Uncompromised presbyopia correction seems to be as elusive as ever, despite a growing population seeking these therapies. The global number of patients with presbyopia is expected to be approximately 1.4 billion by now, and many remain unsatisfied with the currently available options.1,2 Researchers, innovators and manufacturers are forging ahead with a number of new technologies for every form of correction, including spectacles, contact lenses, intraocular lenses (IOLs), surgical treatments and pharmaceuticals. Here’s a look at what’s new in your armamentarium and what might be available in the future.
New Angle, Age-old Problem
Today’s US presbyopic population is significantly different from 20 years ago. The Baby Boomer generation (ages 52 to 70) wants to feel and look more youthful and is working much later in life. In addition, digital devices are creating new visual demands we need to address. The majority of these patients, 63.9%, report symptoms of digital eye strain.3 Even among Generation Xers (ages 36 to 51), 65% spend more than five hours per day on digital devices, with 66% experiencing symptoms of digital eye strain.3 This phenomenon may partially explain why we are seeing presbyopic symptoms at younger ages.
 |
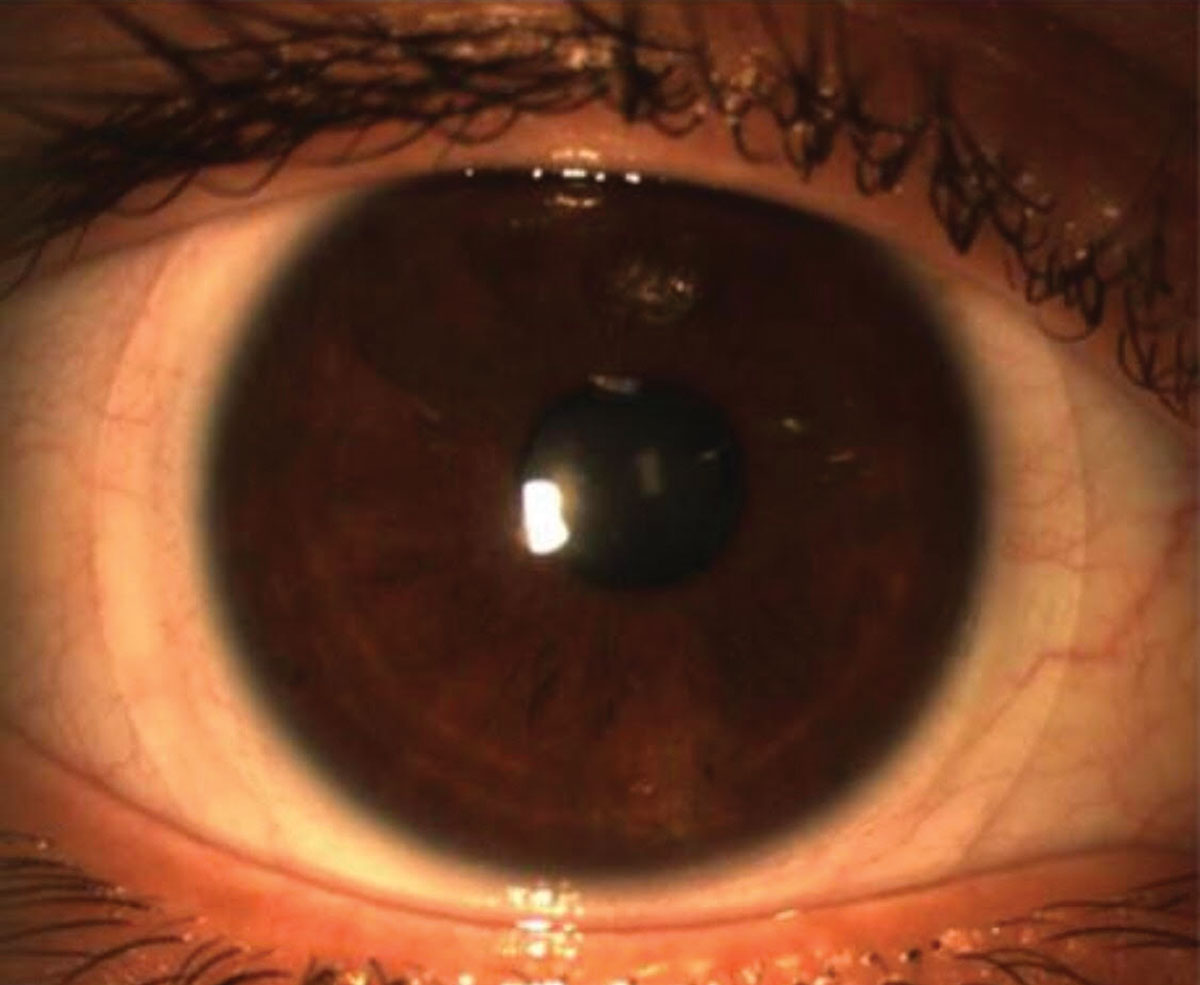
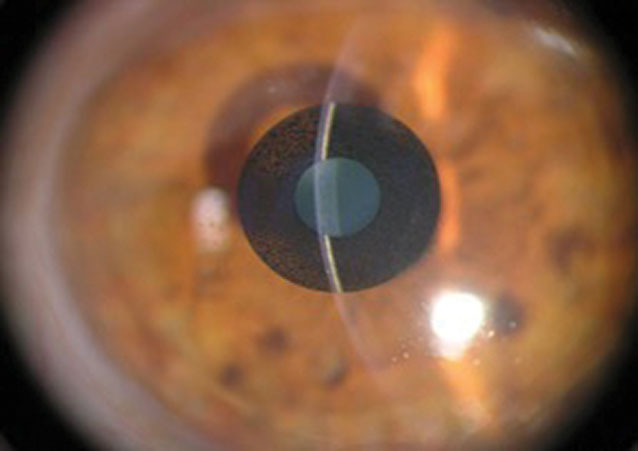
| So far, patients seem to like the range of vision provided by the new trifocal PanOptix IOL. Photo: Cecelia Koetting, OD. Click image to enlarge. |
Many presbyopes are grappling with the psychological effects of getting older and struggling with their vision, possibly more so than in the past as a result of the ubiquitous presence of digital devices. One study found that presbyopia was associated with worse vision-related quality of life than emmetropia in younger individuals.4
As such, presbyopes face a host of issues when they visit our offices looking for a solution—and we need to be ready to meet the demand with new and creative solutions.
Currently, we employ several means of correcting presbyopia: spectacles, monovision and multifocal contact lenses, IOLs with reading glasses, monovision and multifocal IOLs and corneal inlays. Despite ever-improving multifocal options, monovision is still the most common way doctors treat their patients to correct presbyopia.5 For contact lenses, only about 12% of presbyopic fits are with a multifocal design. As for IOLs, only about 8% of surgeries are done with a presbyopia-correcting lens.6 Some feel multifocal and trifocal designs take up too much chair time, while others do not feel they provide adequate vision for the patients.7 Many just can’t break longstanding habits. However, doctors should recommend these options with regularity, as they can provide significant benefits to the right patients.
Contact Lenses of Today
Multifocal contact lens designs continue to evolve. We now have several designs that allow our patients the freedom of spectacle-free vision most of the time. For example, Bausch + Lomb recently introduced the first off-the-shelf toric multifocal, Ultra Multifocal for Astigmatism, for patients who are presbyopic with astigmatism.
