 |
A 24-year-old Hispanic female presented in consultation from her neurologist for intractable headache lasting three weeks, with a normal neurologic exam and blood pressure. Her history was positive for neck pain and transient “blackouts” in both eyes lasting less than 30 seconds. She was taking Avonex (interferon beta-1a, Biogen) for her MS. Her past ocular, family and social histories were unremarkable.
Her best-corrected acuities were 20/25 OU. Ocular motilities were full with no limitation. Pupil evaluation showed no afferent pupillary defect, and she was orthophoric in primary and lateral gaze in both eyes. She noted 10/10 color plates in each eye. Intraocular pressure (IOP) measured 18mm Hg OD and 16mm Hg OS. The anterior segment exam was unremarkable. Fundus exam showed bilateral blurring of the optic disc margins, peripapillary hemorrhages, absent venous pulsations and venous engorgement and tortuosity.
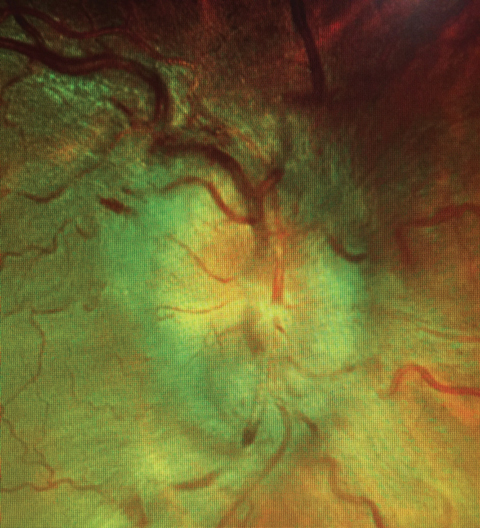 |
| Two years after an IIH bout, this patient returned with grade four papilledema. |
First Encounter
Because of her symptoms of transient visual obscurations, intractable headaches and neck pain, and in accordance with the findings of bilateral disc edema, we were concerned she was suffering from an intracranial process. We ordered fundus photography, spectral-domain optical coherence tomography (SD-OCT) and visual fields (VF). SD-OCT showed significant bilateral elevation of the retinal nerve fiber layer, and VF testing showed an enlargement of the physiologic blindspot and central-inferior hemifield defects OU.
Given her history and demographics, we formed a differential diagnosis of conditions that may result in elevated intracranial pressure (ICP): malignant hypertension, space-occupying mass, hemorrhage, infection, inflammation and, lastly, idiopathic intracranial hypertension (IIH)—also called pseudotumor cerebri—a diagnosis of exclusion.
Consequently, she was sent to the emergency department for emergent head computed tomography (CT) to discount intracranial pathologies such as hemorrhage, infection and mass lesion; her CT scan was unremarkable. She then underwent lumbar puncture (LP), which revealed an opening pressure of 550mm H2O and normal cerebrospinal fluid (CSF). Because a reading above 250mm H2O with normal CSF is consistent with intracranial hypertension secondary to IIH, she was diagnosed with IIH.1
After the patient was discharged from the hospital, we reviewed the laboratory tests to confirm there was no contraindication to starting her on acetazolamide; her potassium was within normal range between 3.5mEq/L to 5.0 mEq/L.2 We started her on acetazolamide 250mg twice daily and slowly titrated up to 500mg twice daily and discussed a low-sodium weight loss plan of one pound per week for 12 weeks.
The patient was monitored monthly, and over the next six months she lost 10 pounds. The headaches, disc edema and visual field testing improved dramatically. However, she was lost to follow up for the next two years.
Back for More
She recently returned with complaints of severe headache, pulsatile synchronous tinnitus and bilateral transient vision loss despite taking 250mg of acetazolamide daily and a net loss of 20 pounds since her last visit.
Ophthalmologic examination revealed recurrent, grade four papilledema. We ordered a metabolic panel to evaluate her potassium before increasing the dose of acetazolamide. The potassium level was 3.3mEq/L, which was slightly lower than the 3.5mEq/L cutoff value. She was instructed to follow up with her primary care physician for clearance. Once cleared, we increased her dosage to 500mg of acetazolamide twice daily.
She returned four weeks later with no improvement in symptoms. We then ordered magnetic resonance venography (MRV) due to the recurrent nature and severity of the papilledema. The MRV revealed narrow dural venous sinuses without frank stenosis or thrombosis. Given the recurrent, aggressive nature of the condition and her lack of proper follow up, we alerted her neurologist and admitted her to the hospital for electrolytes, therapeutic LP and intravenous mannitol. Neurosurgery then evaluated her for an intracranial shunt.
