 |
A 16-year-old Caucasian male presented for routine comprehensive eye exam and contact lens evaluation. He reported no vision problems and just wanted to update his contact lens prescription.
His best-corrected visual acuities were 20/25 OD, 20/20 OS. Confrontation fields were full-to-finger count, extraocular muscles exhibited full range of motion and pupils were equal, round and reactive to light without afferent pupillary defect.
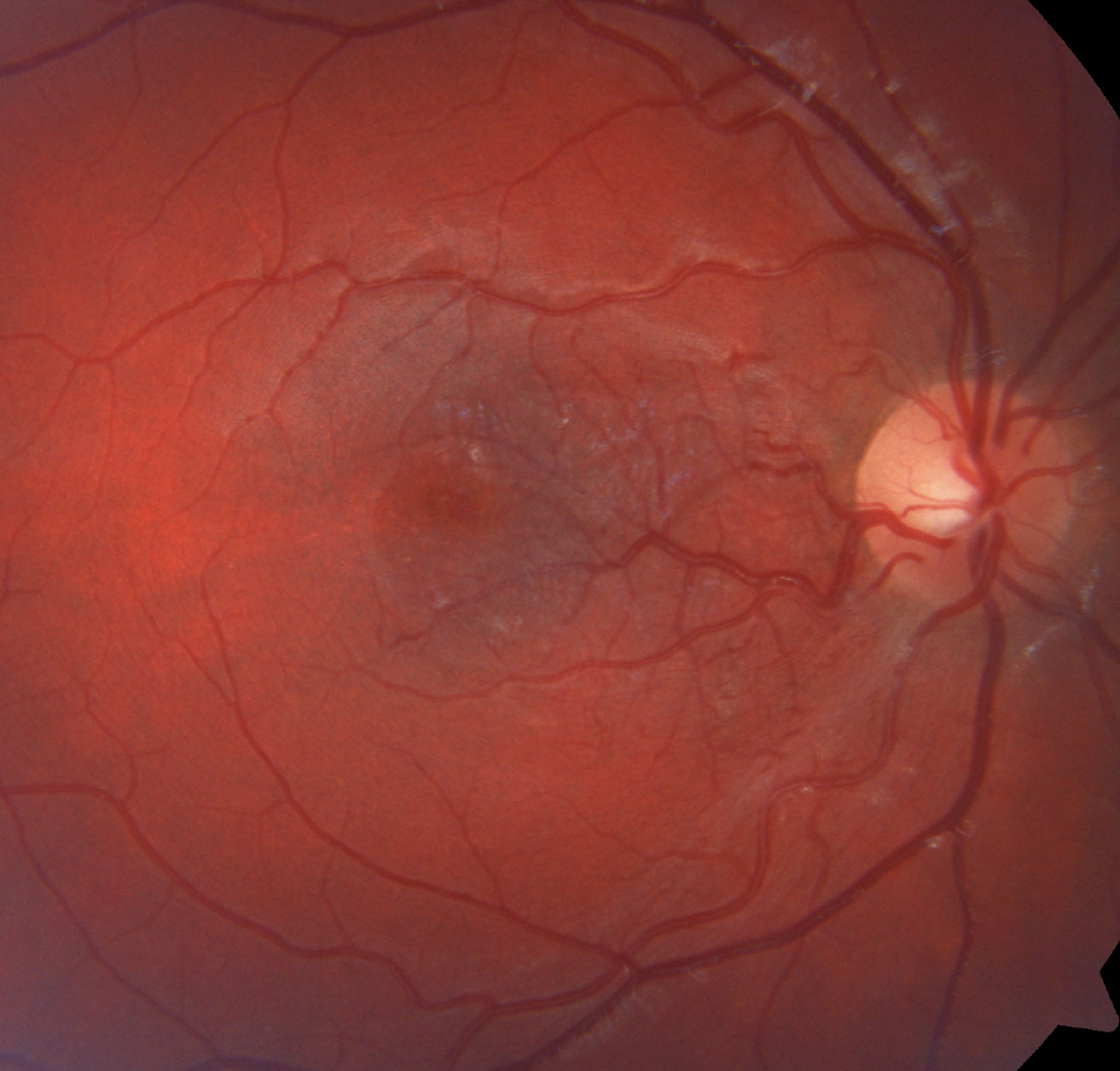
Slit lamp examination was unremarkable. Intraocular pressures were 19mm Hg OD and 17mm Hg OS via iCare tonometer (iCare). A dilated fundus exam revealed retinal vascular changes (Figure 1). The red-free image of the right eye is also available (Figure 1b). Optical coherence tomography (OCT) of the right eye’s macula was performed (Figure 2).