Most of the current multifocal contact lens designs use aspheric optics to achieve near acuity, making lens centration critical to allow the optics to work properly. While these designs do work, they are not ideal for every patient, as they require some optical compromise. Several new designs are in early development, but little information is available currently.
Some innovative designs under investigation include a water gradient lens to simulate an accommodative effect, thus allowing the patient more natural vision with a true full range. Another lens uses microelectrodes to allow for variable vision. Many of the larger contact lens companies have started to partner with tech companies to help them develop new designs.
Scleral Multifocal Contact Lenses: The Search For ComfortBy Nitya Murthy, MSMany patients with presbyopia are looking to rid themselves of glasses for convenience and cosmetic reasons. Contact lenses are a great option, and for those already wearing contact lenses, multifocal contact lenses are a no-brainer. However, issues of comfort and quality of vision can thwart contact lens success in this population. In particular, symptoms of dryness, which increase with age, are the most challenging aspect of adapting to multifocal soft contact lens wear.1 This is where the resurgence of scleral contact lenses can be a valuable asset in our toolbox. Scleral multifocals are generally dismissed as opportunities for presbyopic patients for several reasons:
However, newer options have addressed most of these concerns. For example, various scleral lenses are now designed for normal corneas, with standard base curves and diameters that are compatible with most normal eyes. As for billing, insurance companies provide varying degrees of coverage. CPT code 92071 or V2627 may be covered by the patient’s insurance, while other vision insurance contact lens material fees may be used toward the cost of a scleral lens.2
The Pros Several common variations in fitting philosophies exist: Aspheric vs. concentric. Aspheric lenses have smooth power transitions throughout the lens between distance, intermediate and near powers and are a good option for presbyopes with low adds.4 Concentric designs have designated distance and near rings that alternate moving from the center to the periphery. Center-near vs. center-distance. These fall under the umbrella of concentric designs and perform as they are named. Generally, center-near designs are more common, given the prevalent demand for near-work at mobile device distances. However, center-distance designs are more appropriate for emerging presbyopes and those who prefer to have better distance acuity.4 Practitioners can choose the best lens design based on the patient’s lifestyle needs. Most scleral lens manufacturers offer myriad variations in these designs and include fitting guides to help align the power zones with the patient’s pupil. Scleral lenses provide many invaluable advantages, and fitting them is easier than ever before. We must offer our presbyopic patients all lens options so they can choose the lens that best suits them—which just might be a scleral. Ms. Murthy is a 4th year student at Kentucky College of Optometry (KYCO) and president of the KYCO Contact Lens Society.
