 |
A 16-year-old Hispanic male presented with a sudden and painless onset of blurred vision in the right eye for the past two weeks. His social history was remarkable for recent travel to Nicaragua, but his medical history was unremarkable. An examination revealed his best-corrected vision was 20/25 OD and 20/20 OS. His extraocular motility was normal, and confrontation visual fields were full-to-careful finger counting. The pupils were equally round and reactive; there was no afferent pupillary defect. An exam of the anterior segment was remarkable for keratic precipitates (KP) on the endothelium in the right eye and 1+ cell in the anterior chamber. The left eye was unremarkable.
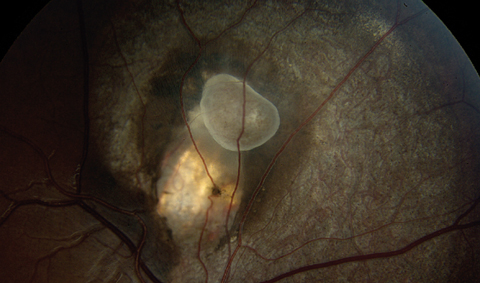
A dilated fundus exam of the right eye showed 1-2+ vitreous cells. The optic nerve and macula appeared healthy. Of interest was an elevated lesion superior to the nerve as seen in the fundus photo (Figure 1). A spectral-domain optical coherence tomography (SD-OCT) is available for review (Figure 2).
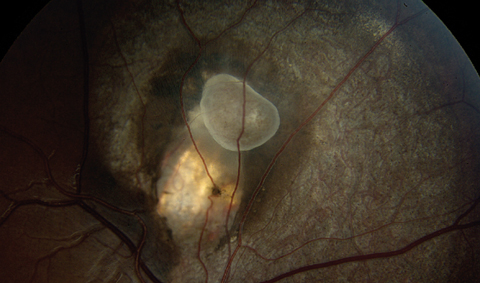  |
| Fig. 1. Fundus photo of the right eye showing the area of interest. What does this represent? Click image to enlarge. |
Take the Retina Quiz
1. How would you characterize the OCT image of this patient?
a. Intraretinal cyst.
b. Hemorrhagic RPE detachment.
c. Sub-retinal pigment epithelium (RPE) hyperreflective lesion with fluid.
d. Exudative retinal detachment.
2. How would you best characterize the fundus changes seen in this patient?
a. Inflammatory.
b. Infectious.
c. Congenital.
d. Traumatic.
3. What is this patient’s most likely diagnosis?
a. Toxocariasis.
b. Toxoplasmosis.
c. Cysticercosis.
d. Treponema pallidum (syphilis).
4. How should this patient be managed?
a. Placed on Bactrim and monitored.
b. Referred for surgical removal.
c. Panretinal photocoagulation.
d. Penicillin.
For answers, see below.
Diagnosis
The lesion superior to the nasal appeared to be a subretinal cyst with adjacent subretinal fluid surrounding it. We also observed chorioretinal scaring and atrophy surrounding the cyst. This was confirmed on the SD-OCT, which shows well delineation of the cystic lesion in the subretinal space along with fluid and exudates.
The patient admitted to having recently traveled to Nicaragua. He also admitted to eating uncooked pork. Given this history, the anterior chamber and vitreous cells, and OCT findings, we made a tentative diagnosis of cysticercosis.
