist for consideration of Nd:YAG membranotomy.
Retina Quiz Answers
1) d; 2) c; 3) a; 4) b.
| 1. Duane TD. Valsalva hemorrhagic retinopathy. Trans Am Ophthalmol Soc. 1972;70:298-313. 2. Goel N, Kumar V, Seth A, et al. Spectral-domain optical coherence tomography findings of subinternal limiting membrane hemorrhage in the macula before and after Nd:YAG laser treatment. Ophthalmic Surg Lasers Imaging Retina. 2011;42(3):222-8. 3. Durukan AH, Kerimoglu H, Erdurman C, et al. Long-term results of Nd:YAG laser treatment for premacular subhyaloid haemorrhage owing to Valsalva retinopathy. Eye (Lond). 2008;22(2):214-8. 4. Khadka , Bhandari S, Bajimaya S, et al. Nd:YAG laser hyaloidotomy in the management of Premacular Subhyaloid Hemorrhage. BMC Ophthalmol. 2016;16:41. 5. Michaels L, et al. Postcoital visual loss due to valsalva retinopathy BMJ Case. Rep 2014;2014:bcr-2014-207130. |

