 |
Two Caucasian females, both in their late 70s, presented as new patients in order to establish care. Both had similar histories insofar as having been diagnosed with glaucoma for several years and managed with medications and surgery. One patient had SLTs performed bilaterally, whereas the other had bilateral SLTs and a trabeculectomy in one eye. Upon presentation, both were clearly in the advanced stage of their glaucoma. And then their stories diverged somewhat.
They were initially seen by me approximately 12 months apart, with the latter having been a patient of mine now for only nine months or so. Where I practice has a very large influx of patients who are moving to the area for retirement. Inheriting someone else’s patient is part and parcel of having a glaucoma practice, but at the end of the day, successfully managing these patients is a win-win for everyone: the patient, myself and the practice.
 |
| Olleyes virtual reality visual field unit. Full glaucoma threshold visual field capability is available on the device. Click image to enlarge. |
Management Challenges
While the majority (about 75%) of glaucoma patients fall into the mild to moderate category, some will certainly fall into the advanced category (about 15%), and the remaining will fall into the refractory category (about 10%), meaning that despite appropriate therapy, they continue to progress or have difficulty maintaining stability. Optometry is well positioned to manage the 75% of glaucoma cases that fall into the mild to moderate stage and often can do so without the assistance of our non-optometric ophthalmic colleagues. Even the 15% of patients who have advanced disease can be managed by optometry and surgical intervention. But oftentimes, in cases of advanced disease, there are some refractory patients who need further care by fellowship-trained glaucoma surgeons.
