 |
An 81-year-old man presented with a new “fish-shaped” gray floater in his left eye that had been a constant for the last three days. He reported that reading had become difficult. However, his visual acuity was 20/20 OS, and he had no other visual symptoms, eye pain, photopsia or headache. Notably, the patient specified that the floater was stationary relative to fixation and did not move with eye movement as his other floaters did.
The patient’s medical history was positive for thyroid disease, hypertension, prostate cancer, anemia and rheumatoid arthritis. His ocular history consisted of intermediate-stage dry age-related macular degeneration, pigment dispersion syndrome, posterior vitreous detachment and pseudophakia.
 |
|
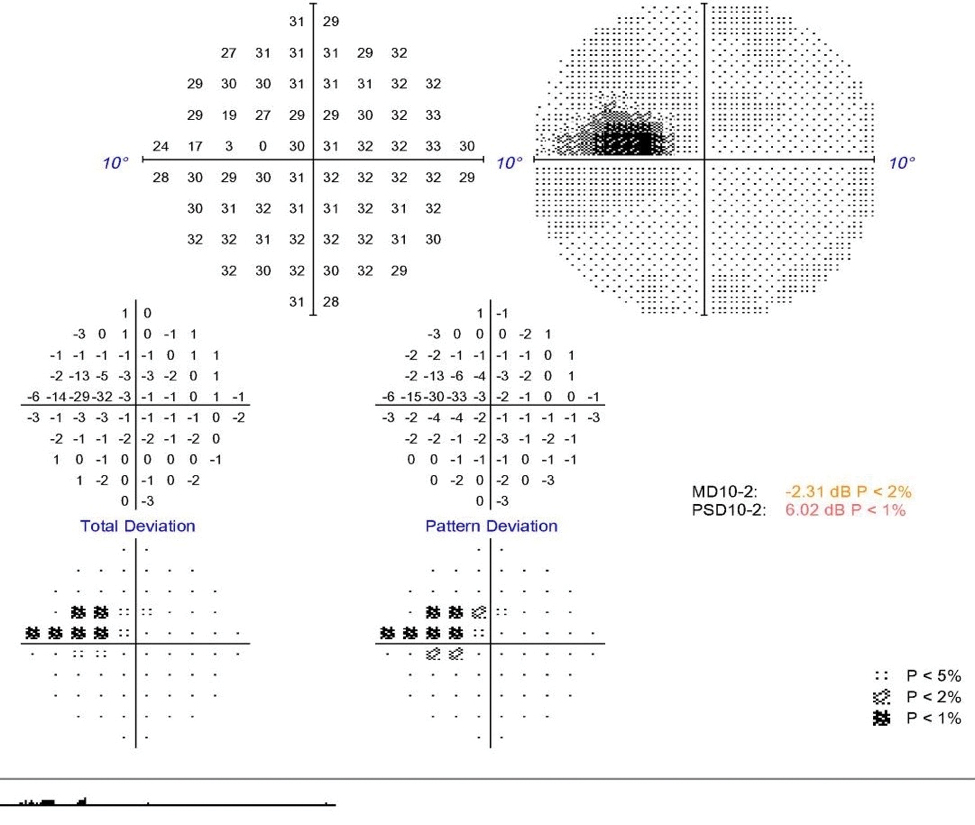
This 10-2 visual field displays our patient’s paracentral scotoma. Click image to enlarge. |
The anterior segment was within normal limits, and intraocular pressures and pupillary responses were normal. On dilated examination, there were no retinal breaks, hemorrhages or optic nerve abnormalities. The macula had a small demarcated area of retinal whitening just off the optic nerve, which corresponded with inner retinal thickening on OCT. A 10-2 Humphrey visual field showed the fish-shaped floater that had brought this patient in to seek help.