|
IOLs in the Works
In addition to recommending an IOL during cataract surgery, clinicians can consider clear lens extraction for patients, usually older than 55, looking for a refractive surgery option. Although many of these patients come into the office for a LASIK consultation, the lens changes that will occur over the next decade make a clear lens exchange a reasonable alternative. During a clear lens exchange, the surgeon removes the crystalline lens prior to cataract formation.
Patients considering an IOL have several presbyopia correction options: they can obtain the best distance vision possible and use readers for near, implant an IOL focused at near for monovision or choose an advanced technology IOL, whether accommodative or multifocal.
Though many patients could benefit from a presbyopia-correcting IOL, only about 12% of IOLs implanted are of the advanced technology type (including toric IOLs).6 Surgeons have been slow to embrace this technology, and referring ODs have been equally hesitant to recommend them—whether out of habit or because they question the lens’s performance.
However, optometry plays a vital role in this decision. We typically have a longstanding relationship with the patient and know their visual needs. For example, a patient corrected with multifocal contact lenses will likely do well with a multifocal IOL and may not be happy with a single-vision IOL. We need to be more proactive in our recommendations to give the patient all their options.
The approved IOLs for presbyopia can be either accommodative or multifocal. The only approved accommodative IOL is the Crystalens (Bausch + Lomb), which remains relatively less popular due to its unpredictable near vision. Two multifocal IOLs approved in the United States include the Tecnis Symfony (Johnson & Johnson Vision) and the Restor (Alcon). These IOLs come in a variety of add powers and have had good success with some side effects, the most common being halo and glare with limited range of clear vision.
