 |
A 66-year-old female established patient sent a message via her electronic health review saying she started seeing a new onset of floaters in her left eye for the past four days and wanted to know if she should be seen in-person for an eye exam. The message was read the next day, and she came in two days later. A review of her medical record showed that she had been seen almost 18 months prior. At that visit, she was noted to have resolving Bell’s palsy on the right side and posterior vitreous detachment (PVD) in both eyes. Besides the PVDs, her retinal exam was unremarkable.
On this most recent examination, her best-corrected visual acuity measured 20/20 OD and 20/40 OS. Extraocular motility testing was normal. Confrontation visual fields were full-to-careful finger counting OU. Her pupils were equally round and reactive to light; there was no afferent pupillary defect. The anterior segment examination was unremarkable.
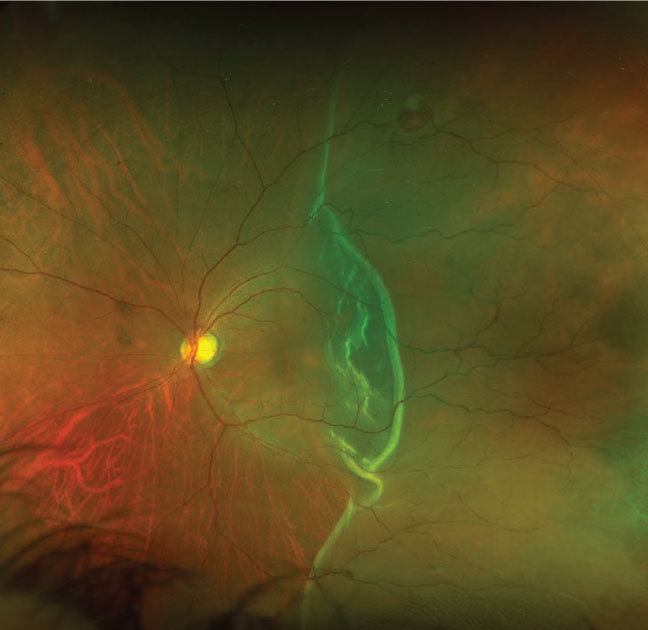
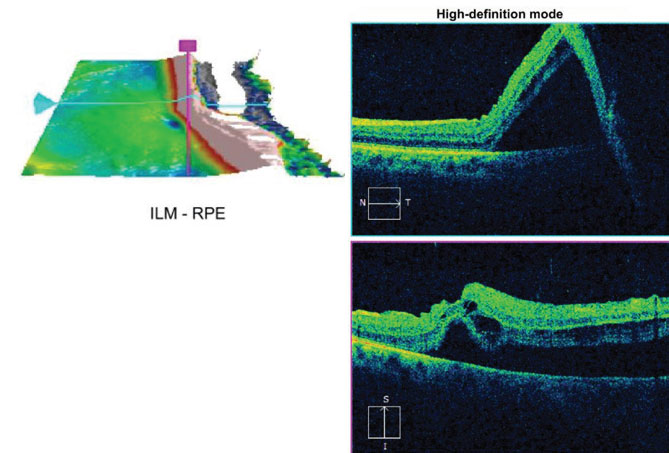
Fundus examination of the right eye was normal. A PVD was present. In the left eye, a PVD was also present in addition to pigment cells in the anterior vitreous. There were obvious fundus changes (Figure 1). OCT was performed and is available for review (Figure 2).
Take the Retina Quiz
 |
|
Fig. 1. This is the widefield fundus photo of the left eye of our patient. What does this finding represent? Click image to enlarge. |
1. What is the correct diagnosis?
a. Rhegmatogenous retinal detachment
b. Exudative retinal detachment
c. Retinal pigment epithelium (RPE) tear
d. Chronic retinal detachment with subretinal fibrosis
2. How would you characterize the macula?
a. Macula is on
b. Macula is off
c. Splitting fixation
d. There is a macular schisis
3. How should this patient be managed?
a. Observation
b. Pars plana vitrectomy (PPV), endo laser and possible scleral buckle procedure (SBP)
c. Injection of gas and laser photocoagulation
d. Surgical retinotomy and gas fluid exchange
4. What is the time frame that this needs to be treated before it affects the final visual outcome?
a. Within 24 hours
b. Within 3 days
c. Within 7 days
d. Within 14 days
5. What is the likely visual outcome at this point?
a. Likely 20/20
b. Between 20/25 and 20/50
c. Between 20/60 and 20/200
d. Worse than 20/200
For answers, see below.
