Refractive surgery is a constant evolution of technological advancement and, as a result, an educational challenge for the practicing O.D. Just as we acquire the knowledge and clinical expertise to incorporate a new and improved treatment modality, the available armamentarium of options expands.
On September 10, 2004, the FDA approved another device for the refractive surgery patient: the Verisyse phakic IOL for the treatment of high myopia (ranging from 5.00D to 20.00D in patients ages 21 and older with <2.50D of astigmatism and an anterior chamber depth 3.2 mm).
My first clinical experience with the Verisyse IOL was in 2000, while working as a clinical associate of Vance Thompson, M.D., one of the principle FDA investigators for this device. Since then, I have been involved in the treatment of patients using this technology and have witnessed the impressive results of high myopia correction following implantation of the IOL. It has quickly become my treatment of choice for moderately to highly myopic patients contemplating refractive surgery.
Lens Design
The Verisyse implant, also known as the Artisan phakic IOL, is manufactured by Ophtec and distributed by Advanced Medical Optics Inc. (AMO) in North America and Japan.
This implant is an anterior chamber phakic intraocular lens that functions through a unique iris fixation method. This positioning is known as iris enclavation in which the fixation arms (haptics) of the lens attach to the stroma of the iris in the non-reactive mid-periphery. There is no significant disruption in pupil function, and this orientation permits centration of the lens over the pupil. The unique convex-concave design allows the lens to be positioned away from the crystalline lens and the corneal endothelium. The fixation of the lens in the iris does not disrupt the anterior chamber angle or impede pupil fixation, and the entire lens is visible to the clinician.
Early in my clinical experience with the Verisyse lens, the typical candidate was the highly myopic patient who had too thin a cornea for LASIK or keratometry readings too flat for optimum laser vision correction. In addition, the patient who had apprehension about excessive tissue removal with high-diopter LASIK was impressed with the Verisyse technology. With each successful case, my enthusiasm grew and, as a result, I introduced more myopic patients to the Verisyse IOL. My clinical view of whom I believed was an ideal candidate kept moving from the extremely myopic patient to the moderately myopic correction level.
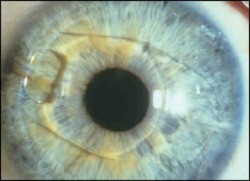 |
| Appearance of the Verisyse phakic intraocular lens in the eye after implantation. |
Most patients were very receptive to the reversible nature of the procedure along with the tissue preservation issue. The Verisyse lens would also allow for PRK or LASIK in the future if residual correction was necessary after implantation.
Clinical Findings
One of the most impressive advantages of the Verisyse lens is the improved image quality patients report following the procedure. Here are some additional impressive findings:
Contrast sensitivity is preserved and often improved following the procedure.1
The rate of retinal detachment in the myopic patient was not increased following phakic IOL surgery compared to lensectomy procedures. 2, 3
The preservation of the crystalline lens allowed for continued accommodation after treatment.2
The predictability of the targeted outcome was impressive. All patients that I evaluated were within +/- 1.00 D spherical equivalent of the goal.
Most of the patients I evaluated had uncorrected vision of 20/40 or better and, over the three-year study, there was very little regression or fluctuation in either the uncorrected vision or the manifest refraction.
|
History of the Verisyse |
| The Verisyse lens was first designed as an aphakic implant and has successfully been used in over 400,000 patients worldwide for this application. Its first use for treatment of myopia came in 1986; currently, more than 100,000 myopic patients outside the U.S. have been treated with the current device for myopia correction. The lens was designed by Netherlands-based professor Jan G. F. Worst, M.D. Over the course of the past 20 years, several technical modifications have resulted in the current lens design, which obtained FDA approval for the treatment of myopia in the U.S. following a three-year study. |
Patient Management
There are distinct differences in patient management when treating with the Verisyse lens, and different risk factors apply. As an intraocular procedure, the results will be surgeon-sensitive. Proper placement of the IOL is critical for optimum visual functioning, primarily the centration of the lens. Good surgical technique is critical to preservation of the intraocular architecture and long-term eye health.
All patients I worked with were educated about blur in the early stages of post-procedural care. The reason for this strong discussion was that residual astigmatism can diminish the image at first, but patients that were informed were less likely to be concerned. The ability to manage potential residual astigmatism is important for a positive first impression to the patient, and good surgical technique can often make a difference. Wound placement, relaxing incisions and, if indicated, selective suture removal can be crucial to the reduction of post-surgical cylinder, which can impact image quality for the patient in the early post-surgical course.