Case Discussion
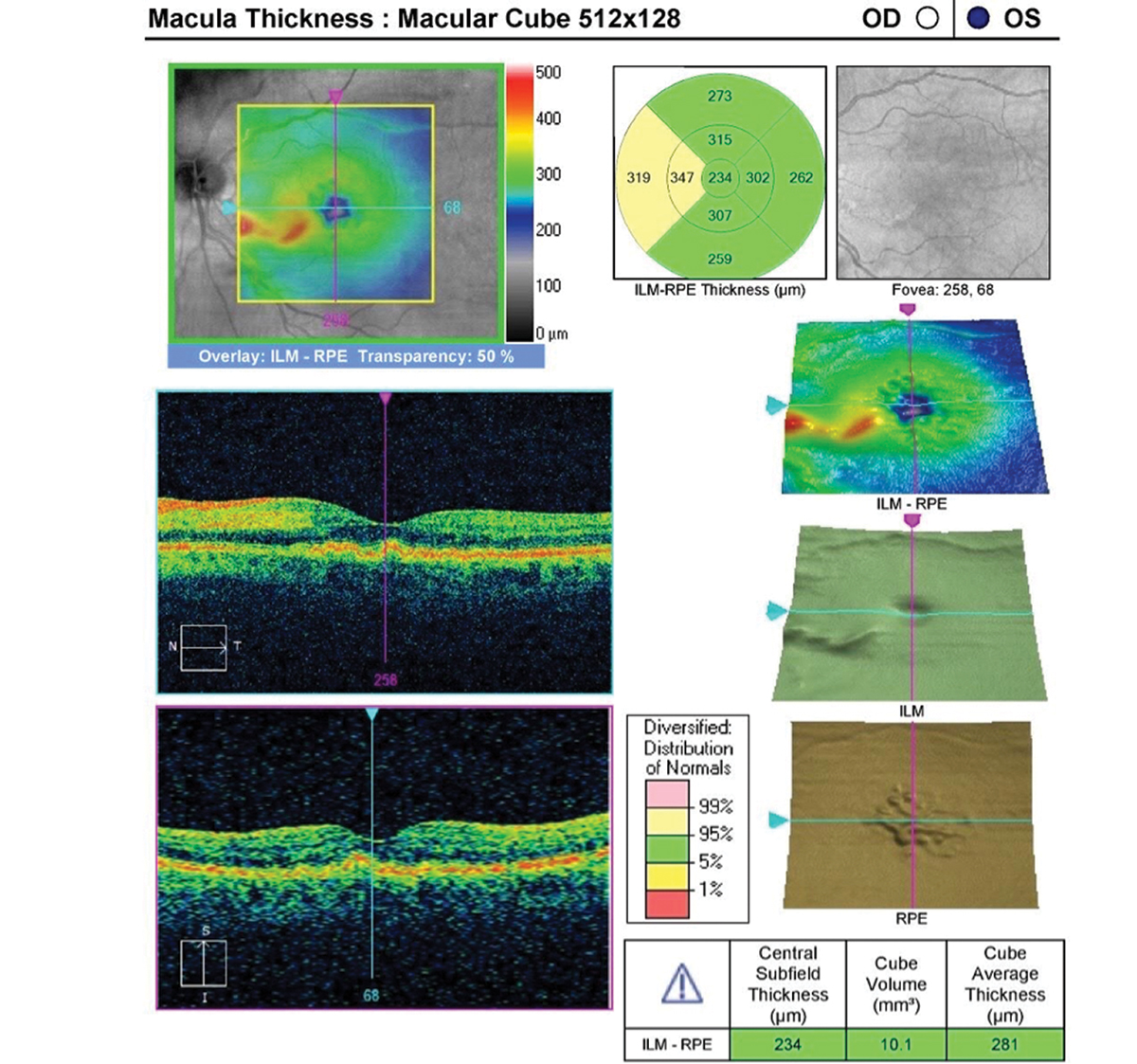
The OCT findings were consistent with nerve fiber layer ischemia and the classic pattern of inner retinal edema with mild outer retinal shadowing seen in acute retinal artery occlusions. Given the shape and location of ischemia, the patient was diagnosed with a cilioretinal artery occlusion (CLRAO).
