 |
Oftentimes in practice, we encounter patients who subjectively report changes to their vision—but we then check their acuities and find no measurable difference in Snellen acuity. In these cases, we should consider an alternative measurement of vision quality: contrast sensitivity (CS). This brief, cost-effective screening tool can help us reveal factors relevant to their overall quality of vision.
Measuring visual acuity alone, using black letters on a white background, may not be completely representative of a patient’s ability to perform their normal activities of daily living. There is also evidence that CS testing can provide early detection of ocular diseases, even before visual acuity or other entrance tests are affected.1
CS is defined as the capability of perceiving minimal luminance changes between objects and areas, or the ability to differentiate two objects from each other and the background.1,2 CS testing measures the ability to discern patterns across a range of spatial scales and is implicated in several prevalent ocular diseases, such as amblyopia, glaucoma, diabetic retinopathy, cataracts and macular degeneration.3
Patients with affected CS will report trouble seeing street signs in the rain or fog, or greater difficulty reading the newspaper in the setting of normal or unchanged visual acuity.2,4 There are several factors that affect CS, both in regards to the limits of normal human vision as well as the effect of ocular disease processes, discussed below.
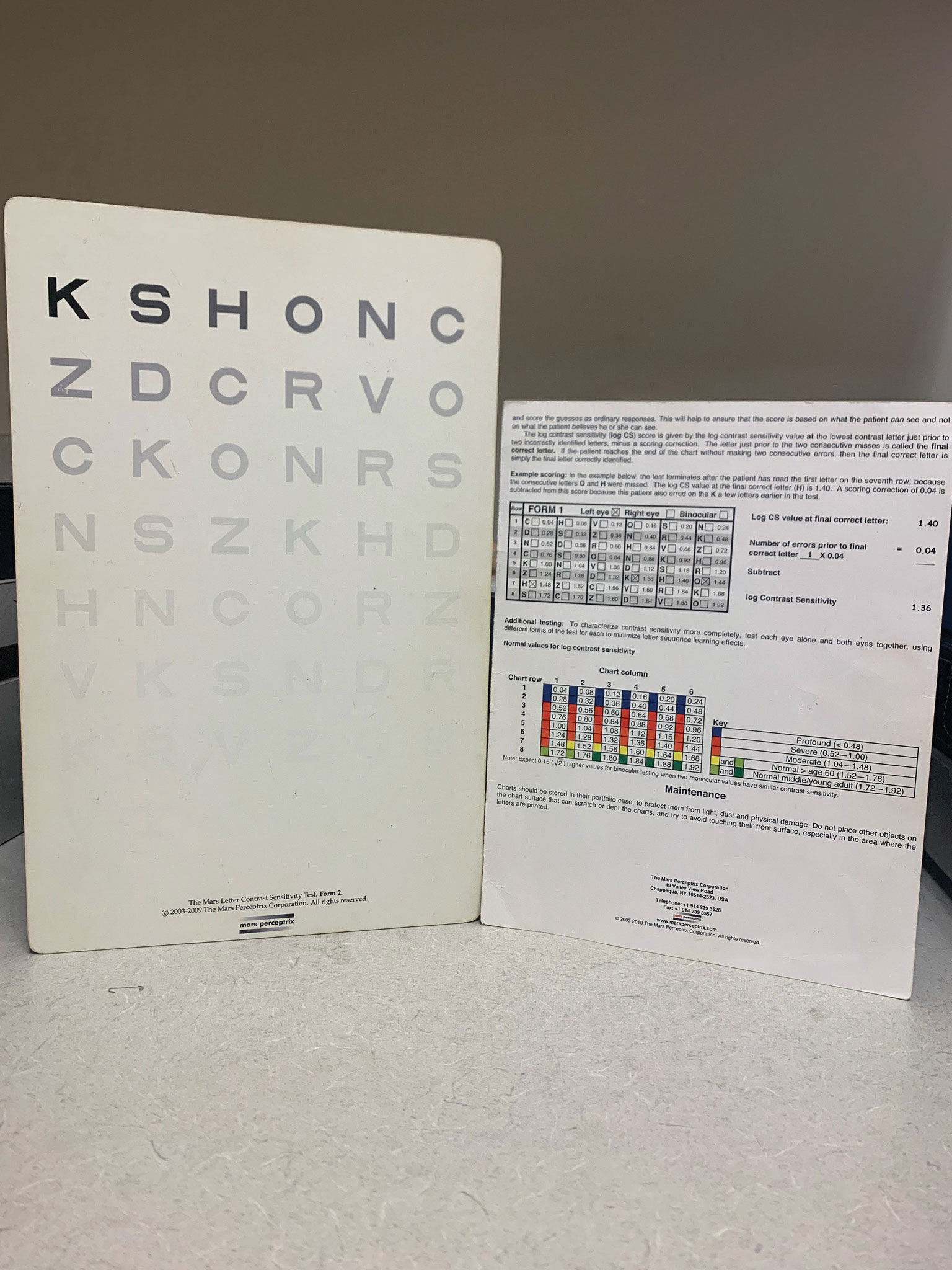 |
| The Mars letter contrast sensitivity test uses optotypes in decreasing contrast. Click image to enlarge. |
Light Scatter
The medium through which light normally travels contains numerous invisible particles suspended at various concentrations, causing light to scatter when encountering them. The greater the amount of light that is scattered, the less light is available to form a clear, distinct image with detailed contrast. This is the reason, for example, why it is more difficult to read street signs in rain or fog compared with a clear day.