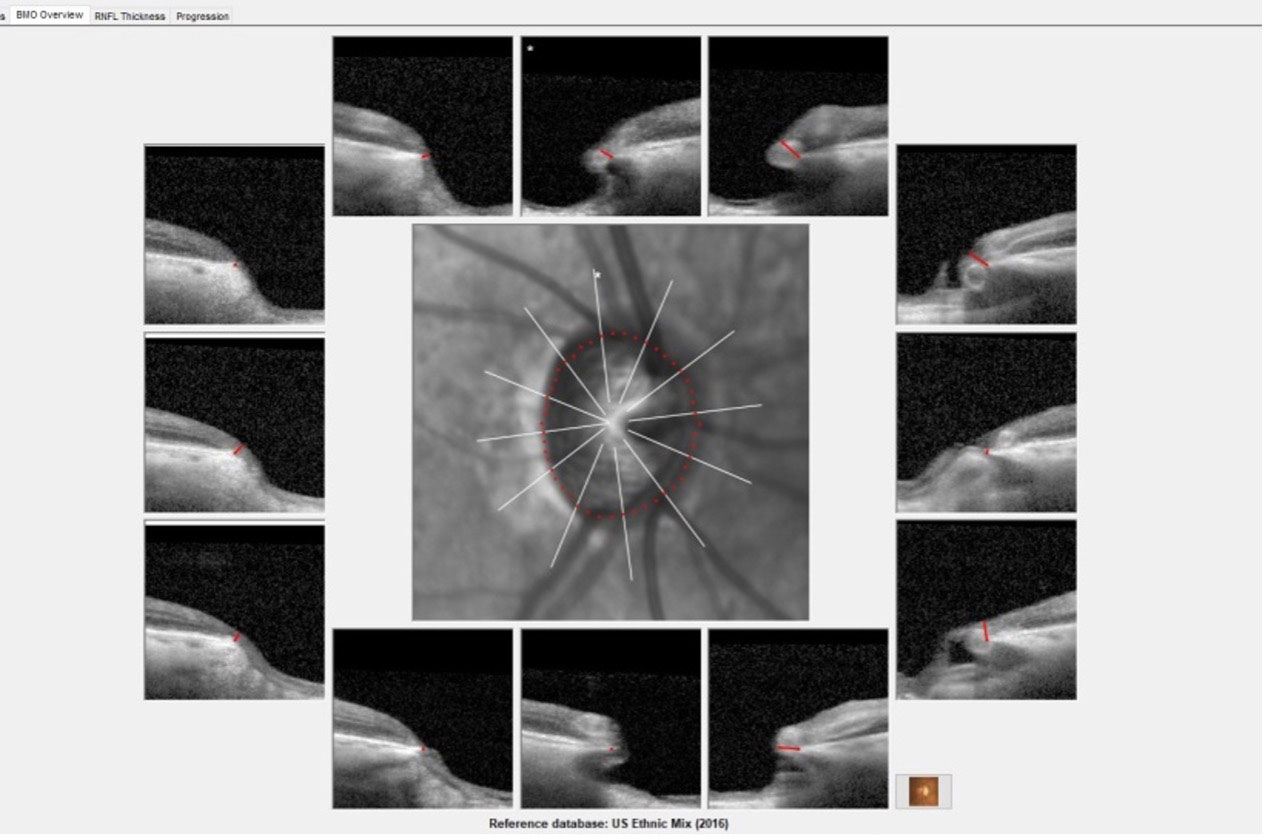 |
| Radial optic nerve scans obtained at the 12 o’clock position with significant thinning of the neuroretinal rim from six o’clock through 12 o’clock in the right eye of the patient with more advanced structural damage. Click image to enlarge. |
Our challenge in managing patients with advanced disease lies in making sure they remain stable. In essence, this is our goal for all glaucoma patients. Certainly, in mild to moderate disease states, there is a bit of room for some progression throughout the patient’s lifetime without significant effects on quality of life, but in patients with advanced disease, there is little room for progression. Once progression is even subtly determined, a change in therapy is warranted, often involving a surgical strategy.
Determining progression in glaucoma involves both structural and functional testing. Studies seem to indicate that patients with minimal to no visual field loss are best identified as having progressed by changes seen in their OCT findings, whereas individuals with more advanced disease seem to demonstrate progression more readily with visual field changes.1 This is certainly partly attributable to the floor effect seen when there is significant loss of retinal ganglion cells, but these rules are not steadfast in all cases. At the end of the day, both structural and functional testing is required for all glaucoma patients, independent of disease staging.
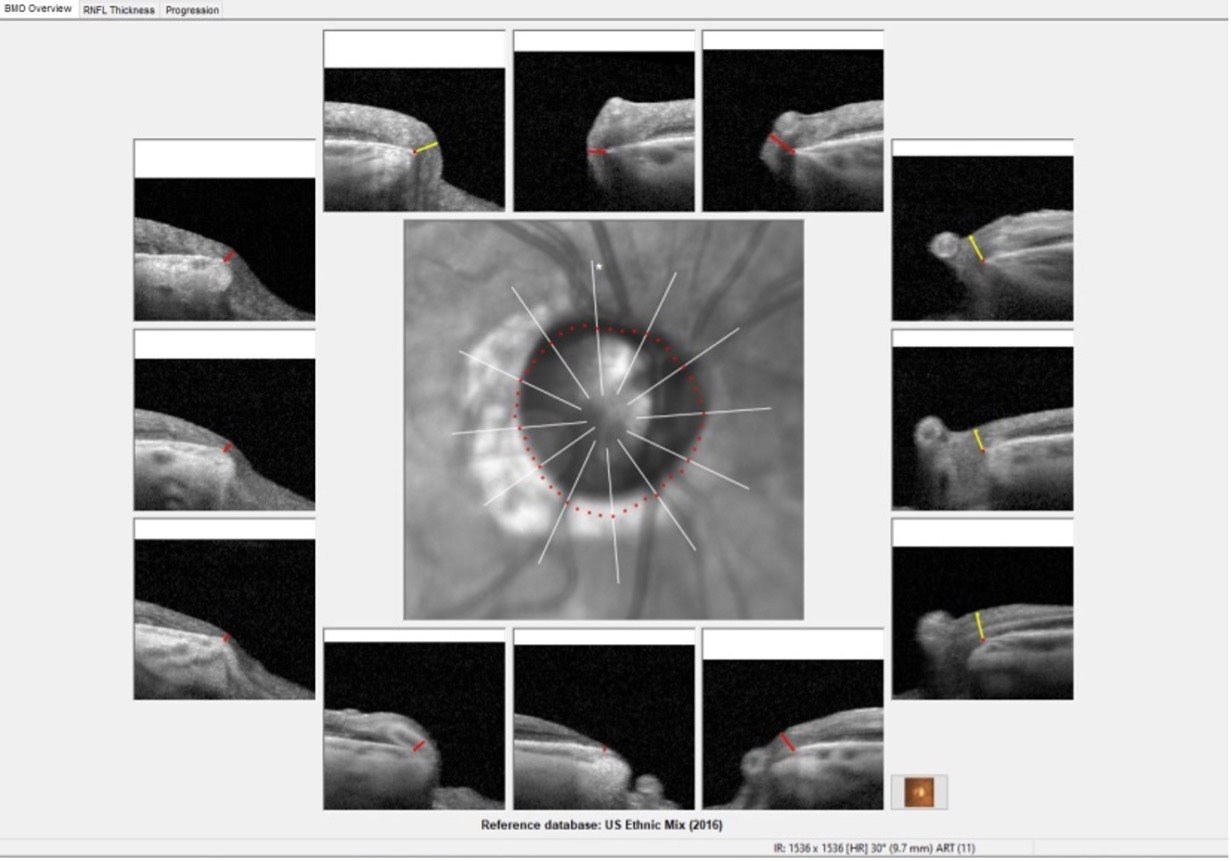 |
| Erosion of the temporal neuroretinal rim in the right eye of the other patient. Click image to enlarge. |