Unlike most refractive surgery procedures that are bilateral, the Verisyse lens will be a monocular surgical procedure. The wait between eyes will be approximately two weeks for the conservative surgeon. In most cases, this will require balancing of the anisometropia with contact lens application for the period between surgeries.
The Verisyse lens design has an optical zone of 6mm up to 15.00D and 5mm up to 20.00D. Visual symptoms at night such as glare, halos and starbursts after lens implantation were experienced by some patients in the FDA trial. The optical visual symptoms may have been due to residual refractive error. I expect that such refractive error will be less common post-approval, now that 0.50D lens power increments are available and post-implantation refractive surgery is permitted to correct residual astigmatism.
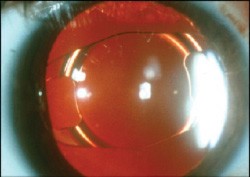 |
| Photo of the dilated pupil demonstrates that the Verysyse IOL does not interfere with pupil dynamics. |
In my experience with more than 100 Verisyse IOL patients, the issue of nighttime glare was not significant. Working with a talented surgeon, our patients normally had minimal residual cylinder and were educated that thin spectacles may be needed to correct residual refractive error for dim illumination image quality enhancement. Our staff and physicians were very sensitive to proper scotopic pupil measurements, and all patients were counseled thoroughly about the risks of glare. Interestingly, the majority of patients I worked with had significant optical device-induced glare problems prior to their procedure and was potentially desensitized to this issue post-surgically. My clinical experience in evaluating the post-Verisyse implant case has not demonstrated a significant difference, compared to the post-surgical ALK or high-dioptic LASIK patient vision in dim illumination. I believe this is potentially a minor clinical and vision performance issue, as it relates to the overall outcome.
Post-op Care
The post-operative management of the Verisyse phakic IOL patient is straightforward. As optometrists, we have become experts in the management of post-surgical cataract cases, and with the phakic IOL case the same basic aspects of good care apply.
I first observe the wound for leakage signs, determine the level of any surgically induced intraocular inflammation and review IOL placement and security. In addition, basic vision measurements to review BCVA and residual refractive error are important at each visit. Some interesting observations you will see with the Verisyse IOL case include pigment dispersion and peripheral iridotomy. Normally, a small amount of pigment will be noted on the anterior lens or between the IOL and crystalline lens. Most surgeons will create peripheral iridotomies to ensure a reduced risk of pupillary block glaucoma.
In all patients, a thorough discussion of the potential for additional surgery to improve uncorrected acuity is presented prior to surgery. (The ability to reduce residual refractive error with either PRK or LASIK is known as a bi-optic case.) Often residual astigmatism needs attention and six months after implantation of the Verisyse IOL, a laser vision correction procedure can improve UCVA. Patients remain impressed that they have the option to improve vision by additional refractive surgery if they desire.
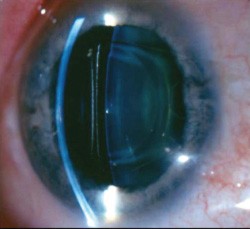 |
| Slit lamp photo showing lens vaulting over the iris plane and distance between the lens and corneal endothelium. |
I have found a majority of patients in the uncorrected state of 20/40 or better are so happy with their vision quality and have overcome such a significant disability that they do not fall into the Greedy Vision Syndrome. Many elect to stay where they are after initial Verisyse treatment. Thin glasses for this class of patient do not represent perceived failure as in the high-expectation LASIK patient.
In the near future, phakic IOL implantation will become more of a mainstream option for the patient seeking refractive surgery and one you will not want to miss developing expertise in.
Dr. Ferguson is in private practice in Dakota Dunes, South Dakota. He specializes in clinical refractive surgery care, dry eye treatment and corneal reshaping. Dr. Ferguson has no financial interest or relationship with AMO or any of the companys products.
1. El Danasoury MA, El Maghraby A, Gamali TO. Comparison of iris-fixed Artisan lens implantation with excimer laser in situ keratomileusis in correcting myopia between 9.00 and 19.50 diopters: a randomized study. Ophthalmology 2002;109:955-64.
2. Pop M, Payette Y. Refractive lens exchange versus iris-claw Artisan phakic intraocular lens for hyperopia. J Refract Surg 2004;20:20-24.
3. Jacobi FK, Hessemer V. Pseudophakic retinal detachment in high axial myopia. J Cataract Refract Surg 1997;23:1095-1102.

