 |
A 27-year-old male presented to the clinic after being referred for management of his markedly elevated intraocular pressure (IOP). His past ocular history was significant for ocular trauma to his left eye that left him with poor vision. He had never been diagnosed with glaucoma before.
His best-corrected acuities were 20/20 OD and 20/400 OS due to a traumatic macular scar, choroidal rupture and fibrotic parapapillary traction. His anterior chamber angles were gonioscopically open to the ciliary body OU, without abnormalities. He had large optic discs with a cup-to-disc ratio of 0.7/0.7 with smooth and regular neuroretinal rims and no focal damage, parapapillary atrophy, disc hemorrhages or retinal nerve fiber layer (RNFL) defects.
His central corneal thicknesses were 557µm OD and 560µm OS. Optical coherence tomography (OCT) showed a normal RNFL in the right eye and abnormal measurements in the left, due to maculopathy. Threshold perimetry was normal OD and unreliable OS. Except for pre-existing traumatic maculopathy, he had no abnormalities or damage attributable to glaucoma. His IOPs, however, were quite remarkable at 51mm Hg OD and 55mm Hg OS. He was subsequently diagnosed with an extreme degree of ocular hypertension (OHTN). Clearly, the patient was not the prototypical ocular hypertension case.
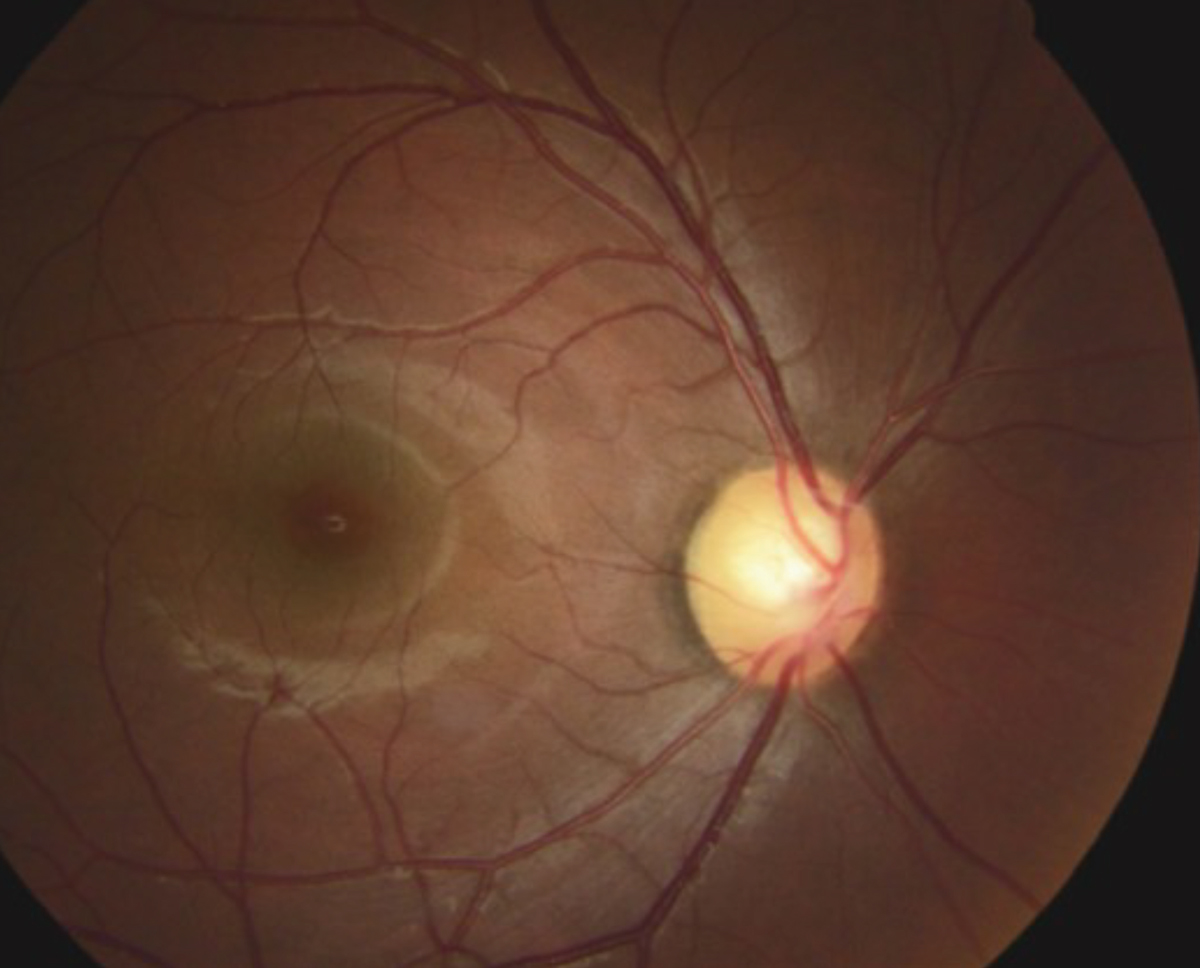 |
This fundus photo shows our 27-year-old patient’s right eye. He has a large, healthy optic nerve despite an intraocular pressure of 51mm Hg. Click image to enlarge. |
Risk of Progression
OHTN—classically thought of as IOP above a statistically normal level of 21mm Hg in the absence of glaucomatous damage to the optic disc, retinal nerve fiber layer (RNFL) or visual field—is one of the most common clinical entities encountered. While diagnosis can be straightforward, management is more challenging, especially when other variables come into play. Patient age, comorbidities, level of IOP and other factors make this common condition a sometimes-complicated management issue.
