Scope of Practice Battle Rages in NC
ODs in North Carolina may soon have the right to perform laser procedures.
By Rebecca Hepp, Managing Editor
North Carolina many soon join Oklahoma, Kentucky and Louisiana in allowing optometrists to perform select laser procedures. But H.B. 36, which could make it happen, is meeting with significant push-back from ophthalmologists, who raise concerns for patient health and safety.
The bill allows North Carolina ODs to perform procedures such as YAG capsulotomy, laser peripheral iridotomy, selective laser trabeculoplasty and removal and identification of skin lesions around the eye, according to Charles Sikes, OD, North Carolina Optometric Society (NCOS) PAC chairman.1
Many ODs recognize this as an inevitable expansion of optometry’s scope of practice. “It’s the next logical step for us,” says Randall Thomas, OD, who practices at the Cabarrus Eye Center in Concord, NC. “West Virginia was the first state to pass therapeutic legislation in 1976, and then it was just like a wave as other states passed similar laws. The next wave in optometric practice is laser procedures.”
Supporters of the bill hope its passage will increase access to eye care, provide patients with more convenient treatment options and reduce time and expense—all without compromising patient safety.
“We have a history now, in Louisiana, Oklahoma and Kentucky, of doing these procedures with virtually no negative outcomes,” says Jim Sandefur, OD, executive director of the Optometry Association of Louisiana. “In Louisiana, we require all of our doctors to report the number of procedures they have done each year in order to get relicensed, so we have an accurate number of how many procedures were done and their outcomes. In 2015, we did right around 2,000 procedures with zero negative outcomes.”
However, opponents also claim optometrists simply don’t have the training to safely perform laser procedures, but “that’s not exactly correct,” Dr. Sandefur says.
Laser procedures are part of the curriculum at optometry schools, said Jill Bryant, OD, president of the NCOS and who works for the National Board of Examiners in Optometry, in a press release. “We are proud of our education.”1
Dr. Bryant also said the NC Board of Optometry would form a credentialing committee to outline required training if the bill passes, and Dr. Thomas says the National Board of Examiners in Optometry is already including questions on laser procedures on the licensure exam for optometrists.
But if ODs already have the knowledge and skills, why is the bill under so much attack? According to Dr. Thomas, it’s about protecting one profession from another.
“The opposition from ophthalmology has nothing to do with protecting the public,” says Dr. Thomas. “It has to do with protecting their turf. Back when optometry gained the right to prescribe therapeutics in the ’70s, ophthalmologists said it would endanger the public, but that certainly hasn’t been the case, and the same will be true with these laser procedures.”
“The opposition always says the sky is falling when we have an expansion of scope bill, and yet they’ve always been wrong,” adds Dr. Sandefur. “Every one of them has been good for the people and has helped the people, and I think that’s the case here again.”
Despite significant optimism by optometrists in North Carolina, there’s still a lot of work ahead before the bill can pass.
“Optometry, for better or for worse, is a legislated profession,” Dr. Thomas says. “We need to ask for what’s right and truly patient-centric, because it’s all about the patient first. But if we are on the right side of the issue, and always have been, then you need to call your legislator, go by and visit with them and explain the true virtues of the issue.”
It will always be a battle, but one well-worth fighting, says Dr. Thomas. “Over the next 20 years, most, if not all, states will pass laser procedure laws,” he predicts. “It’s just how these things evolve.”
| 1. Bonner L. Surgeons don’t want optometrists laser-cutting eyes. The News & Observer. February 7, 2017. Available at www.newsobserver.com/news/politics-government/state-politics/article131198204.html. Accessed February 17, 2017. |
Newly Discovered Retinal Cell’s Link to Myopia
A retinal ganglion cell recently discovered by scientists may be linked to myopia in children who don’t spend enough time outside in natural light.1 The researchers think the cell, named ‘ON delayed,’ for its slow reaction to light stimulation, manages eye growth and development in children. According to the study, which used a mouse retina for testing, when the cell dysfunctions, it instructs the eye to grow for too long, causing the retina to fail when focusing on images. This, in turn, results in myopia.The study attributes the cell’s dysfunction to overstimulation caused by the high red/green contrast of indoor lighting, which leads to eye overgrowth. By this logic, too much time spent indoors during childhood could be the trigger for the cell’s dysfunction.