The eye itself may also contribute to the increase in light scatter, such as in the presence of media opacities. A patient with a cataract will perceive a greater degradation in image quality and contrast due to the increase in light scatter by the hazy ocular media.1,2 This is why patients with cataracts will report glare and yet normal visual acuity could be unaffected.5 The same is true of patients who have undergone refractive surgery and report visual differences in the setting of good visual acuity.1,2
Retinal Photoreceptors
The angle that light hits the photoreceptors in the retina affects their response. For example, photoreceptors are most sensitive to light rays that strike them perpendicularly. This is known as the Stiles-Crawford effect and is the reason that light rays traveling through the pupil center form a clearer retinal image than those of the periphery. Also, if the orientation of the photoreceptors themselves is disrupted, such as in retinal diseases, the quality of the perceived retinal image is also diminished. An example of this would be age-related macular degeneration.2
Retinal and Neural Information Processing
The macula contains the highest number of cones which are responsible for fine, detailed acuity. Each cone contains blue, red or green pigment. When light strikes the cone photoreceptors, it is converted into a neurochemical signal that is passed on to the inner retinal cells, first the bipolar and then ganglion cells. Each ganglion cell contains a receptive field made up of a varying number of bipolar cells, with the highest concentration at the fovea.
This process and anatomical variation is responsible for image information that is relayed to the visual cortex for processing through the optic nerve and perceived visual stimuli.2
As we are already aware, glaucoma is a disease that targets the retinal ganglion cells and optic nerve. As such, damage to these structures has a direct impact on vision. Since peripheral vision is first affected in early glaucoma, patients who report blur or affected central vision are more likely to be describing CS rather than reduced Snellen visual acuity.
Visual ability in low illumination and reduced contrast are important functions in daily life of patients with peripheral vision loss due to glaucoma.6 Evidence suggests that recording CS in early glaucoma patients where central vision is not yet affected, or in very late stages where visual field defect progression is difficult to measure, can be beneficial in monitoring progression of the disease.7
Measuring and Managing
Though there is evidence regarding the effect of CS on image quality and visual function, there has yet to be a gold standard method of measuring CS in the clinical setting.2 Options include printed charts as well as computerized methods. Generally, gratings or optotype targets at varying levels of spacing or contrast are used in these tests.
The Pelli-Robson letter sensitivity chart is a common chairside test at distance that uses letters of the same size in order of decreasing contrast.2,4 The small-letter contrast test also uses rows of letters in decreasing contrast, but luminance is measured with a standard photometer. CS tests using the grating methods include the functional acuity contrast test and the VCTS 6500.2
In the event that a patient does suffer from reduced CS, many management options are available depending on their goals and affected activities of daily living. Something as simple as a referral for a lighting evaluation could offer great benefit for patients suffering from glare. The use of closed-circuit television aids or computer/smart phone apps or features to enhance contrast on their devices or displays are also a good option. These patients may also benefit from the use of filters and orientation and mobility services.4
With these options readily available, CS testing should be considered for patients with subjective visual complaints that do not match Snellen visual acuity to improve overall quality of vision and life.
1. Kara S, et al. Repeatability of contrast sensitivity testing in patients with age-related macular degeneration, glaucoma, and cataract. Arq Bras Oftalmol. 2016;79(5):323-7. 2. Amesbury EC, Schallhorn SC. Contrast Sensitivity and Limits of Vision. International Ophthalmology Clinics. 2003;43(2):31-42. 3. Thurman SM, Davey PG, McCray KL, et al. Predicting individual contrast sensitivity functions from acuity and letter contrast sensitivity measurements. J Vision. 2016;16(15):1-15. 4. Brilliant, Richard L. Essentials of Low Vision Practice. Butterworth-Heinemann, 1999. 5. Shandiz FH, Derakhshan A, Daneshyar A, et al. Effect of cataract type and severity on visual acuity and contrast sensitivity. J Ophthalmic Vis Res. 2011;6(1):26-31. 6. Bambo MP, Ferrandes B, Guerri N, et al. Evaluation of contrast sensitivity, chromatic vision, and reading ability in patients with primary open angle glaucoma. J Ophthalmol. 2016;2016:7074016. 7. Fatehi N, Nowroozizadeh S, Henry S, et al. Association of structural and functional measures with contrast sensitivity in glaucoma. Am J Ophthalmol. 2017 Jun;178:129-39. |