Historically, OHTN was seen as a relatively benign condition that could predispose patients to the development of primary open-angle glaucoma (POAG). However, no scientific assessment of the probability of converting to POAG existed and doctors had no data on the whether it was useful to prophylactically lower IOP. Anecdotally, clinicians who had extensive clinical experience with glaucoma and OHTN patients generally felt that, without treatment, approximately 10% of OHTN patients would develop glaucoma, but that was just a rule of thumb. Researchers had no consensus on how best to manage OHTN. Some doctors chose to merely observe while others treated.
Then, in 2002, the Ocular Hypertension Treatment Study (OHTS) was published. The main focus of that research was to determine if reducing IOP delayed or prevented the development of glaucoma in eyes with OHTN.1 What the investigators found was that, prophylactically lowering IOP in eyes with OHTN reduced the risk of progression over the initial five years of the study.
At 60 months, the cumulative probability of developing POAG was 4.4% among the prophylactically medicated subjects, while it was 9.5% in the observation group.1 That nicely validated our previous rule of thumb that approximately 10% of OHTN patients convert to glaucoma. Although IOP reduction imparted about a 60% reduced risk of conversion to glaucoma, the study results did not imply that all patients with borderline or elevated IOP should receive medication, but that clinicians should consider initiating treatment for individuals with OHTN who are at moderate or high risk for developing POAG.1
Subsequent analysis of that data attempted to identify patients who would be a greater risk of converting to glaucoma. It found that older baseline age, larger vertical and horizontal cup-disc ratio, greater visual field pattern standard deviation values, and greater IOP levels were good predictors for the onset of POAG in the OHTS.2 The research also shows lower central corneal thickness (CCT) is a powerful POAG predictor.2
A European study of OHTN found similar results and the pooled data from these two studies have led to the development of risk calculators to estimate the five-year risk of developing POAG and are useful for clinicians and patients in guiding management plans.2-4 Most experienced glaucoma clinicians recommend treatment when the calculated risk of glaucoma conversion exceeds 15% for longer than five years.
After a median of 7.5 years without treatment, the original OHTS observation group received medication for a median of 5.5 years to determine any problems from delaying treatment. At a median follow-up of 13 years, researchers saw little absolute benefit of early treatment in individuals with OHTN at low risk of developing POAG.5,6 Clinicians need to consider the patient’s age, health status, life expectancy and personal preferences when making treatment decisions.5,6
Balancing Parameters
While we have learned a great deal from OHTS, the information provides only general guidelines and leaves many questions unanswered. Thanks to this research, clinicians now have risk calculators that can help assess the five-year risk of conversion from OHTN to POAG readily available online.7,8
However, these risk calculators must be used accurately. They are only useful for patients with OHTN (and not pre-existing glaucoma) within a specific IOP range (22mm Hg to 32mm Hg). The calculators have not been validated in patients younger than 30 years or older than 80 years. Secondary conditions causing IOP elevation, such as pigment dispersion, exfoliation or uveitis are not part of the assessment. Furthermore, accurate data in terms of several IOP measurements, CCT and visual field parameters need to be entered, which can be time consuming. Deviating from these parameters makes the calculated risk dubious at best.