The newest IOL in the United States is Alcon’s AcrySof IQ PanOptix. This trifocal lens, designed to provide near, intermediate and distance vision, has been used successfully outside the United States for a few years. So far, the reports are quite encouraging for this lens, as patients say they like the range of vision and have little glare.
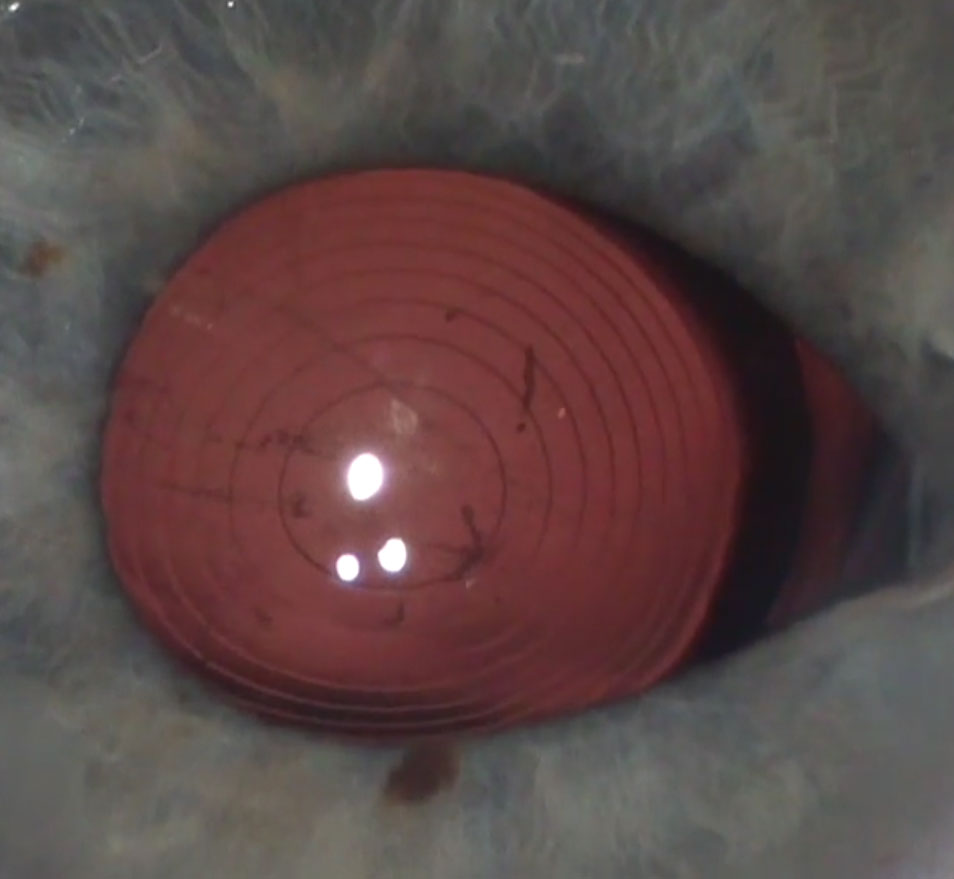 |
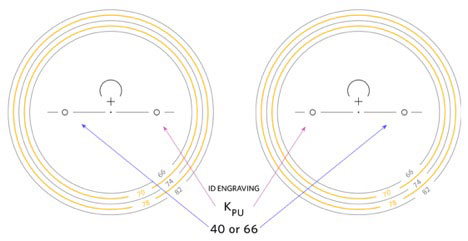
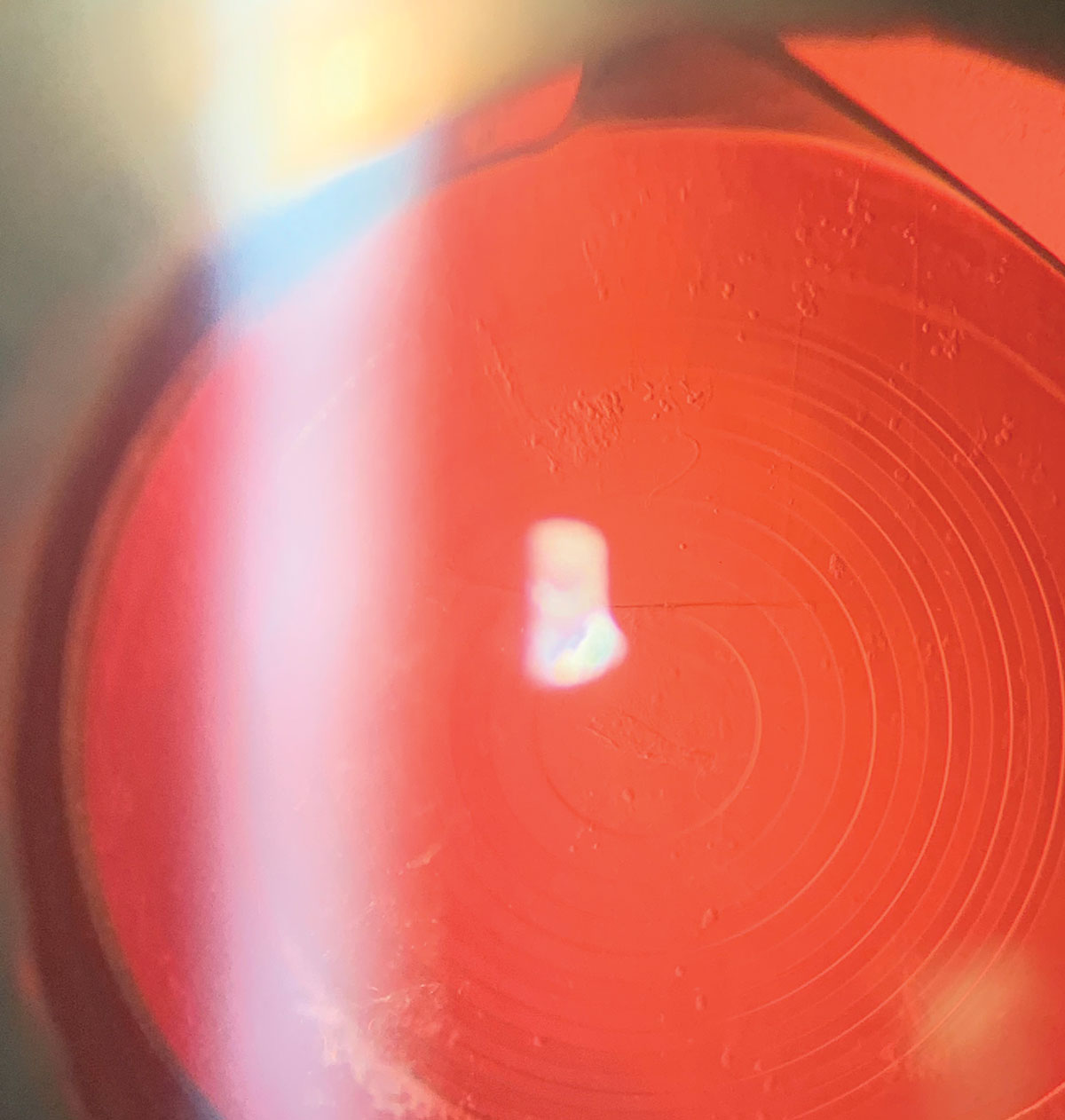
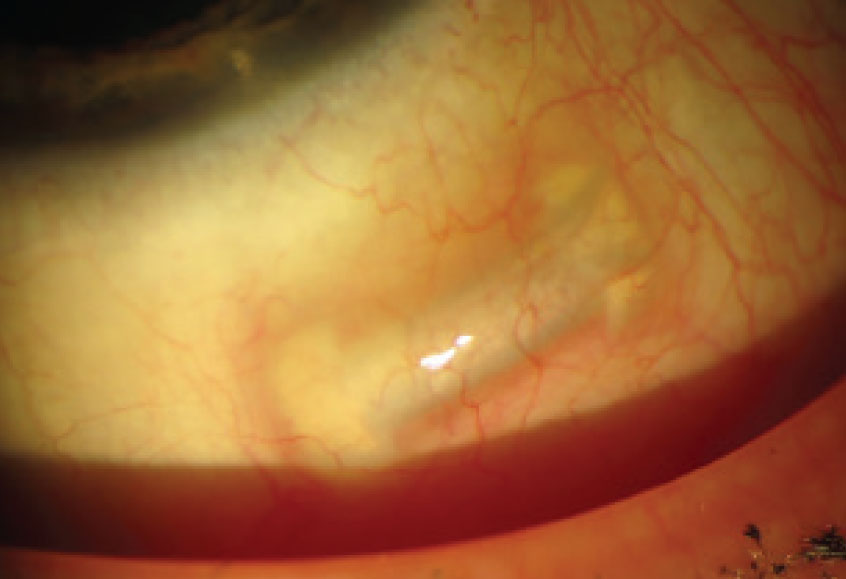
| The Symfony IOL uses refractive echelettes that appear similar to the concentric rings of a multifocal but diffract rather than split the light entering the eye. Photo: Derek Cunningham, OD, and Walter Whitley, OD. Click image to enlarge. |
Several new IOLs are potentially coming to the US market soon:
The RxSight light adjustable IOL has been approved in the United States but has yet to hit the overall market. It should be widely available early this year. The lens is a 6mm silicone optic with a PMMA haptic. The IOL material is modifiable until it is “fixed” by ultraviolet (UV) light, meaning the doctor can adjust the prescription to meet the patient’s needs after the initial implantation. The lens can also be modified to change the amount of asphericity, thereby creating a multifocal effect. If near vision is not adequate or the patient doesn’t like the vision it initially provides, you can modify it. The patient needs to avoid UV exposure until the final Rx is established, so they must wear UV-blocking glasses until then.
