 |
Anterior Complications
The most common ocular complication is parinaud oculoglandular conjunctivitis, presenting with unilateral conjunctival redness, foreign body sensation, serous or purulent discharge and one or more granulomatous nodules on the conjunctiva. These ocular signs occur in addition to an ipsilateral swollen preauricular, submandibular or cervical lymph node.4 Antibiotic treatment in these presentations is considered optional, as it is typically self-limited and resolves in two to six weeks.1,3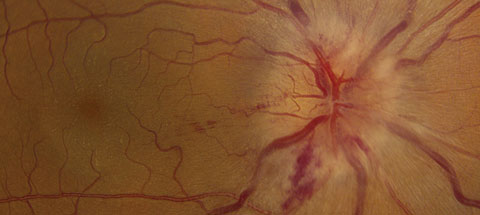 |
| This patient displays optic nerve swelling and a neurosensory retinal detachment in the right eye. If you look closely at the macula, you’ll see exudate in a “macular star” pattern. This presentation most likely represents a neuroretinitis caused by Bartonella henselae, or cat-scratch disease. Click image to enlarge. |
Posterior Complications
CSD affecting the posterior segment, however, is a different story. Cat-scratch neuroretinitis is considered an atypical, serious presentation of CSD and occurs in approximately 1% to 2% of cases.3,5 Although rare, cat scratch neuroretinitis is the most common form of infectious neuroretinitis.6 One study found that Bartonella henselae is the most common cause of neuroretinitis with 64.3% of tested patients with neuroretinitis having positive serological analysis for Bartonella henselae.7 Presenting symptoms of cat scratch neuroretinitis include acute central vision loss (88%), which is typically unilateral, with the associated systemic complaints discussed above.6 Vision loss is typically painless; however, eye pain has been reported to occur in about 8% of cases.6 Color vision changes, including red desaturation, may be present on examination.Inflammation of the posterior segment can indicate a potential case of CSD. The classical description of neuroretinitis is optic disc edema with the presence of a macular star (ODEMS). The macular exudates are a result of serous leakage and may not be present on initial examination. These findings often resolve to 20/40 or better central vision.6 More site-threatening complications of CSD include retinal vasculitis and vascular occlusions. A relative afferent pupillary defect may be noted in unilateral cases. A serous retinal detachment or vitritis, or both, may also be present.1 Discrete, white chorioretinal lesions have recently been a more common posterior segment finding related to CSD.1 Performing an OCT can be useful in confirming or ruling out subtle amounts of intraretinal fluid or a mild/early serous detachment.
Diagnosis Pearls
Apart from the urgency of treating moderate-to-severe CSD, consider the often-urgent differentials. Other conditions known to cause posterior uveitis and retinitis such as lyme disease, sarcoidosis, syphilis, and toxoplasmosis should be considered. Malignant hypertension and diabetic papillopathy must also be ruled out as both conditions can cause ODEMS. Optic nerve edema also necessitates consideration of intraocular mass, increased intracranial pressure and viral infections. Rare cases of bilateral CSD can mimic pseudotumor cerebri.1 CSD can also appear clinically similar to Vogt-Koyanagi-Harada syndrome.1,2,6In cases of possible CSD, an important step in diagnosis is asking for known history of exposure to kittens or cats. Although patients will typically report close contact with a cat, cases have been reported where no history of contact with a cat have been reported.10 CSD should always be considered when a child presents with neuroretinitis. If CSD is suspected, serology testing can be performed for IgM and IgG antibodies. Initial negative serology testing does not rule out CSD and can be repeated even after treatment is initiated.8 One group of researchers showed an MRI localizing enhancement to the optic nerve-globe junction has much higher reliability than serology testing.8,9 A biopsy of the affected lymph node can also yield Bartonella bacillus for diagnosis. Typically, treatment is initiated based on clinical signs and a positive history of exposure.
