 |
It’s debatable whether all acute isolated oculomotor cranial neuropathies, in patients older than 50 with or without vascular factors, should undergo neuroimaging.1-3 Here, we review cranial nerve (CN) three, four and six palsies and provide reasons for neuroimaging all isolated cranial mononeuropathies.
CN Three
The major functions of the third nerve are oculomotor and pupillomotor. Partial and complete third nerve palsies (TNPs) can be manifestations of ischemia in the setting of diabetes, hypertension and hyperlipidemia.4 Non-ischemic pathologies involving the oculomotor nerve include hemorrhagic stroke, primary and secondary neoplasm, aneurysm, cavernous malformation, infection and demyelinating disease.5
Third nerve palsies are clinically differentiated as either partial or complete and pupil-sparing vs. pupil-involving. According to one study, aneurysms are likely to affect pupillomotor fibers in complete TNP, but spare its function in superior division palsies.6 With regards to microvascular TNP, up to 20% of cases had pupil involvement.6 And, according to a second study, the relative presence of aneurysm as a cause of isolated TNP ranged from 14% to 56%.7,8 Finally, while evidence supports observation in complete isolated TNP without pupil involvement, numerous case reports exist implicating midbrain infarction, neoplasm, infection, vasculitis, pituitary apoplexy, aneurysm and carotid artery occlusion as causes of isolated and complete TNP.7
Our recommendation is to obtain emergent CT/CTA or MRI/MRA in all TNPs. In cases where noninvasive neuroimaging is negative and aneurysm is highly suspected, such as in partial TNP with pupil involvement, cerebral angiography should be performed and interpreted by a neuroradiologist before discounting an aneurysm.
 |
| This patient presented with an acute partial pupil-involved third nerve palsy from an aneurysm. The picture shows compete restriction of the right eye on upgaze. Click image to enlarge. |
CN Four
The most common causes of fourth nerve palsies (FNPs) are congenital, traumatic and vasculopathic. While isolated fourth nerve palsies in older individuals, especially with vascular disease, are most often ischemic in nature, additional etiologies include midbrain hemorrhage, pituitary macroadenoma, posterior fossa tumor, dural fistula, schwannoma and cavernoma of the fourth nerve.9-17
According to researchers, a small number of patients with isolated FNPs have trochlear nerve schwannomas.18 Additionally, one study describes a patient with an isolated FNP secondary to a cavernous meningioma, a second reports a patient with an intracavernous carotid artery aneurysm and a third study describes a patient with a carotid-cavernous fistula.19,20,13 Given these findings, it is certainly prudent to consider obtaining contrast-enhanced MRI of the brain with special attention to the cavernous sinus, since there seems to be an increased prevalence of cavernous sinus disease in non-ischemic FNPs.
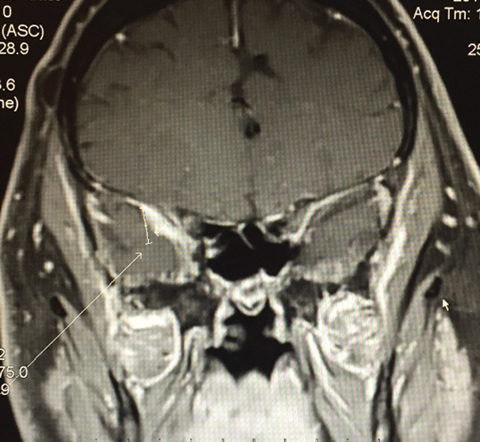 |
| This is an MRI of a 71-year-old white male who presented with an acute isolated right fourth nerve palsy. The MRI shows dural thickening abutting the cavernous sinus and possible compression of the fourth nerve within the cavernous sinus. Click image to enlarge. |
CN Six
Sixth nerve palsy (SNP) is the most common ocular motor nerve palsy due to its long subarachnoid course.21 According to researchers, the etiology of unilateral SNP is often attributed to ischemia, trauma, demyelinating disease, metastasis, aneurysm and intracranial hypertension, the latter of which can occur bilaterally.22
Because hypertension and diabetes are known etiologies of isolated SNPs in up to 35% of patients, some researchers argue that monthly follow-up is the best approach.23 The main disadvantage of these studies is the lack of brain MRI conducted during follow-up. Furthermore, one study concludes that significant evidence doesn’t exist in the literature to warrant observation-only management.24 A Medline literature search conducted by researchers reported 199 patients with isolated SNPs; 31 were traumatic, 42 vasculopathic, 43 “idiopathic;” 50 cases were related to tumors and the remainder were from miscellaneous causes (e.g., lumbar puncture, multiple sclerosis, immunization, infection, aneurysm, sarcoidosis, inflammatory, orbital amyloidosis and diverticulum of the cavernous sinus).25 A second study reported spontaneous recovery of SNPs in the presence of extramedullary compression by a tumor at the base of the brain.26
Ultimately, it’s our opinion that not enough evidence exists to support observation alone in isolated SNPs. It is reasonable to consider ordering contrast-enhanced MRI of the brain in patients with acute isolated SNPs; a previous study shows CT is not diagnostically beneficial.27
Until recently, no well-designed, randomized, prospective, controlled studies or prospective case series have been conducted. One study included patients with acute, non-traumatic, isolated ocular motor nerve palsies. Of the 66 patients followed, nine had significant causes; four patients with TNPs, two of which were pupil-involving, one patient with FNP, and four patients with SNPs. Excluding pupil-involving TNP, which is suggestive of aneurysm and routinely imaged, 11% of patients were identified as having a significant etiology, which were defined by the study as neoplasm, brainstem infarct, demyelinating disease and pituitary apoplexy. Subsequently, these patients were offered early medical and surgical management.28 It’s our opinion that sufficient data supports imaging all acute, isolated cranial nerve palsies regardless of the lack of associated neurologic symptoms.
