 |
An 81-year-old Caucasian male was referred for a YAG capsulotomy evaluation. He complained of constant blurry vision, which started two years ago and was more prevalent in the right eye. Because of this, he had difficulty distinguishing road signs, seeing his cell phone and watching TV. He reported that his vision was “like looking through wax paper” and it had been very difficult to function because he is hard of hearing and depends heavily on his vision.
His medical history consisted of thyroid disease, heart murmurs, hypertension and COPD. His ocular history included cataract surgery OU and a horseshoe tear (HST) with vitreous hemorrhage OD that was treated with argon laser approximately two years ago. He developed an inferior retinal detachment (RD) three months after the HST repair and was treated with pars plan vitrectomy and silicone oil. Postoperative instructions included maintaining face-down positioning; however, the patient was unable to position his head correctly. He subsequently developed proliferative vitreoretinopathy (PVR) with inferior fluid and required a retinectomy.
Upon exam, his best-corrected vision was 20/200 OD and 20/80 OS. The motility was full in both eyes, and confrontation visual fields were restricted 360 OD and full to careful finger counting OS. Pupil was round but nonreactive to light in OD; the one OS was reactive to light. There was an afferent pupillary defect in the OD by reverse testing.
Slit lamp exam of the anterior segment examination showed a central corneal scar OD and mild punctate epithelial erosion. Significant neovascularization of iris (NVI) OD was seen (Figures 1 and 2). Also noted was PCIOL, s/p YAG capsulotomy in OD. A PCIOL was present in OS with moderate posterior capsular opacification OS. IOPs was 28mm Hg OD and 10mm Hg OS. No apparent neovascularization of the angle (NVA) or peripheral anterior synechia was visible during gonioscopy.
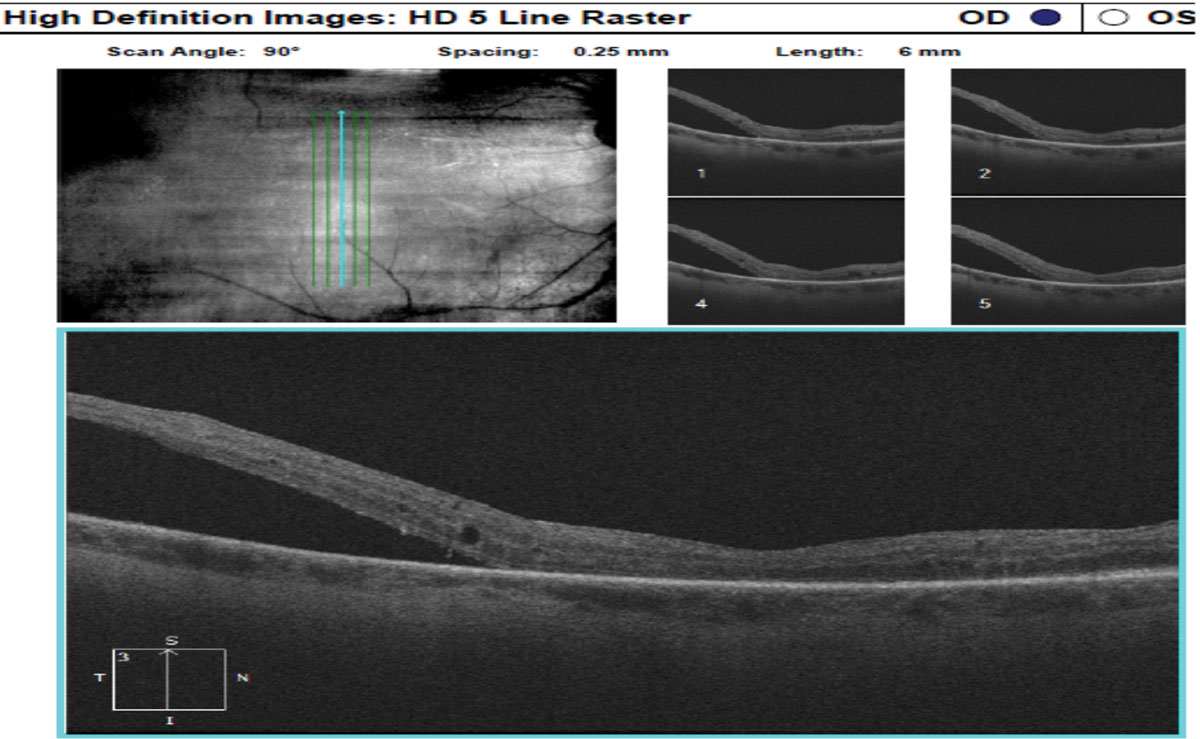
Evaluation of the posterior segment showed CD ratio larger in OD compared to OS. Right eye nerve appeared shallow, and macula showed subretinal fluid (SRF). The area of retinectomy was visible. It also showed chronic anterior inferior retinal detachment (Figure 3). OCT of the right eye confirmed SRF (Figure 4). Left nerve had cup to disc ratio of 0.40, and the rest of the posterior segment was unremarkable.