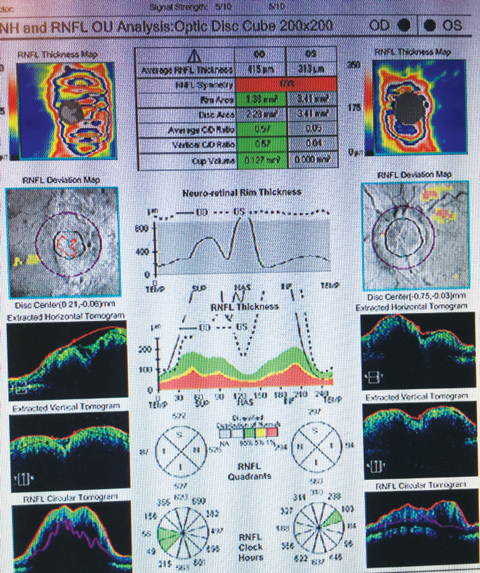 |
| Significant bilateral elevation of the nerve fiber layer can be seen on the patient’s OCT. |
Pseudo Tumor, Genuine Concerns
Even optometrists who see it infrequently know that papilledema is defined as bilateral disc edema secondary to increased ICP, and identification is often straightforward. To a clinician, the bigger challenge is determining what it signifies. Its pathophysiology involves axoplasmic stasis with swelling of axons and leakage.3 The increased pressure is transmitted along the subarachnoid space, leading to increased pressure within the optic nerve tissues and clinical disc edema. Histopathology of papilledema shows displacement of the retina away from the optic disc with serous sensory detachment within the peripapillary area.3
The most common general symptoms of pseudotumor cerebri include headaches in the morning that intensify with movement, projectile vomiting, neck pain, tinnitus (whooshing or ringing in the ears) and loss of consciousness. Ocular symptoms include blurred vision, transient visual obscuration, vision loss, retro-orbital pain and horizontal diplopia.4 Optic nerve findings include elevation of the disc with hyperemia, blurring of the disc margins, superficial retinal hemorrhages, edema of the peripapillary region, loss of venous pulsations, concentric retinal or chorioretinal folds around the optic nerve and macular exudates.4 Other findings include retinal vascular tortuosity and hemorrhages within the posterior pole and retinal periphery.4
Diagnostic criteria. IIH is diagnosed based on the modified Dandy criteria, which include: signs and symptoms of increased ICP, no localized neurologic findings, normal neuroimaging with the exception of an empty sella (dark appearance of the sella tursica on T1-weighted MRI from increased CSF), opening LP pressure of greater than 250mm H2O with normal CSF and no other causes of increased ICP.5
Grading. During clinical examination, it is important to initially grade the severity of papilledema to monitor the effects of therapy:6
Grade I: C-shaped halo of nerve fiber layer edema and blurred disc margins with a temporal gap.
Grade II: progressive circumferential edema and margin obscuration with blurring of the capillaries.
Grade III: Expanded nerve fiber layer edema and obscured major blood vessels as they leave the disc.
Grade IV: loss of major vessels on the disc.
Grade V: characteristics of grade IV plus partial or total obscuration of all vessels of the disc.6
Testing. Taking visual fields is necessary to monitor functional vision. According to research, over 90% of patients with papilledema had visual loss documented by perimetry.7 The most common visual field deficits include enlargement of the blind spot, inferior nasal depressions and peripheral constriction.8
After diagnosing bilateral disc edema, it is important to check the blood pressure to discount primary malignant hypertension or secondary hypertension from increased ICP. The next step is to send the patient to the local emergency department with the diagnosis and your recommendation for stat head CT, as well as LP—in the absence of intracranial pathology on neuroimaging—to record the opening pressure and check the CSF for pathology. CT is preferred over MRI in the emergency setting because it is readily available and quickly assesses for intracranial pathologies such as hemorrhages, space-occupying lesions, obstructive hydrocephalus and cerebral edema, all of which are neurologic emergencies.
In our case, we ordered MRV because the patient continued to show signs of intractable papilledema, headaches and tinnitus despite significant weight loss and long-term acetazolamide use. The MRV allowed us to discount abnormalities within the venous drainage system, identify potential additional causes for the recalcitrant nature of the condition, better establish a prognosis and determine whether surgical intervention was necessary. According to a recent study, MRV reveals bilateral narrowing of lateral sinuses in IIH, which is rarely seen in controls.9
OCT and fluorescein angiography (FA), in addition to recording the stage of papilledema, can be used to monitor the status of the disc during treatment. FA findings of the early phase of papilledema includes disc capillary dilation and leakage within the disc. Late findings show leakage beyond and pooling around the disc.10 On OCT, papilledema causes a hyporeflective space above the retinal pigment epithelium within the papillary space, representing serous sensory retinal detachment.11
Treatment. The key goal is to decrease ICP to help preserve vision and eliminate intractable headaches. Medical therapies include acetazolamide, oral glycerol, IV mannitol and weight reduction.
Acetazolamide is the treatment of choice to manage IIH.2 It reduces CSF production and flow from the choroid plexus. Prior to beginning therapy, a complete metabolic panel should be ordered to establish a baseline level of electrolytes and, if the results are concerning, consult with the patient’s primary care physician before administering the drug.
In one study, treatment with 250mg of acetazolamide, divided into four doses, was administered and then increased by 250mg per week to a maximum dosage of 4g/d until the papilledema grade was less than one in both eyes and the mean deviation on VF testing improved to equal to or better than -1dB in each eye.12 A low-sodium weight management plan should be implemented. Studies show as little as 6% weight loss is effective in improving signs and symptoms of ICP.13
During medical therapy, clinicians should measure the visual acuities, test the VFs and perform fundus photography, OCT and FA. Patients who do not show improvement in papilledema or systemic symptoms despite medical therapy and weight loss should be referred for neurosurgical consultation. Surgical treatment includes therapeutic LP, optic nerve decompression and intracranial shunting.
In IIH, medical management is necessary to preserve visual function and decrease systemic symptoms. Monthly follow up is recommended to test visual acuities, perform formal perimetry and record the grading of disc edema. In recurrent and refractory cases, consider MRV to discount venous sinus pathologies and better gauge prognosis. Patients who show narrowing of the venous system may follow a prolonged treatment course and require closer observation for surgery.
1. Corbett JJ, Mehta MP. Cerebrospinal fluid pressure in normal obese subjects and patients with pseudotumor cerebri. Neurology. 1983;33(10):1386-8. |