One of the inherent difficulties in visual field studies is the subjectivity of the testing, not to mention the simple truth that many patients do not enjoy sitting for a visual field test. Reliability indices can clearly give an indication as to the usefulness of the visual field in determining whether or not there is progression. Perhaps newer visual field platforms, such as virtual reality headset-based field testing, may make the testing experience more enjoyable for the patient and more reliable as well. We’ve introduced virtual reality visual field testing in my office, and to my surprise, the large majority of patients who have used the device have actually commented that they enjoy that modality.
Case Details
Both patients’ BMO-MRW printouts showed significant erosion of the neuroretinal rims in just about all sectors of the optic nerves, especially temporally. One of the places to look for structural progression of glaucoma (in addition to the circumpapillary RNFL) is the neuroretinal rim. OCT of these patients should include scans of the RNFL, BMO and macular ganglion cell layer, all the while looking for subtle signs of progression.
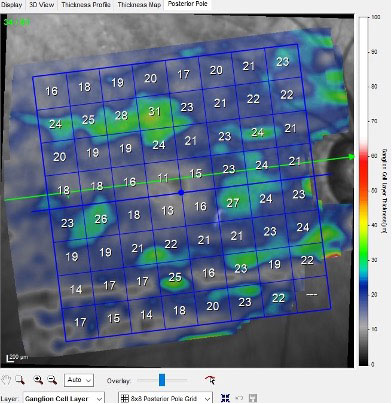 |
| An exceedingly thinned ganglion cell layer in the macula of the patient with more advanced structural damage. Click image to enlarge. |
Interestingly, the patient with slightly more advanced structural damage, the most recent of the two, has remained stable throughout the time I have seen her, but the other has progressed, which is especially evident in the ganglion cell layer analysis.
She has been a challenge from the first visit, presenting with an extensive history of red irritated eyes, sensitivity to several glaucoma medications, a failed trabeculectomy in one eye and IOPs in the mid-teens OU. She was on a steroid drop TID to control for inflammation and three separate glaucoma medications. Frankly, her eyes were unacceptably inflamed.