Practitioners often wonder about a “magic number”— an IOP measurement above which treatment should always be initiated. No such concept has any scientific validity. Most experienced glaucoma practitioners have differing opinions and trying to standardize treatment in this manner independent of CCT, age, optic disc appearance, systemic health and numerous other factors oversimplifies OHTN and may put patients at risk of under- or overtreatment.
For those who demand a “magic number,” look to the design of OHTS.9 Eligibility required that IOP be less than 32mm Hg. Patients with IOP at or above 32mm Hg were excluded, not for any scientific reason, but likely due to the designers’ discomfort at possibly randomizing eyes with this IOP level to observation. Hence, for those who demand an absolute number, OHTS indicated 32mm Hg to be the peak.9
 |
| Ocular hypertension patients usually have visual fields with normal sensitivity and variability only slightly higher than in normal subjects. Click image to enlarge. |
Targeting Treatment
Old wisdom suggests that doctors should treat elevated IOP if for no other reason than to prevent a retinal vascular occlusion (RVO). This practice goes against much of what we learned from the OHTS regarding lowering IOP in ocular hypertensive eyes to prevent glaucoma formation. Do we really want to lower IOP in every ocular hypertensive eye due to fear of RVO?
The most definitive answer to the question of prophylaxis against RVO comes from a subsequent publication from OHTS. In this subanalysis, researchers noted that 26 RVOs occurred in 23 participants (15 in the observation group and eight in the medication group).10 They saw that the 10-year cumulative incidence of RVO was 2.1% in the observation group with untreated ocular hypertension and 1.4% in the medication group.10 Although the incidence of RVO was higher in the observation group than the medication group, this difference was not statistically significant.10
Based upon this evidence, we cannot justify recommending that ocular hypertension be treated to protect against RVO. In fact, the 10-year incidence of RVO in ocular hypertensive eyes is actually low.10 RVO often occurs concurrent with OHTN and POAG because they are comorbidities affecting elderly patients with vascular diseases. I have encountered many patients with IOP ranging from 50mm Hg to greater than 70mm Hg at time of diagnosis and not once saw a concurrent RVO in any eye. In patients for whom I have seen POAG and RVO concurrently, they have almost been exclusively in eyes with well-treated IOP levels. As such, I don’t consider the fear of RVO in my OHTN decision-making.
In the patient described here, very little guidance from controlled studies helps dictate his management. His young age and markedly elevated IOP exceeded ranges from any study on OHTN. Despite IOP in the 50s, his optics discs, RNFL and visual field were still normal. After a discussion of the risks, benefits and the unusual nature of his condition, he was prescribed a topical prostaglandin analog which lowered his IOP to 20mm Hg OD and 18mm Hg OS and he is currently being followed at appropriate intervals.
1. Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701-13. 2. Gordon MO, Beiser JA, Brandt JD, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):714-20. 3. Miglior S, Pfeiffer N, Torri V, et al. European Glaucoma Prevention Study (EGPS) Group. Predictive factors for open-angle glaucoma among patients with ocular hypertension in the European Glaucoma Prevention Study. Ophthalmology. 2007 Jan;114(1):3-9. 4. Ocular Hypertension Treatment Study Group; European Glaucoma Prevention Study Group, Gordon MO, Torri V, Miglior S, Beiser et al. Validated prediction model for the development of primary open-angle glaucoma in individuals with ocular hypertension. Ophthalmology. 2007;114(1):10-19. 5. Kass MA, Gordon MO, Gao F, et al. Ocular Hypertension Treatment Study Group. Delaying treatment of ocular hypertension: the ocular hypertension treatment study. Arch Ophthalmol. 2010 Mar;128(3):276-87. 6. Gordon MO, Kass MA. What we have learned from the ocular hypertension treatment study. Am J Ophthalmol. 2018 May;189:24-7. 7. Kass M. Ocular Hypertension Treatment Study (OHTS) Calculator. MD+CALC www.mdcalc.com/ocular-hypertension-treatment-study-ohts-calculator. Accessed June 10, 2020. 8. Ocular Hypertension Treatment Study. Risk Calculator. ohts.wustl.edu/risk/ as examples. Washington University School of Medicine in St. Louis. 2006. Accessed June 10, 2020. 9. Gordon MO, Kass MA. The Ocular Hypertension Treatment Study: design and baseline description of the participants. Arch Ophthalmol. 1999 May;117(5):573-83. 10. Barnett EM, Fantin A, Wilson BS, et al. The incidence of retinal vein occlusion in the Ocular Hypertension Treatment Study. Ophthalmol. 2010;117(3):484-8. |

