 |
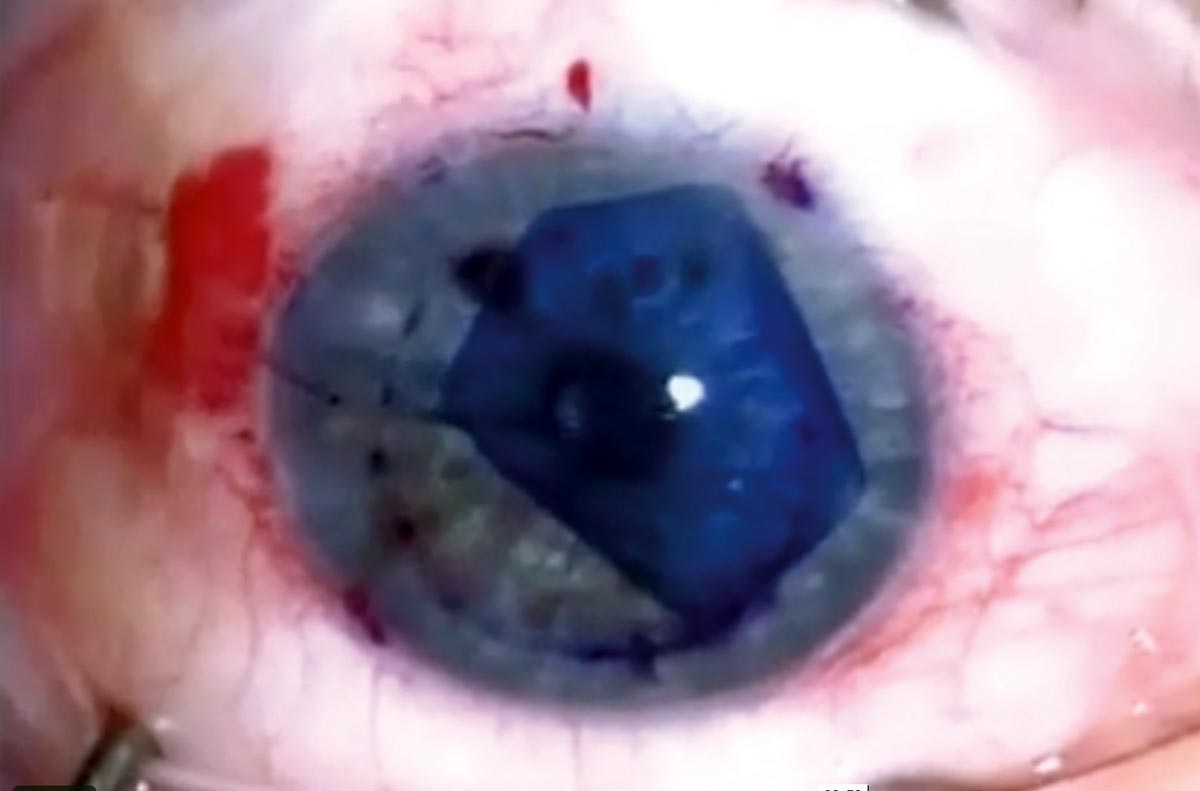
| Several factors were identified in this study that contributed to the 30% of people who experienced no visual improvement one year post-EK. Photo: Jim Guzek, MD. Click image to enlarge. |
Endothelial keratoplasty (EK) is an increasingly common procedure owing to its high graft survival rate and short recovery period. Still, visual outcomes vary among patients due in part to unknown reasons, which is why researchers recently conducted a study to identify the possible risk factors for lack of vision improvement post-surgery. The data concluded that worse visual acuity (VA) outcomes were associated with two main independent factors: postoperative re-bubbling procedures and repeat keratoplasties.
The large database analysis included 30,600 patients in the IRIS registry who underwent EK procedures between 2013 and 2018. The primary outcome measure of the study was change in VA relative to baseline, which was assessed at six months and again at one year. Multivariable models were used to adjust for potential associated factors including sociodemographic factors, baseline vision, surgical indication, ocular comorbidities and postoperative complications. The study population was split between four groups based on their diagnoses: (1) Fuchs’ endothelial corneal dystrophy (FECD), (2) bullous keratopathy (BK), (3) prior graft failure and (4) other or not reported.
On average, VA improved from 0.54logMAR at baseline to 0.40logMAR at six months and further improved to 0.30logMAR by one-year post-op. The following percentage of patients in each subgroup did not achieve significant visual improvement one year after EK: 30.3% of the total cohort, 29.8% of the FECD subgroup and 27.4% of the BK subgroup.
Risk factors for lack of VA improvement differed slightly between subgroups, as two distinct sociodemographic disparities were noted among FECD patients. “In the FECD subgroup, older age (risk ratio: 1.05 per five-year increase) and female sex (risk ratio: 1.10) were associated with VA worse than or equal to baseline at one-year post-op,” the researchers wrote. On the other hand, in the BK subgroup, prior or concurrent routine cataract surgery increased the likelihood of VA improvement.
“In both FECD and BK subgroups, eyes with higher baseline logMAR VA were more likely to have visual improvement postoperatively (FECD risk ratio: 0.82, BK risk ratio: 0.91), whereas postoperative re-bubble procedures (FECD risk ratio: 1.10, BK risk ratio: 1.31) and repeat keratoplasties (FECD risk ratio: 1.41, BK risk ratio: 1.42) were associated with a higher risk of no improvement in VA,” the researchers continued.
They noted the significance of the finding that nearly a third of patients did not experience visual improvement one year after EK. While more studies are needed to investigate why this is the case, the current analysis made several observations about which patients were less likely to receive desirable VA outcomes. “Increased age was associated with higher odds of vision not improving or being worse than baseline, which may explain why patients with advanced age are less likely to undergo a repeat EK,” the researchers wrote.
Female gender could also have been associated with a lack of VA improvement since “FECD is a polygenic disease that has been shown to be more prevalent and severe among women.” In addition, the investigators pointed out another possibility: “Female patients undergoing EK could have more advanced disease, chronic edema or subepithelial corneal scarring that may limit recovery after surgery.”
In conclusion, the researchers recommended remaining cognizant of the link between the following factors and worse VA improvement one-year post-EK: postoperative re-bubble procedures, infectious keratitis, prior or concurrent retinal procedures, subsequent keratoplasty, other anterior segment procedures and preexisting glaucoma.
Srikumaran D, Son H-S, Li C, et al. Disparities in visual acuity outcomes after endothelial keratoplasty – an IRIS registry analysis. Ophthalmology. April 1, 2022. [Epub ahead of print]. |