The AT Lisa (Zeiss) refractive-diffractive hybrid lens has both toric and nontoric versions and a 3.75D add.8 It directs light to one focal point for near and another for distance, and uses simultaneous images to which the patient needs to neuro-adapt. This lens splits the light by using 65% for distance and 35% for near. The design uses concentric diffractive rings that are rounded to reduce halo and glare. The lens has 0.11μm of negative spherical aberration. The lens gets good reports for distance and near vision but may lack in the intermediate area.9
The Lentis Mplus (Oculentis) is a one-piece zonal refractive lens with plate haptic and two refractive segments. The design has a large aspheric distance-vision zone and a sector-shaped zone with 3.00D of near add embedded on the posterior surface.10 The big advantage of this bifocal IOL is that it provides good distance vision.11 A large distance optic zone ensures good contrast sensitivity and reduced glare and halos. Some patients may notice ghost images, as the design also uses simultaneous vision.12,13 Patients can read with this lens in any direction of gaze and do not need to look down as with bifocal spectacles. Some patients do not achieve the near vision they expect, and the intermediate vision may not be good enough for some patients.11
The Fine Vision (PhysIOL) is a trifocal diffractive IOL that uses constructive interference to capture light energy that other diffractive lenses lose. The lens has 3.50D power for near and 1.75D for intermediate vision. Its main advantage is that it can provide intermediate acuity, which is especially useful for digital device use. The lens surface is microlathed in an alternating pattern from the center to periphery. The lens uses constructive interference to increase the amount of light used for each focal point.10 The lens has not had a lot of market tests yet, but early results have been positive.