While the discovery could eventually prove to be a new key to myopic management, some in the field caution against jumping to conclusions. “The media has been calling this retinal ganglion cell a ‘myopia cell,’ but we need to be cautious for best patient care,” says Monica Jong, PhD, BOptom, senior research fellow at the Brien Holden Vision Institute. “This cell is thought to detect defocus, and is found in the mouse retina, but has not yet been identified in primates or humans.”
Defocus has been a target of myopia control efforts, including successes with soft multifocal contact lenses, orthokeratology and executive bifocals. In that regard, Dr. Jong believes the study has opened up new possibilities. “Its potential role in detecting defocus is helpful to further our understanding of one of the mechanisms of myopia,” she says.
The researchers hope to eventually find a gene connected to this cell, at which point scientists can alter its activity in a mouse test subject to try to initiate and cure myopia. A human connection for the cell is also prime among areas to address. “Future research on this needs to identify whether the ON delayed retinal ganglion cell directly influences eye growth and whether it is in humans,” says Dr. Jong.
In the meantime, encouraging more outdoors time in children can be helpful in controlling myopia, even though the connection is still being formed. “We know that time outdoors can prevent new cases of myopia, but the mechanism by which it works is still unclear. This area of research is growing, and evidence is continually building to inform patient care.”
| 1. Mani A, Schwartz GW. Circuit mechanisms of a retinal ganglion cell with stimulus-dependent response latency and activation beyond its dendrites. Available at www.cell.com/current-biology/abstract/S0960-9822(16)31513-5. Accessed on February 14, 2017. |
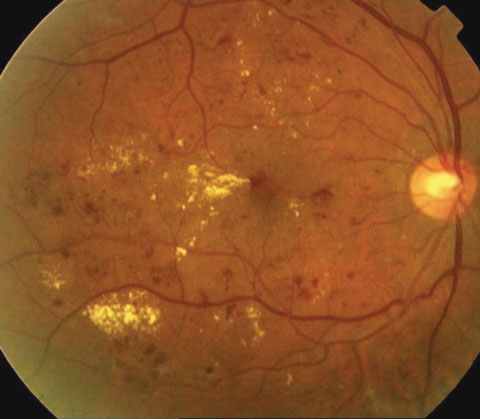
Screening for DME: Look for the Red
New research, recently published in Optometry and Vision Science, suggests focusing on the red channel in color fundus photographs could help reveal diabetes-related eye conditions, especially in racial/ethnic minorities. Investigators at the Indiana University School of Optometry, Bloomington, looked at color fundus photographs of 2,047 adult patients with diabetes, 148 of whom presented with clinically significant diabetic macular edema and 90% of whom identified themselves as a racial or ethnic minority. Standard, full-color fundus imaging showed 13 patients had cystoid macular edema (CME).
When comparing the standard, full-color fundus images with images divided into the red (long wavelength) and green (shorter wavelength) color channels, the researchers found CME was easier to detect using the red-channel images, which showed 100% agreement with the standard, full-color photographs.
However, the same was not true for the green-channel images, in which five of 13 cases of CME were not visible. All five cases were in patients with dark fundi, the researchers note. The cysts in the red-channel images appeared more numerous and covered roughly twice as much area compared with the green-channel images.