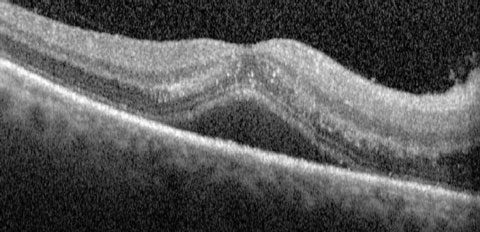 |
| This OCT scan shows the same eye as the previous image. An OCT scan can help detect intraretinal fluid of early serous detachment in CSD patients. |
Treatments
As previously mentioned, CSD is typically self-limiting; however, most ocular findings in CSD are indicative of a moderate-to-severe infection. In these cases, antibiotic treatment is recommended. Controlled, prospective studies of treatment in ocular manifestations of CSD are lacking in the literature; however, one group did publish recommendations in 2004.3 They emphasized the marked difference in immunocompromised versus immunocompetent patients’ improvement with antibiotic therapy. In the absence of posterior segment disease, the authors felt that antibiotic therapy in otherwise healthy patients was not strongly recommended. Immunocompetent patients with retinitis appeared to improve with doxycycline or rifampin treatments, or both.1,3,6 Ciprofloxacin has also been suggested as a treatment in adults who are not pregnant.6 Azithromycin displayed a faster resolution of lymphadenopathy than no treatment; however, doxycycline demonstrates better penetration of intraocular tissues. Investigators suggest erythromycin for pediatric patients.1,3Researchers also found that a four-to-six week course of oral doxycycline (100mg BID) and rifampin (300g BID-TID) promoted resolution of Bartonella henselae neuroretinitis, in addition to the systemic infection.11 They found that once antibiotic therapy was initiated, no further progression of ocular inflammation was noted and disc swelling was reduced within a few days.11 The study concluded that visual recovery was most rapid if the time between symptom onset and initiation of antibiotic therapy was minimized.11 It is for the above reasons that it is so important to recognize the signs and symptoms of cat scratch neuroretinitis and initiate treatment promptly.
The decision to initiate treatment may be made clinically or in consultation with the patient’s primary care provider. As discussed, moderate-to-severe CSD poses risks of systemic dissemination, encephalopathy, and liver, spleen and heart complications.
After the successful diagnoses and treatment of cat-scratch neuroretinitis, it is vital encourage patients who have been diagnosed with cat-scratch neuroretinitis to be monitored long term for signs of late onset optic-neuropathy.11
Dr. Stout is a clinical instructor at the University of Waterloo School of Optometry and Vision Science.
Dr. Harsch is in practice at Nittany Eye Associates in State College, PA.
|
1. Wang, Robert C. Cat Scratch and Whipple’s Disease. In: Yanoff M, Duker JS, ed. Ophthalmology, 4th edition. Elsevier Health Sciences; 2014. 720-22. ClincalKey. 2. Palau A, Mogan M, Yalamanchili S, Lee A. Neuro-ophthalmic annual review. Asia-Pacific J of Ophthal. 2014;3(2):104-25. 3. Rolain JM, Brouqui P, Koehler JE, et al. Recommendations for treatment of human infections of Bartonella species. Antimicrob Agents Chemother. 2004;48(6):1921-33. 4. Cunningham ET, Koehler JE. Ocular bartonellosis. Am J Ophthalmol. 2000;130(3):340-9. 5. Ormerod LD, Dailey JP. Ocular manifestations of cat-scratch disease. Curr Opin Opthalmol. 1999;10:209-16 6. Purvin V, Sundaram S, Kawasaki A. Neuroretinitis: Review of the literature and new observations. J of Neuro-Ophthal. 2011;31(1):58-68. 7. Suhler E, Lauer A, Rosenbaum J. Prevalence of serologic evidence of cat scratch disease in patients with neuroretinitis. Ophthalmology. 2000;107(5):871-6. 8. Gulati A, Yalamchanchi S, Golnik K, Andrew G. Cat scratch neuroretinitis: The role of acute and convalescent titers for diagnosis. J of Neuro-Ophthal. 2012;32(3):243-5. 9. Schmalfuss I, Dean CW, Sistrom C, Bhatti MT. Optic neuropathy secondary to cat scratch disease: distinguishing MR imaging features from other types of optic neuropathies. Am J of Neuroradiol. 2005;26(6):1310-6. 10. Blattner, RJ. Cat-scratch disease without cat contact. J Pediatr. 1963;63:676-8. 11. Reed J, Scales D, Wong M, et al. Bartonella henselae neuroretinitis in cat scratch disease: diagnosis, management, and sequelae. Ophthalmology. 1998;105:459-66.1. |