With the FluidVision IOL (PowerVision), silicone fluid is stored in the soft haptics and accommodative effort forces the fluid to move into the central fluid chambers. This changes the shape of the anterior optic and shifts the eye’s focus to near. Still in early studies, this lens could provide as much as 5.00D of accommodation.14
The Dynacurve IOL (NuLens) is implanted in front of the collapsed capsular bag. The capsule exerts pressure from the ciliary muscle to move the fluid and modify the shape of the optic to cause an accommodative effect. In theory, the researchers say this lens could provide up to 12.00D of accommodation.15
Perfect Lens is not a lens per se but rather a technology designed to modify nearly any pre-existing in situ IOL using a femtosecond laser. The laser can create a multifocal effect of bifocal or trifocal design. If necessary, the lens can be changed several times to achieve the best vision.16
The Gemini Refractive Capsule (Omega Ophthalmics) is not an IOL but a capsular ring that, when inserted into the capsular bag, maintains the original size and shape of the bag. This ensures the proper lens position. This design controls the x/y plane of the eye and helps control the z plane. The ring allows the surgeon to implant most any IOL into it to achieve the best refractive result. Because this ring keeps the capsule bag intact, you should be able to replace the IOL if a better lens becomes available.
The IC-8 small aperture IOL (Acufocus) is another option currently approved in Europe. The lens is designed to extend the eye’s depth of focus by combining a small aperture with a monofocal lens. A retrospective case series conducted in Australia found more than 90% of healthy participants achieved uncorrected distance, intermediate and near visual acuity of 6/12 or better in the corrected eye. The researchers noted that more than half remained spectacle-free for all distances at final follow-up, and those who used spectacles did so only for certain needs such as near-vision tasks and reading in poor lighting.17
Spectacle Lenses for Presbyopia: Shifting FocusGlasses are still the go-to option for most presbyopes. It’s a mature field, technologically, but that doesn’t mean patients won’t have some futuristic options in the coming years. Here are just a few on the market or under development: Signet Armorlite recently released a new ophthalmic lens called Kodak PowerUp, which the company claims can partially acclimate patients to progressive addition lenses before they need them. The company says the product is particularly suited to the visual tasks of a digital, device-centric world by helping patients achieve prolonged, comfortable reading up close. Kodak PowerUp lenses offer two levels of power in the reading area: 0.40D and 0.66D.1
Researchers at Stanford have created what they are calling “autofocals”—eyewear that uses eye tracking technology to identify what the wearer is looking at and then adjust the focus accordingly. The device (the prototype of which looks like a bulky VR headset) incorporates fluid-filled lenses that bulge and thin when the field of vision changes, identified with eye-tracking sensors.2 All 56 presbyopes who used the device during preliminary testing were surprised at how well it performed with reading and other tasks.2 Adjustable focus spectacles are already available from several companies, including Adlens and Eyejusters.3-5 These ophthalmic lenses use dials on the sides of the frames to change the lens prescriptions based on the user’s needs. Adlens incorporates two thin lenses that slide by each other when the wearer shifts the knob, thus changing the power.3,5 Eyejusters have a range of +0.50D to +4.00D and allow users to change the power of each lens independently, providing more options for those with varying prescriptions in each eye.5 The 2005 startup PixelOptics may have filed for bankruptcy in 2013, but its Empower electronic lenses are still a hot topic in many forums as recently as September 2018.6,7 These battery-powered glasses used a liquid crystal reading segment that was activated based on head tilt or with a swipe of a hand. Little information exists on the product’s current availability. Several augmented reality options show promise in helping to correct presbyopia, although none are ready for the consumer market.8
|
Other Surgical Corrections
Several surgical approaches can address a presbyope’s needs:
Monovision with LASIK or photorefractive keratectomy has been employed for years, and we are well aware of the limitations of this technique. Presby-LASIK has fallen out of favor in the United States due to regression and unpredictability.
Likewise, conductive keratoplasty is rarely used due to regression.
