 |
A 66-year-old Vietnamese female, recently arrived in the United States, presented complaining of debilitating blurred vision at distance and near, right eye greater than left, constant and progressive over a three-month period. She reported no pain, headache, nausea, photosensitivity or trauma. She denied both significant ocular history and any previous eye exam. She recently underwent her first medical examination, resulting in a diagnosis of hypertension and hyperlipidemia.
Examination
At the initial visit, her best-corrected visual acuities (BCVAs) were 20/70 OD, 20/30- OS, and she had a 2+ afferent pupillary defect (APD) OD. Confrontations showed significant constriction in all quadrants OD, FTFC OS. Intraocular pressures (IOP) were 52mm Hg OD, 32mm Hg OS. Slit lamp exam revealed shallow anterior chambers in both the left and right eyes; mature nuclear sclerotic cataract greater in the right eye than in the left; glaucomatous cupping and superior notch approaching the rim in the patient’s right eye; and possible early glaucomatous changes to her left eye.
During the glaucoma work-up, gonioscopy revealed no visible structures in primary gaze in all quadrants; open to the anterior trabecular meshwork (TM) with indentation in the right eye; plateau iris in all quadrants, most apparent along horizontal midline in the right eye; ATM in superior, nasal, inferior quadrants in the left eye, no visible structures temporal; steep iris approach in multiple angles with varied presentation in the left eye; and no PAS OU. Angle optical coherence tomography (OCT) imaging showed significant narrowed angles in both eyes, but in the right eye greater than in the left, and convex iris approach in both eyes. Pachymetry readings were 430 OD, 408 OS. OCT RNFL found average thickness 54 OD, 102 OS; severe thinning S/T/I OD, WNL OS. OCT Mac had average GCC + IPL thickness 48 OD, 76 OS; and severe thinning in all quadrants of the right eye, WNL OS.
We could not perform visual fields secondary to the language barrier.
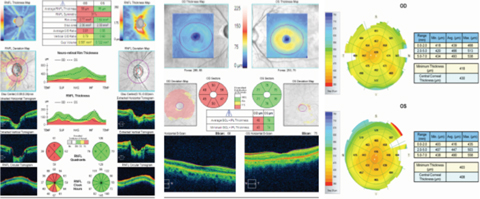 |
| OCT imaging suggests the patient’s elevated IOP was connected to narrowed angles. Click image to enlarge. |
Treatment
Because of the narrow angles and elevated IOP, she was held in clinic and started on Betimol (timolol 0.5%, Akorn), Simbrinza (brinzolamide/brimonidine tartrate ophthalmic suspension, Alcon) and, eventually, pilocarpine 2%. This regimen reduced her IOPs to 30mm Hg OD, 26mm Hg OS.
The patient was scheduled for urgent extracapsular cataract extraction with iStent (Glaukos) implant OD, OS. The procedure had no complications and an uneventful post-op period.
| Anterior segment OCT shows the post-op state of the TM, uveal tract and Schlemm’s canal OD, above, and OS, below. |
Follow Up
The 30-day post-op findings were remarkable. The patients IOP was 13mm Hg OD and 14mm Hg OS—an incredible reduction of 75% in the right eye and 56.2% the left. Her BCVAs were 20/30 OD (subjective complaint of bisected fixation), 20/20 OS with a 2+ APD OD. Confrontations were the same. A slit lamp exam showed a deepened anterior chamber in both her right and left eyes; well-apposed CE wound in each eye; and stable, centered PCIOL without opacity in both the right and left eyes. Her ONH c/d was 0.85v/0.75h with superior notch approaching rim in the right eye, 0.55r OS.
Repeat gonioscopy showed all quadrants open to the posterior TM with sparing view of scleral spur in the right eye; all quadrants open to scleral spur in the left; normal iris approach without pathology; and visible iStent nasal in each eye. Angle OCT showed increased angle depth with iris positioned in a more conventional location. OD remained more narrow than OS.
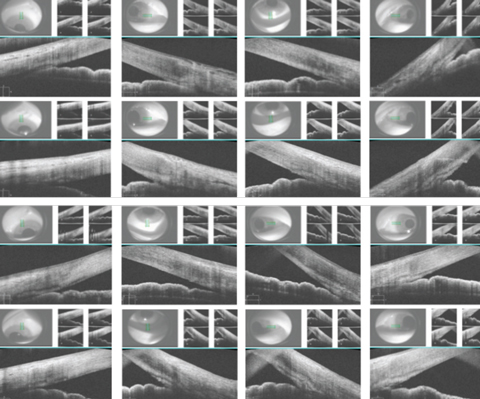 |
| These images show each quadrant of the patient’s eyes, both pre- and postoperatively. The first row shows the right eye preoperatively, the second row shows the right eye postoperatively, the third row shows the left eye preoperatively and the last row shows the left eye postoperatively. Click image to enlarge. |
Discussion
In this case, a firm diagnosis was hampered by substantial pertinent negatives. Bilateral, asymmetric, severely narrowed angles suggest angle anatomy played a large factor in the elevated IOP, which also presented bilaterally but with asymmetric presentation worse in the right eye. This substantiated the final diagnosis of chronic narrow-angle glaucoma via a phacomorphic mechanism. That, in conjunction with the cataracts, indicated cataract extraction would be the appropriate first step in managing both the glaucoma and reduced acuity.
Continuous lens growth that shortens the anterior chamber length, positioning the anterior lens anterior to Schlemm’s canal, offers a mechanism for elevation. This slight displacement causes forward traction on the ciliary body via the zonules, which causes displacement of the uveal tract and crowding of Schlemm’s canal and TM.1
Anterior segment imaging was critical in this case. Potential quantitative parameters, including anterior chamber angle and depth, trabecular-iris angle and surface area and angle opening distance, give researchers an opportunity to confirm the increase in angle depth observed following cataract extraction while exploring the correlation with angle anatomy and IOP.2,3 This is particularly significant in narrow-angle or chronic-angle closure glaucoma, as it consistently demonstrates a stronger relationship than open-angle glaucoma.4-7 This information would provide clinicians predictive models of angle and IOP changes following cataract surgery.8
The medical decision-making and therapeutic results of this case are also largely impacted by the availability of the iStent. The device allows aqueous humor to drain directly from the anterior chamber to Schlemm’s canal, avoiding the resistance of the TM completely. Recently published meta-analyses show iStent implantation with lens extraction decreased IOP by 9% from baseline compared with lens extraction alone with a 4% reduction; two iStents reduced IOP by 27% from baseline.9,10 Individual studies show reduction in baseline IOPs of upwards of 30%, and elimination of ocular hypotensives at six-month follow-ups in as many as 74% of open-angle glaucoma (OAG) patients and 42% of primary OAG patients at four-year follow-ups.11
No studies examining closed-angle or narrow-angle glaucoma patients and the postoperative benefits of a combined phaco/iStent procedure are available. Still, with the well-documented safety of iStent implants, reduced post-op visits and less need for revision, the option was an excellent use of aggressive medical therapy in a patient with cost and compliance concerns.9
While the literature strongly supports iStent insertion in combination with cataract extraction as a viable and safe treatment for POAG, this case provides strong support for the same treatment in narrow-angle glaucoma patients. The expected decrease in pressure is related to the preoperative angle anatomy and pressure. Generally speaking, the more narrow the angle and the higher the IOP, the more dramatic the improvement—and that’s precisely what we saw with this patient.
1. Poley B, Lindstrom R, Samuelson T. Long-term effects of phacoemulsification with intraocular lens implantation in normotensive and ocular hypertensive eyes. J Cataract Refract Surg. 2008;34(5)735-42. |