 |
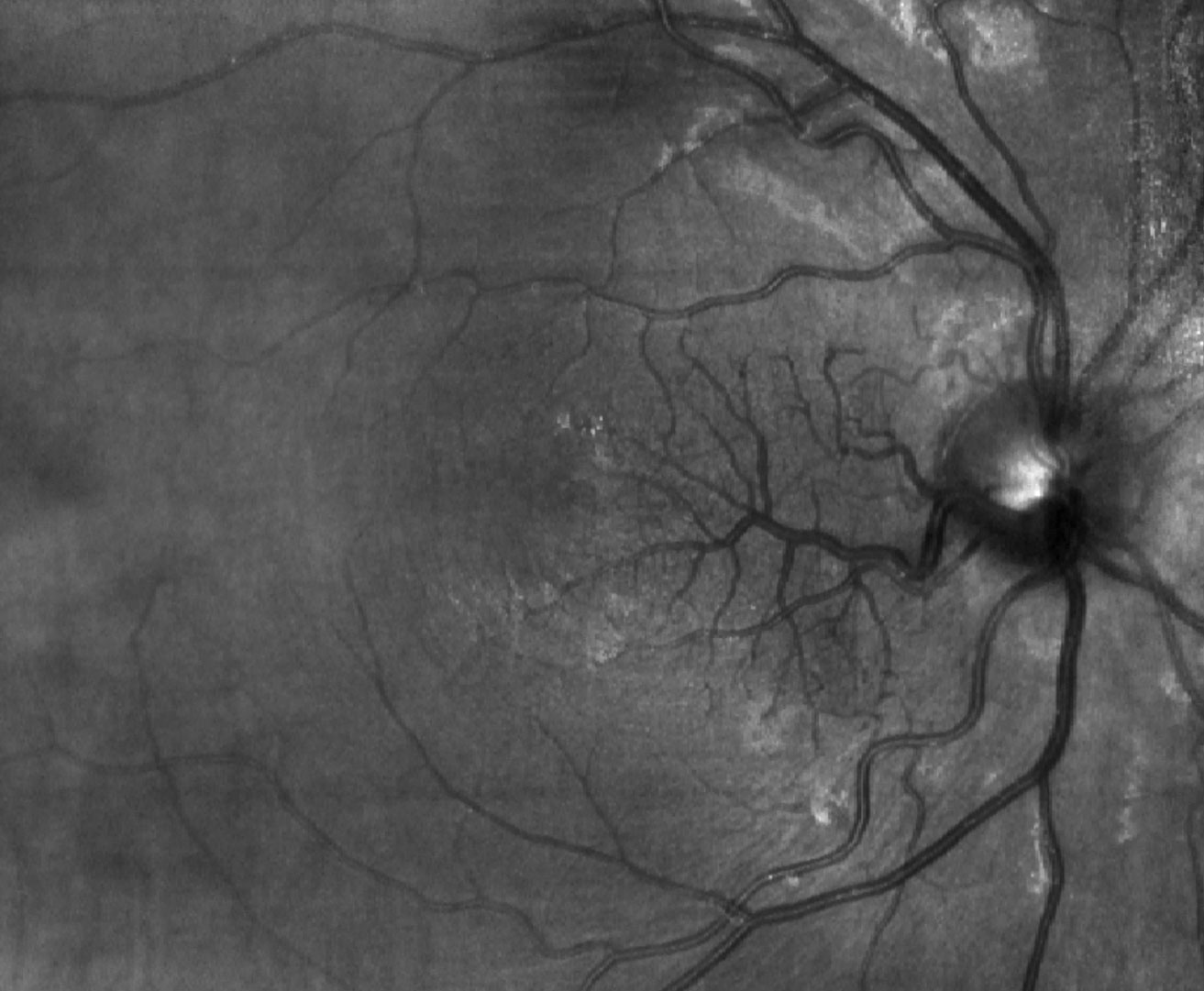 |
| Fig. 1a. and 1b. This fundus (above) and the red-free image of our 16-year-old patient’s right eye shows an unusual retinal finding. Can you identify the patient’s condition? Click images to enlarge. |
Take the Quiz
1. How would you best describe the vascular findings in Figure 1?
a. Retinal neovascularization.
b. Shunt vessels (collaterals).
c. Dilated and aberrant macular vessel crossing horizontal raphe.
d. Retinal hemangioma.
2. How would you characterize the findings at the junction of inner and outer retina in the OCT of the right eye in Figure 2?
a. Hard exudates.
b. Large vessels in deep capillary plexus.
c. Foveal cyst.
d. Both b and c.