Corneal inlays are an additive technology that can be removed in the event of patient dissatisfaction. The procedure does not remove any tissue, providing an opportunity to potentially employ future technologies.18 Although three companies went through FDA trials to get these devices to market, two have since gone out of business. The third device, the Kamra inlay (CorneaGen), is still a viable option. With this monovision technique, the inlay is placed in the nondominant eye, creating a pinhole pupil to increase the near eye’s depth of focus. The eye’s distance vision needs to be close to plano before the procedure. The inlay has not found a strong following and relatively few procedures are being done.
 |
| The Kamra inlay requires distance vision near plano before surgery. Photo: Vance Thompson, MD. Click image to enlarge. |
The other two inlays were the Raindrop (Revision Optics), which changed the corneal shape to create the near effect, and the Flexivue Microlens (Presbia), which provides distance vision through a central plano zone surrounded by one or more rings of varying powers for intermediate and near vision.19
The VisAbility insert (Refocus Group) is placed in four quadrants outside the visual axis in scleral tunnels. The bands are inserted in both eyes to create an increase in accommodative effect by allowing the ciliary muscle to exert more pressure on the lens. Studies show about a 1.50D increase in accommodation. The device is awaiting FDA approval and should be available in 2020. This technique will not have an effect on future cataract surgery.
 |
| The VisAbility scleral inserts represent a new concept in presbyopic surgery currently undergoing FDA trials. Photo: Refocus Group. Click image to enlarge. |
Drops on the Way
A pharmaceutical presbyopia management option might prove to be the Holy Grail clinicians and researchers have been looking for. Several are in the pipeline:
Yolia’s True Vision Treatment combines customized contact lenses and specially formulated eye drops to provide a noninvasive, binocular treatment for presbyopia. The drops soften the cornea to allow the rigid lenses to reshape the eye and then stabilize the new shape. This treatment adds asphericity to the corneal surface, creating a multifocal effect. The company is now doing clinicals in Mexico and the United States.
Novartis’s UNR-844 (formerly EV06) lipoic acid choline ester 1.5% is a prodrug that penetrates through the cornea and metabolizes into choline and lipoic acid. Enzymes within the lens fiber cells chemically reduce the lipoic acid to its active form dihydrolipoic acid. This chemically reduces disulfide bonds, ensuring the lens fibers remain flexible to allow for continued accommodation. This treatment is in early trials and not much data is available at this time.
The Liquid Vision (PRX-100, Presbyopia Therapies) drop contains aceclidine and low-dose tropicamide to create a miotic pupil without the accommodative effect. This results in a pinhole effect to increase the eye’s depth of focus. The drop is used once a day in the nondominant eye.
The CSF-1 drop (Orasis) is a parasympathomimetic agent with a nonsteroidal anti-inflammatory in an oil-based formulation that also causes a miotic pupil and increases the eye’s depth of focus. This option is currently in Phase II trials.
FOV Tears, currently available in Colombia, is a combination of a parasympathetic, alpha agonists 1 and 2, an anti-cholinesterase and an NSAID, according to Colombian researcher Felipe Vejarano, MD, a lead investigator for the drug. The drop affects the ciliary muscle, which causes a physiological accommodation and a dynamic pseudo-accommodation. Initial study results suggest the drop has a cumulative effect, lasting four to five hours initially, but can last up to eight hours with continual use.20 More recent data shows the drops improved near vision by one or more lines in 92.3% of the patients two hours after instillation, with a greater effect in the youngest patients compared with the oldest.21 The drop remains under investigation in Colombia and Spain.
Allergan’s AGN-199201 and AGN-190584, both miotic-based drops that work as pupil constrictor agents, remain in development. Early research found 70.6% of participants who first received one drop of AGN-190584 ophthalmic solution and one drop of the AGN-199201 vehicle in the nondominant eye and then two drops of AGN-199201 vehicle in the dominant eye experienced a two line or more improvement.22
Researchers have also investigated a combination of carbachol 3% and brimonidine 0.2% to create a miotic effect to improve vision in presbyopia. A pilot study of 10 naturally emmetropic and presbyopic subjects shows the monocular treatment with one drop a day of carbachol/brimonidine in the non-dominant eye provided statistically significant improvement in mean near visual acuity for all patients. The improved depth of focus caused a statistically significant improvement in near visual acuity, with no change in binocular distance vision, the study found.23
Many presbyopia correction options are under investigation, and some are more promising than others. No doubt the coming years will see new management strategies for this growing population in need, as we are embarking on entirely novel ways to treat this condition.
Dr. Geffen is the director of Optometric and Refractive Services at the Gordon Schanzlin New Vision Institute of TLC Laser Eye Centers in San Diego, CA. He is the immediate past president for the Optometric Cornea and Cataract Refractive Society.