My initial goal of her treatment was threefold: (1) to decrease her medication burden, (2) to reduce her chronic inflammation and (3) to obtain better IOP control. After reviewing her previous records and adjusting a variety of her medications, slowly but surely, and with very close monitoring, we were able to achieve a reasonably good outcome of all three goals. This took, however, the better part of six months to accomplish. All the while, her fields and OCT findings remained stable.
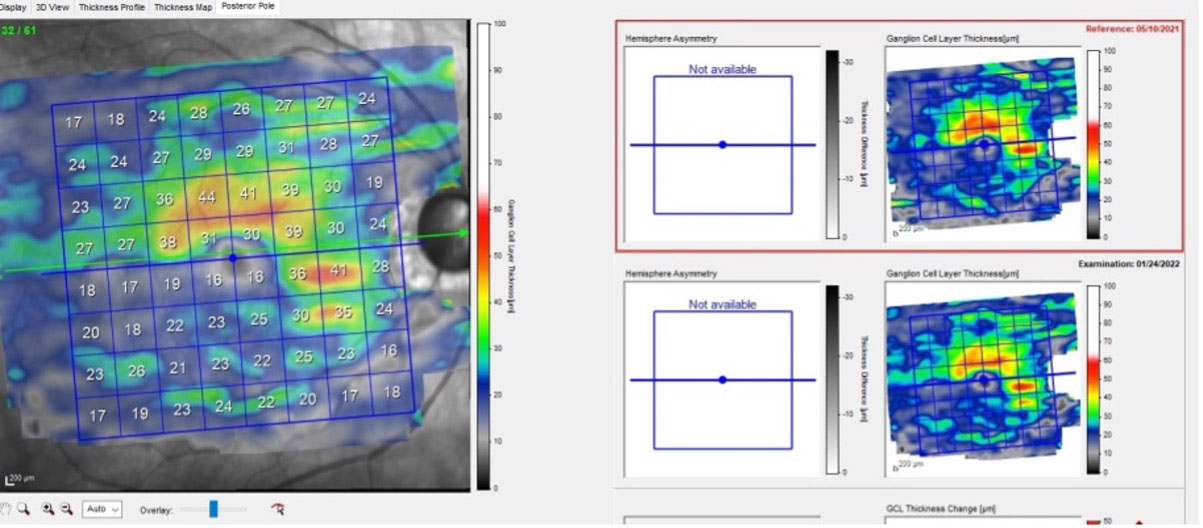 |
| Subtle progression in ganglion cell layer loss in the other patient. Click image to enlarge. |
Unfortunately, her OCTs began to show subtle change recently, and without any realistic medical options left, she was referred to the most appropriate glaucoma surgeon for further intervention. While her disease was not quite as advanced as the other patient, she is the one who has been experiencing consistent progression while in my care.
Will this patient be seeing the glaucoma surgeon exclusively from here on out? No, the glaucoma surgeon will render what surgical intervention they believe would best suit the patient, but she will ultimately return to my care for continued management. It’s important to find the right glaucoma surgeon, one who provides the best care for the patient and has mutual respect for all members of their care team. Great glaucoma surgeons do great things in the operating room and recognize that great optometrists do great things in the office. And sometimes, that great glaucoma surgeon is not in your home town.
Dr. Fanelli is in private practice in North Carolina and is the founder and director of the Cape Fear Eye Institute in Wilmington, NC. He is chairman of the EyeSki Optometric Conference and the CE in Italy/Europe Conference. He is an adjunct faculty member of PCO, Western U and UAB School of Optometry. He is on advisory boards for Heidelberg Engineering and Glaukos.
1. Abe RY, Diniz-Filho A, Zangwill LM, et al. The relative odds of progressing by structural and functional tests in glaucoma. Invest Ophthalmol Vis Sci. 2016;57(9):421-8. |

