 |
A 34-year-old black female presented for an annual eye exam as part of her vision plan insurance. She had not had her eyes tested in several years and said she began noticing eye fatigue after prolonged computer use. She does not wear glasses, reports being in good health and says she does not take any medications.
On examination, her entering visual acuities were 20/20 in each eye. Confrontation visual fields were full-to-careful-finger-counting in both eyes. Her pupils were equally round and reactive; there was no afferent defect. Extraocular motility testing was normal. The anterior segment examination of both eyes was unremarkable. Tensions by applanation tonometry measured 16 OU.
On dilated fundus exam, the vitreous was clear. Fundus images were taken of her optic nerves (Figure 1). The macula, vessels and periphery were normal. Spectral domain optical coherence tomography (SD-OCT) are available for review (Figure 2).
 |
| Fig. 1. These fundus images show the right (at top) and left optic nerves of our 34-year-old patient. What can they tell you about her likely diagnosis? Click image to enlarge. |
Take the Retina Quiz
1. How would you characterize the optic nerves?
a. Elevated but no swelling.
b. Lumpy/bumpy.
c. Grade II disc swelling.
d. Grade III disc swelling.
2. What additional testing may be necessary?
a. No additional testing.
b. MRI.
c. LP.
d. Both B and C.
3. Based on the clinical findings, what is the likely diagnosis?
a. Optic nerve head drusen.
b. Papilledema.
c. Optic nerve hypoplasia.
d. Idiopathic intracranial hypertension.
4. How should this patient be managed?
a. Only observation.
b. Weight loss.
c. Periodic visual fields.
d. Acetazolamide.
For answers, see below.
Table 1. Optic Nerve Swelling Grading ClassificationsGrade I: papilledema is characterized by a C-shaped halo with a temporal gap. Grade II: papilledema, the halo becomes circumferential. Grade III: papilledema is characterized by loss of major vessels as they leave the disc Grade IV: papilledema is characterized by loss of major vessels on the disc. Grade V: papilledema has the criteria of grade IV plus partial or total obscuration of all vessels of the disc. |
Diagnosis
Our patient had very obvious bilateral optic nerve swelling in both eyes. On clinical exam, the optic nerves were clearly elevated, the margins were blurred 360 degrees and there was an absence of a spontaneous venous pulse in both eyes. Based on the modified Frisén classification of disc swelling, our patient had grade III disc swelling. The SD-OCT also showed obvious RNFL thickening beyond what is seen in the normative data base.
At this point, it was too early to tell what was going on with our patient. We were most suspicious of idiopathic intracranial hypertension (IIH), but we also recognized the list of differential diagnoses can be quite extensive.
IIH predominantly affects obese women of childbearing age.1 It has no known etiology; however, risk factors for IIH include exposure to or withdrawal from certain exogenous substances, systemic diseases, certain endocrine or metabolic disorders and disruption of cerebral venous flow.1 Our patient was 5 feet 2 inches and weighed 133 pounds, but she did admit that, over the past four months, she had lost more than 15 pounds due to changes in her diet and exercise. On appearance, she seemed fit and not significantly overweight.
Given the clinical findings of bilateral disc edema, a medical work up that includes magnetic resonance imaging (MRI) and a lumbar puncture (LP) is a mandatory next step.
Our patient had an MRI of her brain and orbits on the same day of our exam. It was normal without detection of any mass lesions. The following day an LP was performed and her opening pressures were 50cm H2O. The normal range is 7cm to 18cm H20, so our patient’s cerebrospinal fluid (CSF) pressure was extremely high—consistent with a diagnosis of IIH.2
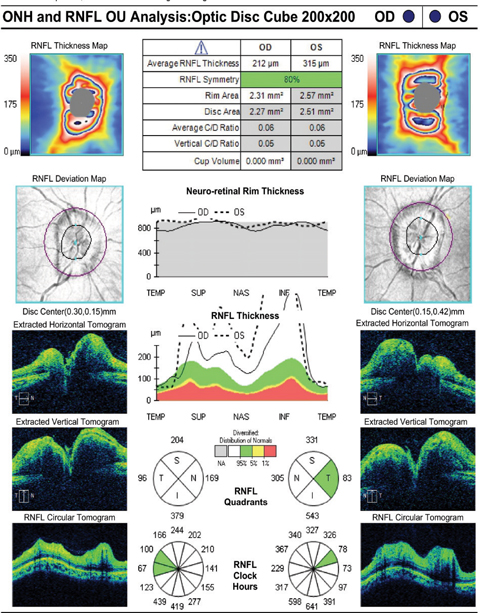 |
| Fig. 2. How would you interpret these retinal nerve fiber layer OCT findings in our patient? Click image to enlarge. |
Discussion
IIH develops from chronically elevated intracranial pressure (ICP). Terminology for this condition has evolved over the years. Pseudotumor cerebri and benign intracranial hypertension are synonymous terms and were commonly used to describe this condition until IIH emerged as the preferred term.
The most significant neurologic complication from IIH is papilledema, which, if left untreated, may lead to progressive optic atrophy and blindness. The grading of optic nerve swelling based on the modified Frisén classification (Table 1).3
Other neurologic symptoms of elevated ICP include severe headaches, ringing in the ears, blurred vision and diplopia, which may result from a cranial VI palsy.1,4 Our patient had none of these symptoms.
Management
Weight loss is considered the best long-term management for this condition, but can be difficult for patients to maintain.5 A referral to a dietitian may be appropriate to help formalize this process. Our patient is off to a good start as she had already lost 14 pounds over the past three months.
The most affective pharmacologic treatment for IIH is acetazolamide. The initial dosage is 0.5g to 1g per day, usually with the 500mg Diamox Sequels bid.1,4 Unfortunately, many patients become intolerant to the side effects of the medication, which include paresthesias in the extremities, fatigue, metallic taste from carbonated beverages and decreased libido. In patients that develop progressive vision loss despite being on Diamox, surgical management may be warranted. Options include optic nerve sheath fenestration, lumboperitoneal or ventriculoperitoneal as a means of diverting the CSF and venous sinus stenting.1,4
We started our patient on 1g of acetazolamide per day and counseled on the benefits of weight loss. She was asked to return in six weeks for follow up.
1. Friedman DI. Papilledema. In: Miller NR, Newman NJ, Biousse V, Kerrison JB, eds. Walsh & Hoyt’s Clinical Neuro-Ophthalmology. 6th ed. Vol I. Philadelphia: Lippincott Williams & Wilkins; 2005, 237-91. |
Retina Quiz Answers:
1) d; 2) d; 3) d; 4) d.