1. Frick KD, Joy SM, Wilson DA, et al. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmology. 2015;122(8):1706-10. 2. Holden BA, Fricke TR, Ho SM, et al. Global vision impairment due to uncorrected presbyopia. Arch Ophthalmol. 2008;126(12):1731-9. 3. The Vision Council. 2016 Digital Eye Strain Report: eyes overexposed: the digital device dilemma. www.thevisioncouncil.org/content/digital-eye-strain. Accessed November 14, 2019. 4. McDonnell PJ, Lee P, Spritzer K, et al. Associations of presbyopia with vision-targeted health-related quality of life. Arch Ophthalmol. 2003;121(11):1577-81. 5. Goldberg DG, Goldberg MH, Shah R, et al. Pseudophakic mini-monovision: high patient satisfaction, reduced spectacle dependence, and low cost. BMC Ophthalmol. 2018;18(1):293. 6. OOSS IOL Survey Overview: Study shows new premium IOL adopters, lens preferences, and some likely trends for the future. Ophthalmology Management. 2017;21(May):16-18, 20. 7. American Optometric Association. Care of the Patient with Presbyopia. www.aoa.org/documents/optometrists/QRG-17.pdf. Accessed November 14, 2019. 8. Alio JL Plaza-Puche AB, Javaloy J, et al. Comparison of a new refractive multifocal intraocular lens with an inferior segmental near add and a diffractive multifocal intraocular lens. Ophthalmology. 2012;119(3):555-63. 9. Visser N, Nuijts RM, de Vries NE, et al. Visual outcomes and patient satisfaction after cataract surgery with toric multifocal intraocular lens implantation. J Cataract Refract Surg. 2011;37(11):2034-42. 10. Gatinel D, Pagnoulle C, Houbrechts Y, Gobin L. Design and qualification of a diffractive trifocal optical profile for intraocular lenses. J Cataract Refract Surg. 2011;37(11):2060-67. 11. Muñoz G, Albarrán-Diego C, Ferrer-Blasco T, et al. Visual function after bilateral implantation of a new zonal refractive aspheric multifocal intraocular lens. J Cataract Refract Surg. 2011;37(11):2043-52. 12. Santhiago MR, Wilson SE, Netto MV, et al. Modulation transfer function and optical quality after bilateral implantation of a +3.00 D versus a +4.00 D multifocal intraocular lens. J Cataract Refract Surg. 2012;38(2):215-20. 13. Hoffer KJ. Personal history in bifocal intraocular lenses. In: Maxwell A, Nordan LT, eds. Current Concepts of Multifocal Intraocular Lenses. Thorofare, NJ: Slack, Inc; 1991:127-32. 14. Alio JL, Ben-nun J, Rodríguez-Prats JL, Plaza AB. Visual and accommodative outcomes 1 year after implantation of an accommodating intraocular lens based on a new concept. J Cataract Refract Surg. 2009;35(10):1671-78. 15. Roux P. Early clinical results with PowerVision’s FluidVision IOL. Presented at the ASCRS Symposium on Cataract, IOL and Refractive Surgery; April 6, 2008, Chicago. 16. Perfect Lens. www.perfectlens.com/index.htm. Accessed November 14, 2019. 17. Hooshmand J, Allen P, Huynh T, et al. Small aperture IC-8 intraocular lens in cataract patients: achieving extended depth of focus through small aperture optics. Eye (Lond). 2019;33(7):1096-1103. 18. Wang M, et al. Surgical Correction of Presbyopia: The Fifth Wave. Thorofare, NJ: Slack, Inc; 2019. 19. FDA approves first-of-its-kind corneal implant to improve near vision in certain patients. www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm443471.htm. Accessed April 12, 2017. 20. Renna A, Vejarano LF, De La Cruz E, et al. Pharmacological treatment of presbyopia by novel binocularly instilled eye drops: A pilot study. Ophthalmol Ther. 2016;5(1):63-73. 21. Vargas V, Vejarano JLA. Near Vision improvement with the use of a new topical compound for presbyopia correction: a prospective, consecutive interventional non-comparative clinical study. Ophthalmol Ther. 2019;8(1):31-39. 22. Safety and efficacy of AGN-199201 and AGN-190584 in patients with presbyopia. clinicaltrials.gov/ct2/show/results/NCT02197806. Accessed December 12, 2019. 23. Abdelkader A, Kaufman HE. Clinical outcomes of combined versus separate carbachol and brimonidine drops in correcting presbyopia. Eye Vis (Lond). 2016 Dec 5;3:31. [Epub]. |