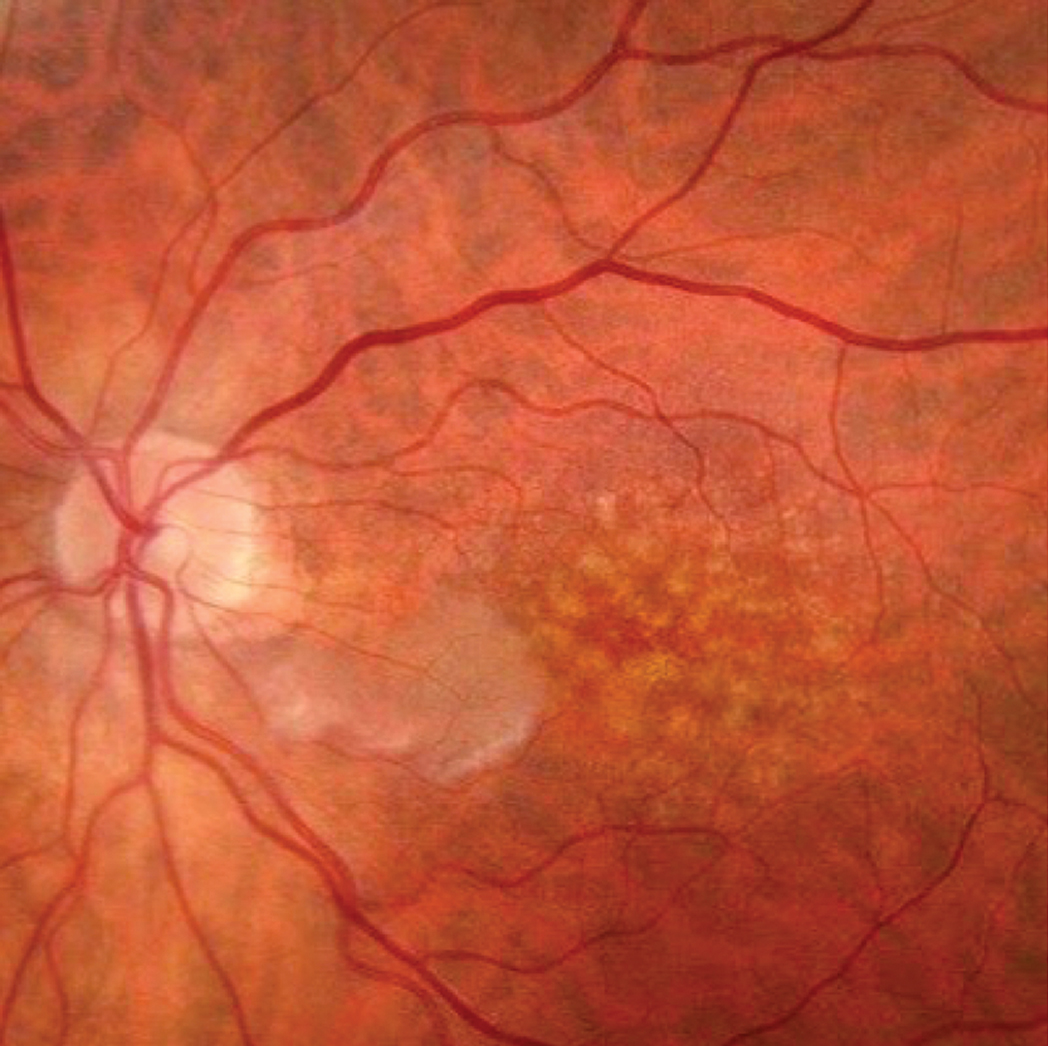 |
| Fundus photography of the retinal whitening corresponds with the cilioretinal artery. Click image to enlarge. |
The cilioretinal artery is only present in approximately one in three people and provides a secondary blood supply to the inner layers of the macula.1 CLRAO comprises only 5.3% to 7.1% of all retinal artery occlusions.1 It has been associated with embolism, lupus, antiphospholipid syndrome, sildenafil, pregnancy and systemic hypertension.2 CLRAO can present in three ways: with ischemic optic neuropathy in giant cell arteritis (GCA), with concomitant central retinal vein occlusion (CRVO) or in isolation. It is important to distinguish which of these scenarios is at play, as the etiology will guide the treatment process and visual prognosis.
If there is reason to believe GCA is at the heart of the problem, either from associated symptomatology or clinical optic nerve appearance, it is critical to arrange for same-day erythrocyte sedimentation rate and C-reactive protein testing and intravenous steroid treatment. The inflammatory vasculitis of GCA has a predilection for medium-sized arteries like the ophthalmic artery, of which the cilioretinal artery is a branch. This disrupts the blood supply to both the ciliary circulation and the central retinal artery, which is why CLRAO usually occurs in conjunction with a central retinal artery occlusion and/or anterior ischemic optic neuropathy. The lack of redundant circulation is why GCA-associated CLRAO has the worst prognosis and, if not treated in a timely manner, could result in severe bilateral vision loss.
