 |
Q: One of my keratoconus patients will need cataract surgery in the near future. Her topography shows classic inferior steepening with a relatively “normal” central cornea with moderate astigmatism on her Pentacam image. How do you best decide who might do well with a toric IOL option?
A: Paying close attention to the patient’s corneal topography is key to selecting a toric IOL.
“Cataract surgery—and specifically IOL selection—in keratoconus patients can be challenging. These patients often have steeper corneas and their astigmatism has varying degrees of irregularity, which makes predicting the correct magnitude and axis for toric IOL placement difficult,” says Eric Donnenfeld, MD, a Long Island ophthalmologist who specializes in refractive cataract surgery.
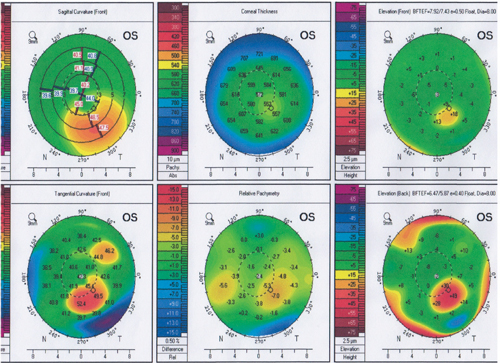
In the case of this particular patient, toric IOL implantation is possible because the ectasia pattern avoids the central cornea, says Martin Fox, MD, who serves as medical director at the Cornea and Refractive Surgery Practice of New York. However, he cautions, clinicians should adhere to a few conditions.
|
|
| A Pentacam image of a keratoconus patient. Depending on corneal topography, these patients can do well with toric IOLs. Photo: Dr. Martin Fox, MD |
|
First, the patient must have a history of reasonably good spectacle-corrected visual acuity with moderate levels of astigmatism. If this condition is not met, the patient is unlikely to do well with the IOL, Dr. Fox explains. Additionally, when evaluating the patient’s astigmatism, axis and corneal power should be the same when measured using both manual keratometry and elevation tomography. Any difference in measurements likely indicates the astigmatism is too irregular and could result in the lens being implanted in an inappropriate position.
These patients should instead be managed with standard monofocal intraocular lenses and then subsequently fit with a soft or GP contact lens to address residual refractive errors, says Dr. Fox. In any case, he adds, doctors should avoid multifocal IOL implants in all patients with confirmed keratoconus.
Dr. Donnenfeld says he generally prefers to avoid performing incisional surgery on patients who already have ectatic disease, but recommends evaluating a keratoconic patient using refraction and topography (or keratometry)—a toric IOL will generally do well if the axis of cylinder is the same with regards to both refraction and either topography or keratometry. If the axis is not the same, he suggests using a zero aberration IOL instead.
Both surgeons agree: some of the challenge in selecting an IOL starts with cataract removal. They each recommend steps to improve the procedure to make IOL implementation easier. Dr. Donnenfeld suggests considering first performing Intacs to reduce and regularize the cylinder. “In the very near future, topographic ablations will be available in the United States,” he says. “That can help improve the corneal topography and improve post-cataract surgery visual rehabilitation.”
Dr. Fox suggests a two-step approach when faced with a highly irregular cornea and cataract. “Femtosecond laser keratoplasty (FLAK) should be performed as a first measure, with cataract surgery to follow after adequate corneal stabilization,” he says. FLAK is associated with rapid corneal healing with low levels of astigmatism, and “our patients have been able to move forward with follow-up cataract as early as three months post-corneal surgery, with excellent results.”