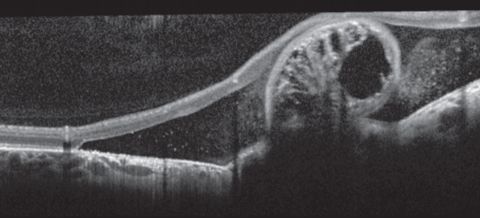 |
| Fig. 2. The above SD-OCT image shows the lesion. |
Discussion
Cysticercosis is the most common parasitic disease of the central nervous system, affecting the eye, muscle and subcutaneous tissue.1 It is caused by encystment of the tapeworm Taenia solium from uncooked pork meat.1,2 It is believed that the larvae travels from the choroid through the RPE and either encysts in the vitreous or subretinal space.2
In the ocular form, it typically presents unilaterally, affects young individuals in the second to fourth decade of life and is endemic in developing countries.1 In severe cases, anterior and posterior inflammation is present and vision is greatly reduced due to exudative retinal detachment.2 Rarely, vitreous hemorrhage can occur if the cyst migrates through the retina into the vitreous.2 Systemically, neurocysticercosis is the most serious of this condition’s sequela.2 Neurological findings are most commonly seizures and hydrocephalus.2
Upon close comparison of our high-definition OCT with histopathological slides of cysticercosis, we were able to definitively characterize that the double-layered cyst wall is evident (Figure 3a). The scolex, which represents the knoblike anterior end of the tapeworm, can also be seen but is more difficult to visualize. We suspect our imaging captured the outline of the cyst (Figure 3b). The honeycomb invagination within the cyst is the intestine of the larvae (Figure 3c).3,4
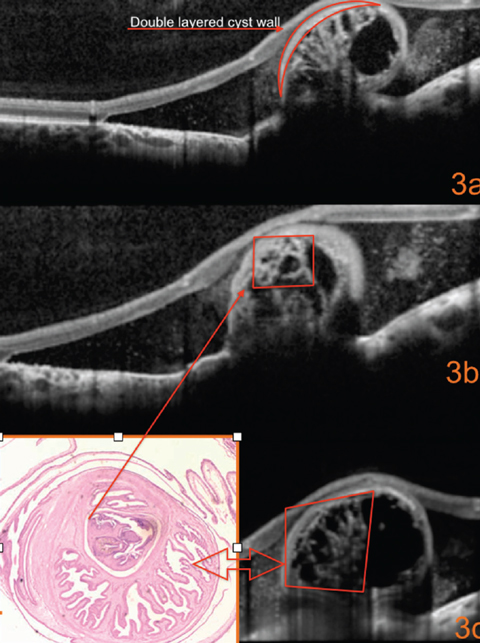 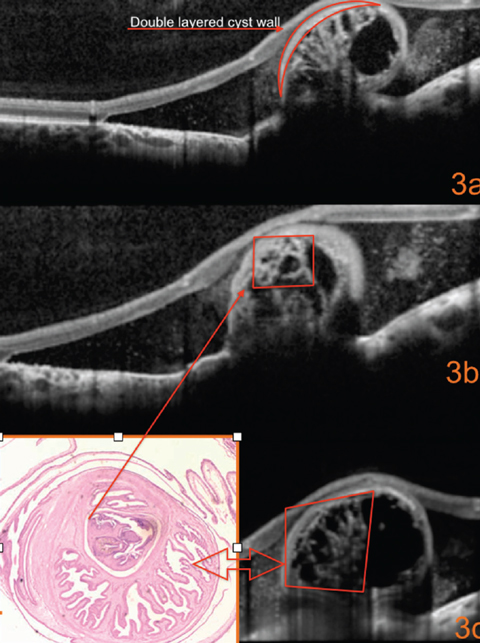 |
| Fig. 3. What can this detailed look at the SD-OCT image reveal? Click image to enlarge. |
Treatment
The management of ocular cysticercosis consists of prompt referral to a retina specialist for consideration of surgical removal of the cyst and treatment of the retinal detachment, if present. All patients we suspect have this condition should undergo a serology work up for toxocariasis and toxoplasmosis, as well as a full blood panel to rule out systemic involvement. Serologic testing for our patient was obtained and was negative for active cysticercosis infection and also negative for toxoplasmosis infection. The negative testing likely indicates the patient may have had this for some time even though he only recently became symptomatic. Some of the clinical findings such as RPE mottling and atrophy also suggest this has been present longer than his symptoms would have indicated.
Systemic treatment for neurocysticercosis involves anthelminthic therapy; however, this treatment may be contraindicated if an active ocular infection is present.4 Our patient underwent magnetic resonance imaging to rule out neurological involvement prior to coming in for his retinal exam, and the results were normal.
Visual prognosis for these patients is good if it does not involve the macula, and is typically restored to normal once the cyst is removed and the patient’s condition is treated systemically. Recurrence is uncommon.
Proper follow up is warranted postoperatively, as with any surgery. Lastly, the best method of prevention is to thoroughly cook pork and use proper hygiene when handling meat.
Our patient underwent pars plana vitrectomy, removal of the cyst and was treated for retinal detachment. One month post-surgery, his vision returned to baseline of 20/25 without correction. The pathology report confirmed the presence of the cyst in the specimen removed. He did not require anthelminthics, as he was not affected systemically.
Dr. Edriskhalaf is a former optometric resident at the Bascom Palmer Eye Institute in Miami, FL.
1. Dhiman R, Devi S, Duraipand K, et al. Cysticercosis of the eye. Int J Ophthalmol. 2017;10(8):1319-24. |