When CLRAO is associated with a CRVO, there is a better prognosis, as the vein occlusion tends to be non-ischemic. The exact etiology as to why these conditions sometimes occur simultaneously is unclear, and the incidence may be underreported.3 The most widely accepted theory is that the initial CRVO raises the pressure in the capillary bed, causing hemodynamic block and a subsequent CLRAO.4 Supporting this hemodynamic theory are reports that emboli are rarely, if ever, identified in eyes with concomitant CRVO and CLRAO.5 Treatment focuses on the presence of macular edema and neovascularization in cases of isolated CRVO.
 |
|
Note the warmer colors on this macular OCT, indicating edema in the corresponding area. On the B-scan, you can see the hyperreflectivity of the edematous inner retinal layers. Click image to enlarge. |
The third subtype has the best visual prognosis and can be seen in this patient. Isolated CLRAOs tend to be embolic in nature; therefore, treatment aims to dislodge the embolus and restore blood flow to the retina as soon as possible. Treatments include ocular massage, paracentesis and intra-arterial thrombolysis.6 Perhaps most promising is hyperbaric oxygen treatment, the goal of which is to increase oxygen levels in the choroidal circulation to allow for diffusion into the inner layers until sporadic recanalization occurs, usually within the first 72 hours.7
This approach has shown significant improvement in subjective vision compared with observation and has a more favorable safety profile compared with thrombolysis.8 Irreversible retinal damage is known to occur after four hours of CLRAO in animal models, though this may not directly translate to clinical practice given the multiple variables of acuteness of onset, degree of occlusion and patient-specific factors regarding perfusion pressure required to avoid permanent injury.7,9 A widely accepted rule of thumb is that hyperbaric oxygen treatment should be performed within 24 hours of symptom onset.10
 |
|
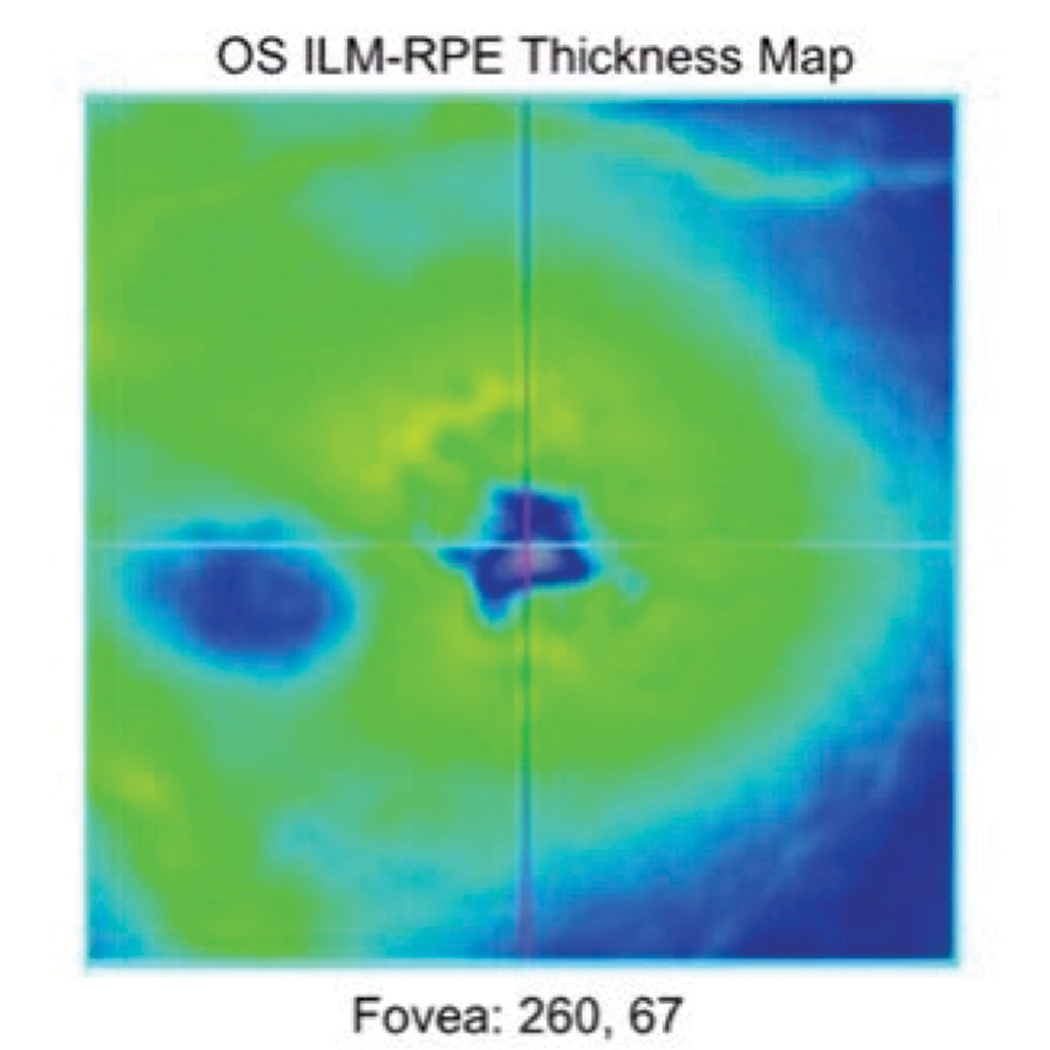
Repeat OCT was taken two months after the patient first presented, and you can see the area of thickening has now thinned due to atrophy. Click image to enlarge. |
Case Wrap-up
Fortunately, this patient had excellent presenting acuity, even though it was too late for hyperbaric oxygen treatment. After confirming there was no GCA or concomitant vein occlusion, the patient’s case was deemed likely to be embolic and isolated in nature.
The patient was already being treated for systemic hypertension and on a daily aspirin regimen. It was recommended he follow-up that same day at the hospital for a full stroke evaluation, as up to 31% of patients with acute retinal artery occlusion may have concurrent cerebral infarction.11