3. What is the correct diagnosis?
a. Retinal venous malformation (congenital retinal macrovessel).
b. Retinal capillary hemangioma.
c. Branch retinal vein occlusion.
d. Neovascularization.
4. What other testing would you order?
a. Genetic testing.
b. Blood pressure.
c. Carotid imaging.
d. Neuroimaging.
5. What other clinical condition/finding is associated with this retinal finding?
a. Vascular malformation of the brain.
b. Von Hippel-Lindau syndrome.
c. Strawberry hemangioma.
d. Port wine stain.
Diagnosis
This patient presented with a large aberrant vessel in his right eye, which we determined was a retinal venous malformation (RVM), also known as congenital retinal macrovessel. RVM is a dilated, aberrant vein that traverses the foveal region and crosses the horizontal raphe.1,2 It can originate either as a branch of one of the arcades, from the central retinal vein or from its immediate branches at the disc. It presents unilaterally and is usually found incidentally, due to minimal or no effect on visual acuity.1,2
RVM is rare, with an estimated incidence of 1:200,000, though that may be an underestimation since patients are typically asymptomatic.2 RVM is non-progressive, and visual/ocular prognosis is excellent. However, recent studies show a correlation between RVM and vascular malformations of the brain, which can have significant complications.2,3 Our patient was promptly sent for brain MRI.
Visual acuity may be affected in cases where:
- Tributaries of the abnormal vessel cross over the foveola.
- There is a presence of a foveolar cyst.
- There are changes to foveal avascular zone.1-4
Some cases report retinal hemorrhage or central serous retinopathy associated with RVM, but these may be coincidental or due to other underlying etiologies.2-4 Though acuity may not be affected in most patients, one study determined that retinal sensitivity can be reduced in the area of the aberrant vessels despite normal Snellen acuity.5
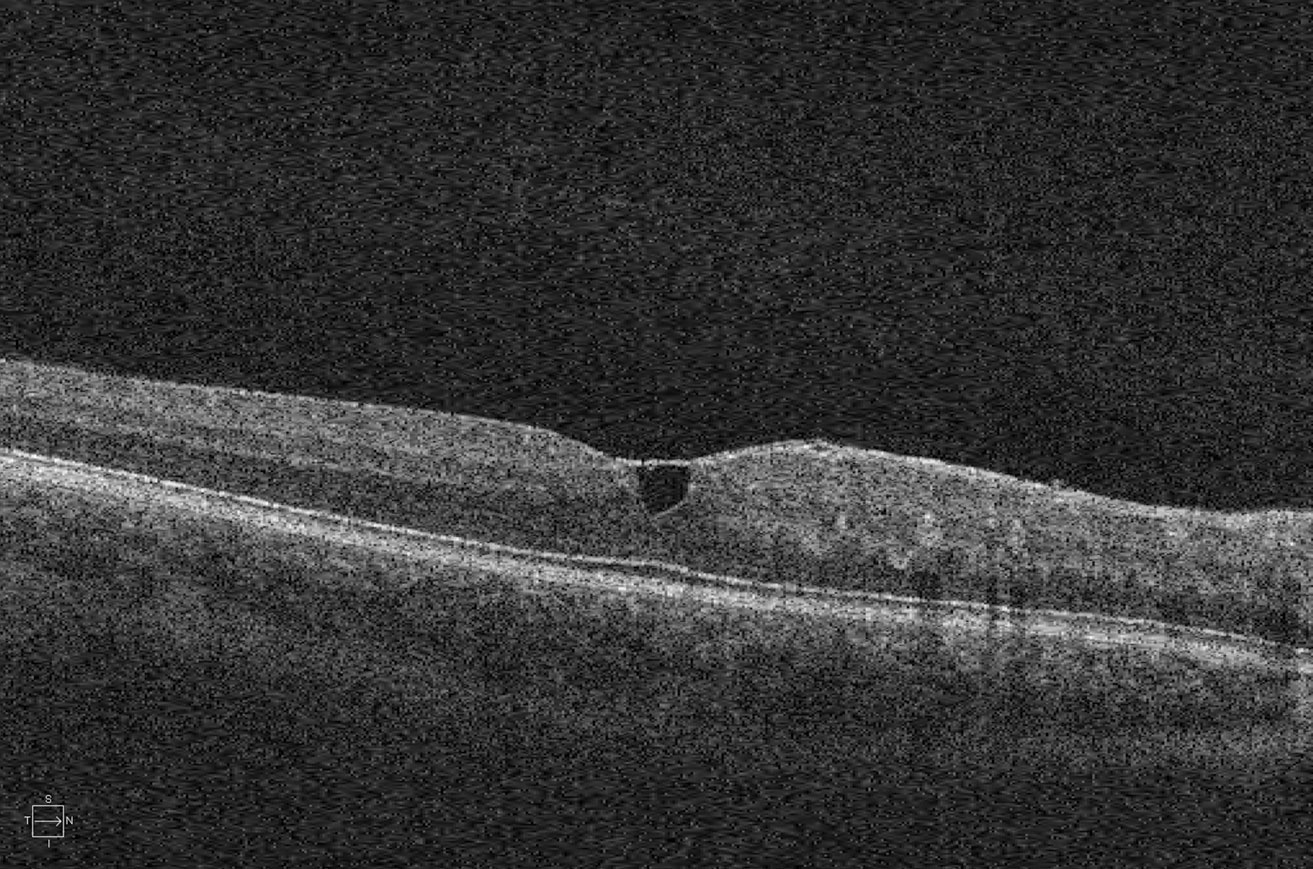 |
| Fig. 2. We also obtained this SD-OCT image of the macula of the patient’s right eye. Click image to enlarge. |
Discussion
In our case, the slightly reduced acuity is possibly due to the epiretinal membrane-like structural changes, foveal cyst and abnormal vessels within the foveola. Though neither fluorescein angiography nor OCT angiography has been done on this patient, large vessels are visible in the deep capillary plexus on OCT within the fovea, and it is plausible that small tributaries of these vessels course through the foveola.
