 |
All eye care providers know dry eye signs and symptoms do not correlate.1 Patients reporting dryness, burning, itching, fluctuating vision and even redness could be diagnosed with any number of conditions, including allergic conjunctivitis; blepharitis; eye misalignment issues such as convergence insufficiency and vertical imbalance; epithelial basement membrane dystrophy; giant papillary conjunctivitis; conjunctivochalasis; and conjunctival concretions, to name only a few. Fortunately, point-of-care tests such as osmolarity and inflammatory markers may help you make the differential diagnosis.2
However, there are also patients that truly have dry eye disease (DED) but lack significant symptoms (e.g., neurotrophic dry eye), while others may have a subtype of DED such as neuropathic ocular disease where symptoms are disproportionately advanced compared to signs.3 Making things even more confusing is the fact that many patients have clear physical signs of DED, including meibomian gland dysfunction, but are still asymptomatic.4 To help solve this confusion, let’s look at neuropathic ocular pain to better understand these phenomena.
Understanding Chronic Pain
In general, there are two types of pain associated with most conditions such as DED. Nociceptive pain is the pain we generally think of, commonly stemming from trauma, insult or the potential of insult to a specific location. Neuropathic pain, however, occurs due to a lesion or disease of the somatosensory nervous system.5 Neuropathic pain is a complex, chronic pain state that usually is accompanied by tissue damage; yet, sometimes it is simply dysfunction of the physiological nervous system.6
With neuropathic pain, the nerve fibers themselves are often damaged, altered or injured, and the tissue, in this case the ocular surface, itself is not affected.7 These nerves may become damaged as a result of hypersensitization of the corneal or conjunctival somatosensory nerves and can send incorrect signals to other pain centers within the body, such as the peripheral and central trigeminal sensory network.8
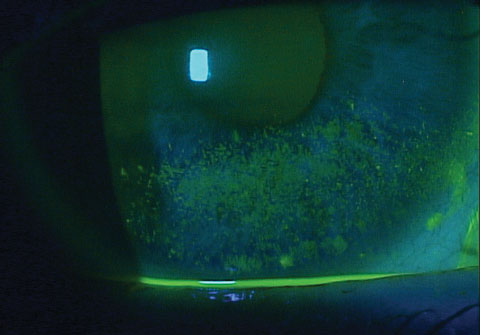 |
| Patients with corneal staining are already in the late stage of DED. You must catch it earlier with new diagnostic tools to avoid neuropathic pain. |
Although pain management specialists are familiar with managing pain without obvious signs, most optometrists are not. We want to be able to see improvement in signs and symptoms. Chronic stress such as lid wiper, hyperosmolarity, surgical procedures or inflammation can result in hypersensitization and eventual neuropathic pain, possibly explaining the significant variances that exist in symptoms among patients with various levels of DED.9
The more DED we manage, the more cases we’ll see of patients who, despite mild signs, are in such severe pain they cannot function (and patients with severe signs who have little to no symptoms at all). Some have referred to the neuropathic condition as “pain without stain,” which helps understand the disassociation between signs and symptoms for this type of DED.9 Furthermore, neuropathic pain may explain why patients with dry eye and reduced corneal sensitivity have significant dry eye symptoms.10 This form of dry eye disease requires astute clinical judgment to make the diagnosis since demonstrable signs are not readily visible.
Ocular neuropathic pain is a likely symptom because of the presence of significant corneal nerves, and the unique location of the corneal nerve endings between the superficial epithelial cell and near the ocular surface make them vulnerable to repeated damage from environmental exposure and hyperosmolarity.11 Research involving a mouse model shows the primary afferent nerves became sensitized on exposure to hyperosmolar and inflammatory solutions.12
Diagnosis
Diagnosis involves significant clinical judgment and a good understanding of the disease course. By definition, patients with neuropathic pain will often experience hyperalgesia or exaggerated pain, spontaneous pain, allodynia (a pain response to normal stimuli such as light or mild air flow) and dysethesias (abnormal sensations). Patients with chronic pain such as neuropathic pain also tend to have higher levels of anxiety, depression and sleep disorders.13,14
Although advanced testing such as confocal microscopy potentially can show a damaged sub-basal nerve plexus, most of us do not have access to such technology.15 The primary method of diagnosis is secondary to symptoms that do not resolve with typical DED treatments. A more specific and effective way to make the diagnosis of neuropathic dry eye is to instill topical anesthetic in the eye. Patients with neuropathic pain will typically mention little to no resolution of their symptoms.5,16
Treatment
Unfortunately, these patients rarely respond well to local treatments. Still, we should treat the inflammation possibly contributing to their dry eye, as there may be benefit over time and with long-term use. Furthermore, local treatment may remove the stress and continuous stimuli causing the pain response. However, more standard treatments such as artificial tears do not provide patient-reported pain resolution in most cases.13 Therefore, consider using options with anti-inflammatory properties, including corticosteroids, Restasis (cyclosporine ophthalmic emulsion, Allergan), Xiidra (lifitegrast, Shire) and oral doxycycline, to name a few. Autologous serum, which includes nerve growth factor among its contents, may affect corneal nerve function.17
Treating the ocular surface is essential to minimizing further insult or removing stimuli that is exaggerating pain. Other treatments include those targeting the neuropathic pain centers and descending pathways, such as tricyclic antidepressants, serotonin–norepinephrine reuptake inhibitors (SNRIs) and gabapentinoids.18 However, tricyclic antidepressants and SNRIs may exacerbate ocular surface issues, given their strong anticholinergic activity and potential ocular drying effects. Nonsteroidal anti-inflammatory drugs (NSAIDs) are another topical option that may affect the nerves because of their ability to decrease peripheral sensitization.18,19 Thus, treatment with gabapentinoids and topical NSAIDs may affect more nerve pathways than using one alone. Research also shows protecting the ocular surface from environmental stimuli may benefit patients with neuropathic pain, and scleral lenses may help those with neuralgia-type pain.20
Catch it Early
However, as with any condition, prevention is the best treatment, and preventing neuropathic pain requires early diagnosis of DED. In the early stages, DED patients typically have persistent stimuli such as hyperosmolarity and inflammation. Eventually, the pain—now neuropathic—remains even after the initiating insult is removed or treated.21 In the case of lid wiper epitheliopathy, for example, longstanding trauma could eventually result in neuropathic pain and, even if the lid wiper is then treated, the neuropathic pain will persist.5
To ensure earlier diagnosis, we must use better diagnostic testing. Research shows NaFl corneal staining is a late disease indicator similar to a visual field defect in a patient with glaucoma.22 Early disease diagnosis, however, requires uncovering early disease indicators, and newer technologies such as meibography, non-invasive break-up time and osmolarity testing—perhaps the most sensitive test to early DED—can help identify the beginning structural changes.22
Neuropathic dry eye is a fascinating yet difficult condition to manage. Doctors need to be aware of this condition to help prevent its development with early intervention of dry eye disease. In cases where DED and neuropathic pain coexist, knowing how to make the diagnosis and treatment options can make a significant difference in the lives of these patients.