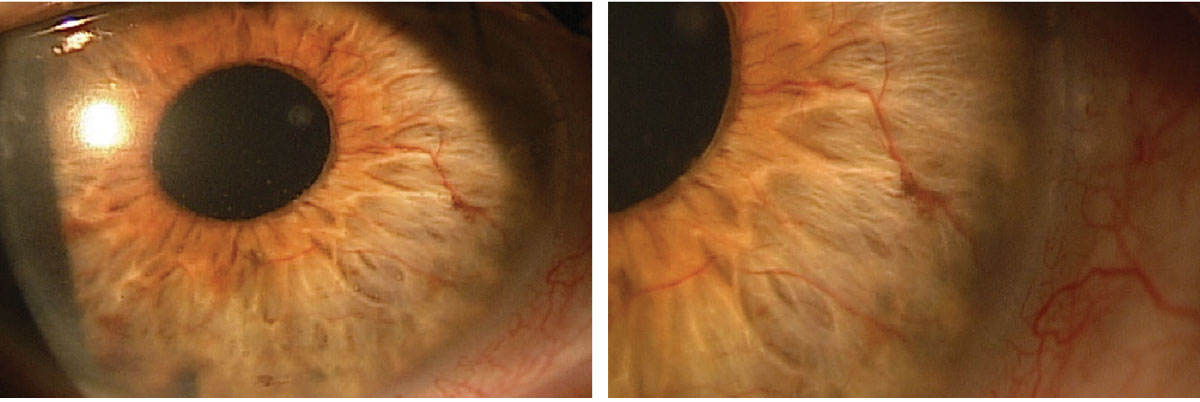 |
Figs. 1 and 2. Neovascularization of iris (NVI) was found during the slit lamp exam. Click image to enlarge. |
Take the Retina Quiz
1. Which is not a cause of NVI?
a. Central retinal vein occlusion (CRVO).
b. Chronic RD.
c. Proliferative diabetic retinopathy (DR).
d. Exudative macular degeneration.
2. What duration of time defines an RD as “chronic?”
a. Greater than one week.
b. Greater than two weeks.
c. Greater than one month.
d. Three months.
3. Which is not considered a risk factor for development of PVR in a RD?
a. Vitreous hemorrhage.
b. Chronic RD.
c. Smoking history.
d. DR.
4. What is the surgical failure rate in RD repair due to PVR?
a. 1% to 5%.
b. 5 to 10%.
c. 10% to 20%.
d. Over 25%.
5. Which statement is false?
a. NVI can occur before NVA.
b. NVA can occur before NVI.
c. Prostaglandin analogs should be used to manage neovascular glaucoma (NVG).
d. Prostaglandin analogs should not be used to manage NVG
For answers, see below.