The researchers concluded that separating the red-channel color in retinal images could offer an advantage when screening under-served groups who have a high proportion of dark-eyed patients and higher rates of diabetic eye disease.
| Alhamami MA, Elsner AE, Malinovsky VE, et al. Comparison of cysts in red and green images for diabetic macular edema. Optom Vis Sci. 2017;94(2):137. |
Drug Combo Shows Promise for DR Treatment
A recent study may have uncovered a promising treatment option for patients with diabetic retinopathy (DR). In a rat model, researchers found that a two-drug combination better protected against diabetes-related vision loss compared with a single drug.1The combination of an angiotensin receptor neprilysin inhibitor (ANRI) that contains irbesartin (an angiotensin receptor blocker) and thiorphan (a neprilysin inhibitor and anti-diarrhea compound) was more effective at reducing the symptoms of DR in rat retinas compared with the use of irbesartin alone. Capillary loss was reduced by 68% in the group given ARNI, compared with 43% in the single-drug group. The ARNI group also showed reduced apoptotic cell death by 51%, while the single-drug group showed a reduction of 25%. In addition, the reduction percentages between the ARNI group and the single-drug group were roughly the same after five weeks. Because DR is strongly associated with prolonged diabetes, ARNI’s efficacy over time is a promising sign.
 |
| ANRI may one day help patients avoid the effects of diabetic retinopathy for longer. |
As promising as these findings may be, research still needs to address several areas, including long-term effects, side effects and, eventually, tests on the human eye. Still, these results are a step in the right direction for DR patients. “It may someday help millions of diabetic patients affected by retinopathy and its devastating visual complications,” says Dr. Ferrucci. “If we could slow down the progression and help patients with diabetes live longer without visual complications, we can really increase these patients’ quality of life.”
| 1. Prasad T, Roksnoer LCW, Zhu P, et al. Beneficial effects of combined AT1 receptor/neprilysin inhibition (ARNI) versus AT1 receptor blockade alone in the diabetic eye. Invest Ophthalmol Vis Sci. 2016;57(15):6722–30. |
In the news
New research suggests cells developed using induced pluripotent stem cells (iPSCs) do not contain more mutations than cell lines created using other methods such as subcloning—a concern that has slowed medical research. Using skin cells from the same donor, investigators created identical copies of the cells using iPSCs and subcloning. When they sequenced the DNA, they found mutations occurred at the same rate in both iPSC and subcloned cells. | Kwon EM, Connelly JP, Hansen NF, et al. iPSCs and fibroblast subclones from the same fibroblast population contain comparable levels of sequence variations. PNAS. 2017;114(8):1964-9. |
Laundry detergent pods, with their colorful packaging and easy rupture, are proving hazardous, according to a new study. Researchers found that, between 2012 and 2015, ocular chemical burns associated with laundry pods increased from one dozen to 480 and accounted for 26% of all chemical ocular burn injuries in 2015 among three- and four-year-olds—up from just 0.8% in 2012.
| Large increase in eye injuries linked to laundry detergent pods among young children. ScienceDaily. February 21, 2017. Available at www.sciencedaily.com/releases/2017/02/170202122817.htm. Accessed February 21, 2017. |
A new RNA interference (RNAi) therapeutic agent may safely block ocular inflammation, according to new research. Used a mouse model, investigators tested a single-strand RNAi agent that suppresses the receptor-associated prorenin system involved in the pathogenesis of uveitis. Results suggest this new molecule was safe and effective, causing significant improvement of both acute uveitis and chronic diabetic inflammation.
| Kanda A, Ishizuka ET, Shibata A, et al. A novel single-strand RNAi therapeutic agent targeting (pro)renin receptor suppresses ocular inflammation. Molecular Therapy - Nucleic Acids. January 12, 2017. [Epub ahead of print]. |
Correction |
| In the article, “Are You Missing these Optic Neuropathies?” (February 2017), the formula for calculating erythrocyte sedimentation rate (ESR) was incorrect. The corrected text reads: “For ESR, the expected range is equal to the age of a male patient divided by two and the age of a female patient +10 divided by two.” |