Upon following up for an additional workup, imaging did not detect cerebral ischemia, but the MRI did incidentally reveal a pituitary tumor. The patient was kept overnight for observation, started on atorvastatin and scheduled for a follow-up with neurosurgery. The visual field defect persisted, but his vision remained 20/20 and the scotoma was not as bothersome.
Dr. Hammond is a consultative medical optometrist at North Suburban Eye Specialists in Minneapolis. He has no financial interests to disclose.
Dr. Mangan is a board-certified consultative optometrist from Boulder, CO, and a fellow of the American Academy of Optometry. He is an assistant professor in the department of ophthalmology at the University of Colorado School of Medicine. His focus is on ocular disease and surgical comanagement. He has no financial interests to disclose.
1. Hayreh SS. Acute retinal arterial occlusive disorders. Prog Retin Eye Res. 2011;30(5):359-94. 2. Christodoulou P, Katsimpris I. Optical coherence tomography findings in a case of cilioretinal artery occlusion reversal, treated with mannitol and carbogen administration. Ann Eye Sci. 2019;4:13. 3. Messner LV, Newman TL, Bartlett M, et al. Cilioretinal artery occlusion with central retinal vein occlusion. Optom Vis Sci. 1999;76(11):741-6. 4. Grzybowski A, Elikowski W, Gaca-Wysocka M. Cardiovascular risk factors in patients with combined central retinal vein occlusion and cilioretinal artery occlusion. Medicine (Baltimore). 2018;97(1):e9255. 5. Schmidt D. Comorbidities in combined retinal artery and vein occlusions. Eur J Med Res. 2013;18(1):27. 6. Varma DD, Cugati S, Lee AW, et al. A review of central retinal artery occlusion: clinical presentation and management. Eye (Lond). 2013;27(6):688-97. 7. Aktaş S, Uyar OM, Özer E, et al. Idiopathic isolated cilioretinal artery occlusion treated with hyperbaric oxygen therapy. Turk J Op thalmol. 2016;46(5):244-7. 8. Schumacher M, Schmidt D, Jurklies B, et al. Central retinal artery occlusion: local intra-arterial fibrinolysis versus conservative treatment, a multicenter randomized trial. Ophthalmology. 2010;117(7):1367-75. 9. Hayreh SS, Zimmerman MB, Kimura A, et al. Central retinal artery occlusion. Retinal survival time. Exp Eye Res. 2004;78(3):723-36. 10. Murphy-Lavoie H, Butler F, Hagan C. Central retinal artery occlusion treated with oxygen: a literature review and treatment algorithm. Undersea Hyperb Med. 2012;39(5):943-53. 11. Biousse V, Nahab F, Newman NJ. Management of acute retinal ischemia: follow the guidelines. Ophthalmology. 2018;125(10):1597-1607. |

