 |
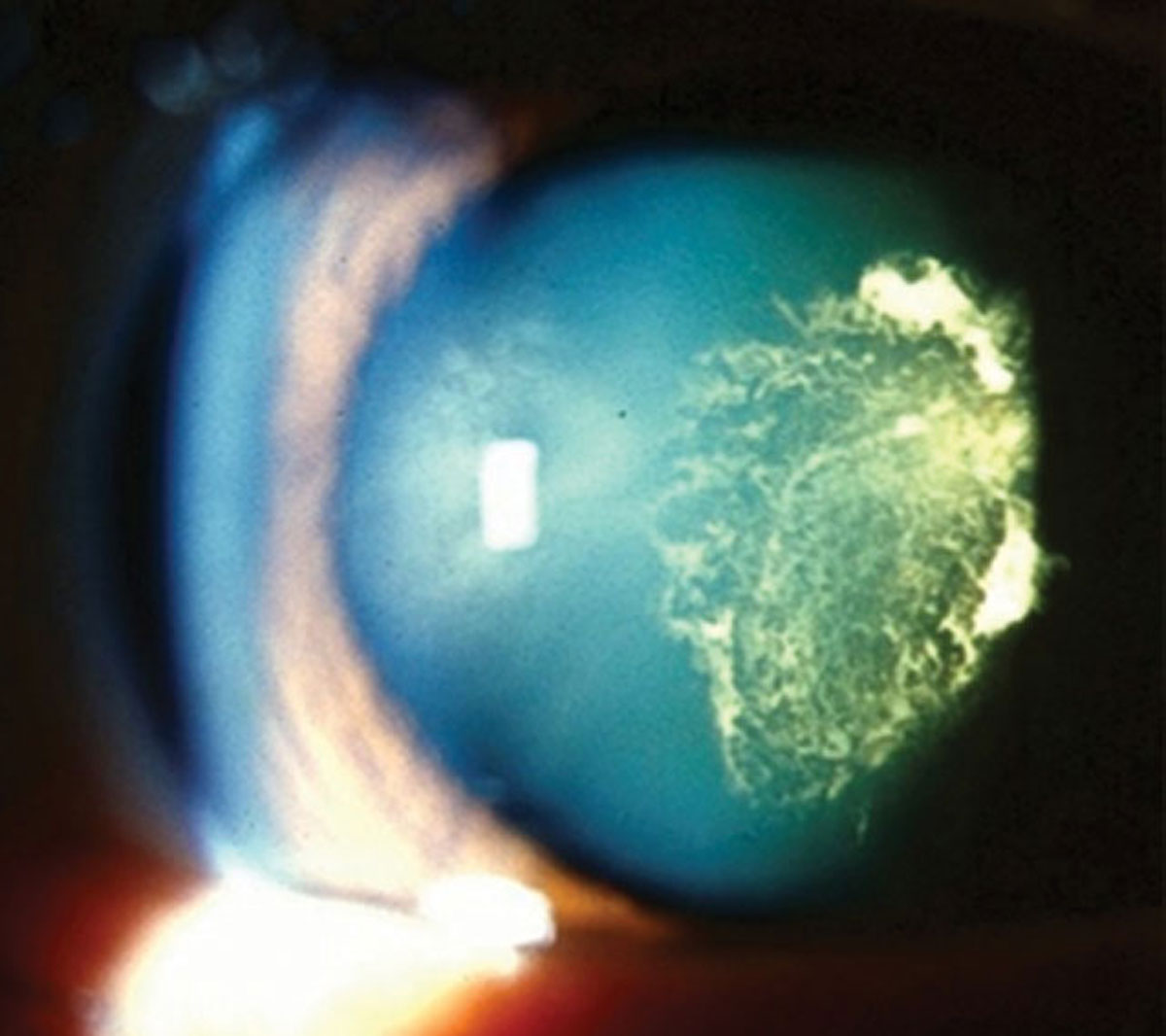
| Patient-practitioner collaboration contributes to more successful cataract outcomes. Photo: Julie Tyler, OD. Click image to enlarge. |
Shared decision making—a relatively new approach in which clinicians and patients work together to determine the best treatment option based on clinical evidence while balancing risks and expected results—has been associated with improved patient knowledge, satisfaction and outcomes in both medical and surgical specialties. New research from the Albert Einstein College of Medicine in the Bronx suggests shared decision making may also be effective in eye care, particularly in cases where patients have glaucoma or cataracts.
The investigators analyzed 19 shared decision making-based studies pertaining to chronic medical and surgical conditions in eyecare, all of which emphasized the value of this approach, with two reporting improved patient outcomes.
One pilot study of 65 patients with POAG queried patients before and after they received an educational booklet about their condition. After reading the booklet, patients reported improvements in their satisfaction, glaucoma knowledge, medication adherence and decision making.
The second study, a randomized control trial of 773 patients, examined the effectiveness of a patient decision aid for cataract surgery. The investigation found the intervention group that received the decision aid had fewer issues when it came to decision making and was less likely to regret their treatment choice compared with individuals in the control group.
Shared decision making is especially useful in chronic conditions that have multiple evidence-based management options and require patient adherence and participation, such as in the treatment of glaucoma and age-related cataracts, the authors noted.
However, in more acute care conditions such as uveal melanoma, one study concluded that the conventional principles of shared decision making didn’t apply. In this time-sensitive setting with few viable treatment options, traditional paternalistic medicine plays a greater role, the investigators explained.
While many of the doctors and patients in the reviewed studies cited positive opinions about shared decision making, barriers to implementation still exist, including time, resources and experience, the researchers said.
Regardless, the authors found no papers that investigated or demonstrated poorer patient outcomes following shared decision making.
Bouaziz M, Cheng T, Minuti A, et al. Shared decision making in ophthalmology: a scoping review. Am J Ophthalmol. December 4, 2021. [Epub ahead of print]. |