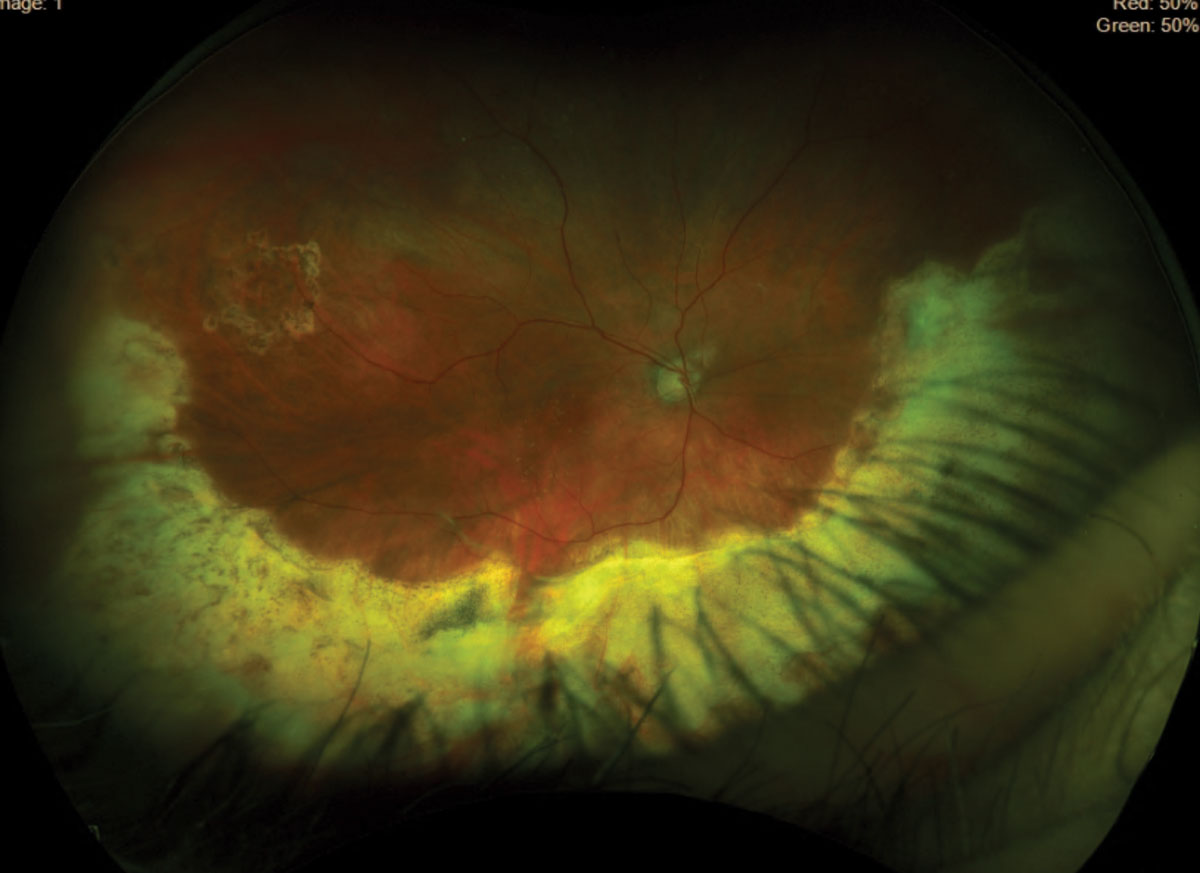 |
| Fig. 3. Inferior retinal detachment was found in the right eye. Click image to enlarge. |
Diagnosis
This patient was diagnosed with an old rhegmatogenous retinal detachment (RRD), macular atrophy from presumed multiple macula-off RDs, active NVI and ischemic status of the retina (suspected ocular ischemic syndrome) OD, and ocular hypertension from impending NVG. He also had some detached retina inferiorly, which was believed to represent the anterior portion of the retinectomy.
The previous carotid Doppler—done 10 years prior—was found to have 80% occlusion, which prompted a new Doppler to be ordered. After reviewing the results, the retina specialist did not think repair of the patient’s chronic RD would abate the anterior segment neovascularization. He was started on Combigan (brimonidine/timolol, Allergan) BID OD to help lower the intraocular pressure (IOP).