Fluorescein angiography of RVM reveals early filling and late emptying. Sometimes there are areas of capillary non-perfusion adjacent to the aberrant vessel or remodeling of the foveal avascular zone. Microaneurysm-like changes can also be seen. However, in none of these cases is there leakage from the RVM.1-4 Because there is no leakage, it is proposed that foveal cysts form secondary to perfusion abnormalities and that the microaneurysm-like changes are just large vessels viewed en face.1
A proposed etiology is that RVM originates in the 15th or 16th week of gestation when pre-endothelial mesenchymal cells invade nerve fiber layer from the hyaloid artery at the optic disc. These cells eventually differentiate and mature into blood vessels and, researchers believe, during the maturation process one of these vessels enlarges and positions inappropriately.1,6 The stimulus for this event is unknown.1,6
Most importantly, a significant correlation exists between RVM and vascular malformations of the brain. One retrospective study looked at 49 patients across the globe determined to have RVM. In the 12 who were found to have either a venous or cavernous malformation of the brain, the abnormality was ipsilateral in 85% and in the frontal lobe in 75%.2
This study suggests a rate of 24% of vascular malformation of the brain in the presence of an RVM, but this may be an underestimation since only 27 patients had neuroimaging done and 44% of those MRIs had vascular abnormalities.2 Compared with a rate of 0.2% to 6.0% of brain venous malformations in the general public, this study clearly demonstrates a strong correlation between RVM and venous malformation of the brain.2 Based on these neurologic findings and retinal vessel appearance, researchers believe RVM may be a milder variant of racemose angiomatosis (Wyburn-Mason syndrome).4,6
Recent publications encourage using the term retinal venous malformation rather than congenital retinal macrovessel to highlight the correlation between RVM and venous malformation of the brain and to emphasize the importance of ordering neuroimaging.2,4
At this time, our patient has yet to undergo neuroimaging and is currently scheduled for a CT angiography and brain MRI.
Dr. Schaeffer graduated from the Illinois College of Optometry in 2017, and completed his residency training in ocular disease at Bascom Palmer Eye Institute. He is currently providing primary eye care with MyEyeDr in Birmingham, AL.
1. Brown GC, Donoso LA, Magargal LE, et al. Congenital retinal macrovessels. Arch Ophthalmol. 1982;100(9):1430-6. 2. Pichi F, Freund K, Ciardella A, et al. Congential retinal macrovessel and the association of retinal venous malformations with venous malformations of the brain. JAMA Ophthalmol. 2018;136(4):372-9. 3. Sanfilippo C, Sarraf D. Congenital macrovessel associated with cystoid macular edema and an ipsilateral intracranial venous malformation. Retin Cases Brief Rep. 2015;9(4):357-9. 4. de Crecchio G, Alfieri MC, Cennamo G, Forte R. Congenital macular macrovessels. Arch Clin Exp Ophthalmol. 2006;244(9):1183-7. 5. Shah VA, Chalam KV. Congenital retinal macrovessel causes reduced retinal sensitivity at the macula. Eur J Ophthalmol. 2004;14(4):341-4. 6. Archer D, Deutman A, Ernest J, Krill A. Arteriovenous communications of the retina. Am J Ophthalmol. 1973;75(2):224-41. |
Retina Quiz Answers:
1) c; 2) d; 3) a; 4) d; 5) a