| 1. Patel SV, Mutyala S, Leske DA, et al. Incidence, associations, and evaluation of sixth nerve palsy using a population-based method. Ophthalmology. 2004;111:369–75. 2. Bendszus M, Beck A, Koltzenburg M, et al. MRI in isolated sixth nerve palsies. Neuroradiology. 2001;43:742–5. 3. Tamhankar MA, Biousse V, Ying GS, et al. Isolated third, fourth, and sixth cranial nerve palsies from presumed microvascular versus other causes: a prospective study. Ophthalmology. 2013; 120(11):2264–2269. 4. Jacobson DM, McCanna TD, Layde PM. Risk factors for ischemic ocular motor nerve palsies. Arch Ophthalmol. 1994;112:961-6. 5. Bruce BB, Biousse V, Newman NJ. Third nerve palsies. Semin Neurol 2007; 27:257–68. 6. Trobe JD. Managing oculomotor nerve palsy. Arch Ophthalmol. 1998; 116:798-802. 7. Lee AG, Hayman LA, Brazis PW. The evaluation of isolated third nerve palsy revisited: an update on the evolving role of magnetic resonance, computed tomography, and catheter angiography. Surv Ophthalmol. 2002; 47:137-157. 8. Mathew MR, Teasdale E, McFadzean RM. Multidetector computed tomographic angiography in isolated third nerve palsy. Multidetector computed tomographic angiography in isolated third nerve palsy. 9. Galetta SL, Balcer LJ. Isolated fourth nerve palsy from midbrain hemorrhage: case report. J Neuroophthalmol. 1998; 18:204- 205. 10. Petermann SH, Newman NJ. Pituitary macroadenoma manifesting as an isolated fourth nerve palsy. Am J Ophthalmol. 1999; 127:235-236. 11. Krohel GB, Mansour AM, Petersen WL, et al. Isolated trochlear nerve palsy secondary to a juvenile pilocytic astrocytoma. J Clin Neuroophthalmol. 1982; 2:119-123. 12. Mielke C, Alexander MS, Anand N. Isolated bilateral trochlear nerve palsy as the first clinical sign of a metastatic [correction of metastasic] bronchial carcinoma. Am J Ophthalmol. 2001; 132(4):593-4. 13. Selky AK, Purvin VA. Isolated trochlear nerve palsy secondary to dural carotid-cavernous sinus fistula. J Neuroophthalmol. 1994; 14:52-54. 14. Feinberg AS, Newman NJ. Schwannoma in patients with isolated unilateral trochlear nerve palsy. Am J Ophthalmol. 1999; 127:183-188. 15. Maurice-Williams RS. Isolated schwannoma of the fourth cranial nerve: case report. J Neurol Neurosurg Psychiatry. 1989; 52:1442-1443.2001; 132:593-594. 16. Leibovitch I, Pakrou D, Selva D, et al. Neuro-ophthalmic manifestations of intracranial cavernous hemangiomas. Eur J Ophthalmol. 2006; 16:148-152. 17. Surucu O, Sure U, Mittelbronn M, et al. Cavernoma of the trochlear nerve. Clin Neurol Neurosurg. 2007; 109:791-793. 18. Feinberg AS1, Newman NJ. Schwannoma in patients with isolated unilateral trochlear nerve palsy. Am J Ophthalmol. 1999 Feb; 127(2):183-8. 19. Slavin M. Isolated trochlear nerve palsy secondary to cavernous sinus meningioma. Am J Ophthalmol. 1987; 104:433-4. 20. Arruga J, de Rivas P, Espinet H, Conesa G. Chronic isolated trochlear nerve palsy produced by intracavernous internal carotid artery aneurysm. J Clin Neuro-ophthalmol. 1991; 11:104-8. 21. Rosenberg RN. Comprehensive Neurology. New York: Raven Press, 1991. 22. Richards BW, Jones FR Jr, Younge BR. Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves. Am J Ophthalmol. 1992; 113(5):489–496. 23. Patel S. V., Mutyala S., Leske D. A. et al. Incidence, associations, and evaluation of sixth nerve palsy using a population-based method. Ophthalmology. 2004; 111:369-75. 24. Moster ML, Savino PJ, Sergott RC, et al. Isolated sixth-nerve palsies in younger adults. Arch Ophthalmol. 1984; 102:1328-30. 25. Miller RW et al. A Practice Pathway for the Initial Diagnostic Evaluation of Isolated Sixth Cranial Nerve Palsies. Med Decis Making. 1999; 19:42–48. 26. Volpe NJ, Lessell S. Remitting sixth nerve palsy in skull base tumors. Arch Opthalmol. 1993; 111:1391–5. 27. Nolan J. Diplopia. Br J Ophthalmol. 1968; 52:166-71. 28. Volpe N. The Work Up of Isolated Ocular Motor Palsy: Who to Scan and Why. http://content.lib.utah.edu/utils/getfile/collection/ehsl-nam/id/116/filename/7.pdf. 2009. Accessed Jun7, 2015. |