Discussion
Historically, the most common causes of NVI include DR and CRVO. His retina did not show any signs of these conditions and he denied having diabetes or any history of venous occlusion. Other differential diagnoses included retinal ischemia, tumors, ocular inflammation and RD.
This patient had a history of RRD, PVR and retinectomy. PVR is thought to be an abnormal wound healing process where proliferative, contractile cellular membranes form in the vitreous and the retina, causing tractional RD. Membranes are formed due to cytokines and inflammatory mediators from tissue damage or anatomic disruption caused by the RRD.1
The surgical failure rate of RRD repair due to PVR in RRD is believed to be between 5% and 10%. Risk factors for PVR development include retinal tear size, presence of vitreous hemorrhage, chronic intraocular inflammation, longstanding untreated RRD, unsuccessful RRD repair, history of smoking and penetrating ocular trauma.2
 |
|
Fig. 4. OCT of the right eye confirmed SRF. Click image to enlarge. |
Retinectomy is the treatment of choice to relax the tension on the retina by peeling the tractional membrane and removing the tissue—the anterior flap of a retinal tear or remove the fibrotic, contracted retina from PVR.2,3 It is performed in up to 64% of the PVR cases. Studies have shown that retinectomy with use of silicone in eyes with recurrent RD or PVR shows good prognosis and low risk of recurrence. Three types of retinectomy are performed: inferior 180° (as seen in this patient), 360° and focal posterior—of which the first is most common.3
The severe neovascularization of the patient’s anterior segment was thought to be secondary to carotid occlusive disease or from hypoxia due to chronically detached retina. Carotid artery occlusion with elevated IOP in the ipsilateral eye is suspicious for ocular ischemic syndrome.4 However, his current carotid Doppler was reported to be normal.
Retinal ischemia and subsequent hypoxia can occur due to chronic separation of the sensory retina from the choroidal blood flow.1 This can trigger neovascularization. In this patient, chronic RD caused retinal ischemia and hypoxia, which stimulated the production of VEGF and triggered the NVI.
Preserving the remaining vision, preventing NVG and secondary angle closure glaucoma OD and improving his vision OS by performing YAG capsulotomy are the primary goals for this patient.
NVG can be managed with topical alpha-2 agonists, beta blockers and topical or oral carbonic anhydrase inhibitors. Prostaglandin analogs should be avoided to prevent further breakdown of the blood-aqueous barrier.4 The patient’s IOP remained high on Combigan BID, so he was referred to a glaucoma surgeon for possible surgical intervention.
Special thanks to Taylor Brooke Runyon and Hannah Collier, both fourth-year students at University of Pikeville, Kentucky College of Optometry.
Retina Quiz Answers
1) d; 2) b; 3) d; 4) c; 5: c
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
Dr. Patel received her doctor of optometry degree at Nova Southeastern University College of Optometry and practices at Commonwealth Eye Surgery in Lexington, KY. She is a member of the Kentucky Optomeric Association and the American Optometric Association. She has no financial interests to disclose.
| 1. Abrams GW. Proliferative vitreoretinopathy. American Academy of Ophthalmology. March 8, 2021. eyewiki.aao.org/Proliferative_Vitreoretinopathy. Accessed July 25, 2021. 2. Aboumourad R. Persistent proliferation. RevOptom. 2021;198(5):94-6. 3. Eliott D. Retinectomy: contribution to vitreoretinal surgery. Ophthalmology Times. March 13, 2013. ophthalmologytimes.com/view/retinectomy-contribution-vitreoretinal-surgery. Accessed July 25, 2021. 4. Rodrigues GB, Abe RY, Zangalli C. Neovascular glaucoma: a review. Int J Retin Vit. November 14, 2016. journalretinavitreous.biomedcentral.com/articles/10.1186/s40942-016-0051-x. Accessed July 25, 2021. |