|
1. Nichols KK, Nichols JJ, Mitchell GL. The lack of association between signs and symptoms in patients with dry eye. Cornea. 2004;23(8):762-70. 2. Bron AJ, Tomlinson A, Foulks GN, et al. Rethinking dry eye disease: a perspective on clinical implications. Ocul Surf. 2014;12(2 Suppl):S1-31. 3. Spierer O, Felix ER, McClellan AL, et al. Corneal mechanical thresholds negatively associate with dry eye and ocular pain symptoms. Invest Ophthalmol Vis Sci. 2016;57(2):617-25. 4. Arita R, Minoura I, Morishige N, et al. Development of definitive and reliable grading scales for meibomian gland dysfunction. Am J Ophthalmol. 2016 Sep;169:125-37. 5. McMonnies CW. The potential role of neuropathic mechanisms in dry eye syndromes. J Optom. 2016 Jul 15. pii: S1888-4296(16)30034-6. 6. Weiner DK. Office management of chronic pain in the elderly. Am J Med. 2007;120:306-315. 7. Tsantoulas C, Zhu L, Shaifta Y, et al. Sensory neuron downregulation of the Kv9.1 potassium channel subunit mediates neuropathic pain following nerve injury. J Neurosci. 2012 Nov 28;32(48):17502-13. 8. Goyal S, Hamrah P. Understanding neuropathic corneal pain—gaps and current therapeutic approaches. Semin Ophthalmol. 2016;31(1-2):59-70. 9. Rosenthal P, Baran I, Jacobs DS. Corneal pain without stain: is it real? Ocul Surf. 2009;7:28-40. 10. Benitez-Del-Castillo JM, Acosta MC, Wassfi MA, et al. Relation between corneal innervation with confocal microscopy and corneal sensitivity with noncontact esthesiometry in patients with dry eye. Invest Ophthalmol Vis Sci. 2007;48:173-81. 11. Galor A, Levitt RC, Felix ER, et al. Neuropathic ocular pain: an important yet under-evaluated feature of dry eye. Eye. 2015;29:301-12. 12. Parra A, Gonzalez-Gonzalez O, Gallar J. Tear fluid hyperosmolality increases nerve impulse activity of cold thermoreceptor endings of the cornea. Pain. 2014;155(8):1481-91. 13. Haanpaa ML, Backonja MM, Bennett MI, et al. Assessment of neuropathic pain in primary care. Am J Med. 2009;122:s13-21. 14. Crane AM, Levitt RC, Felix ER, et al. Patients with more severe symptoms of neuropathic ocular pain report more frequent and severe chronic overlapping pain conditions and psychiatric disease. Br J Ophthalmol. 2016 Apr 29. [Epub ahead of print]. 15. Spierer O, Felix ER, McClellan AL, et al. Corneal mechanical thresholds negatively associate with dry eye and ocular pain symptoms. Invest Ophthalmol Vis Sci. 2016;57:617-25. 16. Rosenthal P, Borsook D. Ocular neuropathic pain. Br J Ophthalmol. 2016;100(1):128-34. 17. Lambiase A, Micera A, Sacchetti M, et al. Alterations of tear neuromodulators in dry eye disease. Arch Ophthalmol. 2011;129:981-6. 18. Kraff MC, Martin RG, Neumann AC, et al. Efficacy of diclofenac sodium ophthalmic solution versus placebo in reducing inflammation following cataract extraction and posterior chamber lens implantation. J Cataract Refract Surg. 1994 Mar;20(2):138-44. 19. Kalangara JP, Galor A, Levitt RC, et al. Burning eye syndrome: do neuropathic pain mechanisms underlie chronic dry eye? Pain Med. 2016 Apr;17(4):746-55. 20. Parminder A, Jacobs DS. Advances in scleral lenses for refractive surgery complications. Curr Opin Ophthalmol. 2015 Jul;26(4):243-8. 21. Galor A, Zlotcavitch L, Walter SD, et al. Dry eye symptom severity and persistence are associated with symptoms of neuropathic pain. Br J Ophthalmol. 2015;99:665-68. 22. Schargus M, Ivanova S, Kakkassery V, et al. Correlation of tear film osmolarity and 2 different MMP-9 tests with common dry eye tests in a cohort of non-dry eye patients. Cornea. 2015 Jul;34(7):739-44. |