Discussion
 |
|
Fig. 2. How do you interpret this OCT scan through the macula? Click image to enlarge. |
Our patient has a macula-off rhegmatogenous retinal detachment. A retinal tear can be seen along the superior temporal arcade. The OCT confirms the macula is off, but just barely. In fact, the macula may still be on temporally, but it is clearly off superiorly where we can see fluid and separation of the retinal from the RPE. Despite being macula-off, visual acuity was surprisingly good, which likely indicates that the macula has not been off for very long.
There are a few interesting questions to consider. Why did she develop a retinal tear after already having had a PVD? The assumption is that every tractional force occurring on the retina is relieved after developing a PVD, but that’s not always the case because the vitreous can still be attached anteriorly, causing traction. That is clearly what has occurred in our patient.
Horseshoe tears most commonly develop as a result of traction at the posterior margin of the vitreous base. The base represents a circumferential zone where the vitreous is attached to the peripheral retina. It measures about 2mm to 6mm wide and straddles the ora serrata. The adhesion of the vitreous at the peripheral retina is usually evenly distributed circumferentially.
Through the natural aging process, the vitreous begins to liquefy, and irregularities develop in the shape and extent of where it attaches to the retina. This, in turn, may result in isolated areas of focal traction on the retina that may result in the development of a horseshoe tear. It is believed that these irregular focal adhesions are responsible for a majority of retinal tears not associated with lattice degeneration.1
Don’t Delay
It’s clear the patient needs surgery to repair the retinal detachment, but how quickly does this need to occur? Does it need to be done on the same day (that we diagnosed the retinal detachment) or can it wait until the next day or even the day after? This becomes particularly important in the era of COVID-19, where surgical patients must be tested for the virus and negative prior to surgery. This could possibly result in a delay. At what point does waiting compromise the visual outcome?
There are a number of predictive factors for poor visual outcomes of macula-off retinal detachment. These include the initial presenting visual acuity, duration of the macular detachment and height of the retinal detachment. Obviously, worse acuity, longer duration of the detachment and more bullous detachments are all associated with worse visual outcomes.
For our patient, we don’t know how long she has had the retinal detachment, but her symptoms probably give us a good clue—i.e., from the time her symptoms began until she was seen and diagnosed was seven days. We also don’t know how long the macula has been off, but based on her reasonably good acuity and the OCT findings, it hasn’t been more than a day or two. These are all great prognostic indicators for a good visual outcome.
A number of studies have tried to determine optimal timing for repair of macula-off retinal detachments. Most have shown the best visual outcomes are achieved when the surgery is performed within seven days of the macular detachment.2,3 However, the window of opportunity for optimal visual success may be less than that. One meta-analysis found that a delay of more than three days was associated with statistically worse final visual outcome. Eyes that had surgery within three days averaged a final visual acuity of around 20/30, whereas eyes that were operated on between four and seven days averaged a final visual acuity of around 20/70.4
Our patient was referred to a retina specialist and seen the same day. She was tested at that visit for COVID-19 using real-time reverse-transcriptase PCR assay (SARS-CoV-2 DiaSorin Simplexa assay) and was negative. She had surgery the following day via PPV, injection of 16% C3F8 gas and endo laser without a scleral buckle.
This process took under three days, which should give her the best opportunity for achieving optimal visual success. She will likely not see immediate results, as she will likely develop a cataract from the surgery and gas injection, which will ultimately result in needing cataract surgery.
On day one post-op, her retina was attached. By week three, she was able to pinhole to 20/60, but she still had a gas bubble present and she was well on her way to developing a cataract. We will continue to follow her.
Retina Quiz Answers
1) a; 2) b; 3) b; 4) b; 5) b.
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
| 1. Wilkinson CP, Rice TA. Michels’ retinal detachment, 2nd edition. St. Louis: Mosby; 1997:935-977. 2. Burton TC. Recovery of visual acuity after retinal detachment involving the macula. Trans Am Ophthalmol Soc. 1982;80:475-97. 3. van Bussel EM, van der Valk R, Bijlsma WR, et al. Impact of duration of macula-off retinal detachment on visual outcome: a systematic review and meta-analysis of literature. Retina. 2014;34:1917-25. 4. Greven, MA, Leng T, Silva RA, et al. Reductions in final visual acuity occur even within the first 3 days after a macula-off retinal detachment. Br J Ophthalmol. 2019;103:1503-6. |

