Dry eye and allergy are common presentations in optometric practice, and they can wreak havoc on a patient’s ocular comfort, especially for contact lens wearers. But with prompt diagnosis and management, astute clinicians can keep patients comfortable in their contact lenses, even in the face of allergy, dry eye or both.
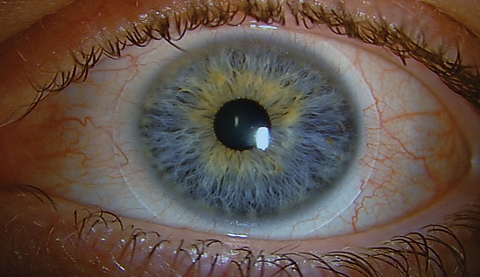 |
| A hypersensitivity or toxic reaction to the preservative in the contact lens solution is typically characterized by conjunctival injection and superficial punctate keratitis. Click image to enlarge. |
Know the Enemy
The first step to diagnosis is knowing what to look for. While allergy and dry eye often present with similar symptoms, their differing pathophysiology and prevalence among certain patient populations can help with the differential diagnosis.
Allergy. Recent reports suggest the prevalence of allergic conjunctivitis (AC) may be as high as 40%.1 As with asthma, the increase in AC prevalence has been observed globally in adults as well as children.2 Although seasonal AC is the most common presentation, chronic forms such as vernal and atopic keratoconjunctivitis contribute to the overall disease spectrum as well. While vernal keratoconjunctivitis has a predilection for males younger than 18 years, seasonal and perennial AC is often present in all genders from childhood through middle age.3,4 Although symptoms associated with atopy tend to decrease with age—in opposition to dry eye—AC may persist well beyond middle age.1
Itching is generally perceived as the harbinger of allergies.5 Milder presentations may exhibit relatively modest clinical signs. With more severe disease, a clinically consistent picture would include chemosis, conjunctival injection, eyelid edema or a combination of all three.3 First-line treatment typically includes antihistamines (often in association with a mast cell inhibitor).6 Over-the-counter (OTC) topical agents such as ketotifen fumarate administered twice daily are accessible to the patient at a relatively modest cost. Prescription medications potentially add convenience (once-daily dosing) and higher efficacy.7 A “softer” corticosteroid with a lower propensity for side effects (ocular hypertension, cataract) may be added to the regimen on a short-term basis, particularly when the clinical signs are more severe.6 Cold compresses and avoiding the allergen, when feasible, may be beneficial as well.6,7
 |
| Adults may benefit from preemptive management of coexisting dry eye and allergy. |
Dry eye. In 2007, the International Dry Eye Workshop (DEWS) examined available data and reported potential risk factors for dry eye disease (DED).8 DEWS retained the 1995 National Eye Institute/Industry Workshop classification of aqueous tear-deficient dry eye and evaporative dry eye.9 Notably, the researchers found DED in 5% to 30% of the population aged 50 years or older with lower rates presumably reflecting patients with more severe disease and higher rates including patients with milder forms.8 DEWS also found DED increases with age and is more prevalent in women.8 In addition to age and gender, connective tissue disease, vitamin A deficiency, LASIK surgery, antihistamine use, radiation therapy, stem cell transplantation, androgen deficiency and a diet low in omega-3 essential fatty acids are consistently associated with the condition.8 Less substantiated risk factors include other medications (tricyclic antidepressants, diuretics, beta-blockers), diabetes, systemic chemotherapy and penetrating keratoplasty. The association of DED with oral contraceptives, pregnancy and menopause, while cited, is less clear.8
If itching is the harbinger of ocular allergies, burning is the hallmark of dry eye. Current practices emphasize management of evaporative, rather than aqueous tear-deficient, dry eye. Treatment strategies focus on the lipid layer of the tear film, which in turn protects the cornea from the hyperosmolarity associated with ocular inflammation. Initial intervention typically includes heat to enhance meibomian gland function, lipid-based artificial tears, nutritional counseling (omega-3 essential fatty acids) and lid hygiene.
Further management may include a short course of corticosteroids to more aggressively manage the inflammation and, as appropriate, jump start other ophthalmic agents such as cyclosporine A 0.5% and lifitegrast 5%. Oral antibiotics can provide additional anti-inflammatory effects. Heat masks (Bruder or ThermalOn) and lid hygiene products (OcuSoft and Avenova, NovaBay Pharmaceuticals) are useful in milder presentations of DED, while higher technology strategies, when accessible, may be necessary with more advanced disease. DED management is generally complementary to that of AC; however, clinicians should carefully balance the mechanical component of lid hygiene and the drying effects of oral antihistamines, as they can exacerbate symptoms of coexisting allergy/DED.
Contact lens discomfort (CLD). This remains the primary reason for discontinuation of lens wear, contributing to a dropout rate greater than 20%.10-12 As with DED, clinical signs and patient symptoms of CLD often do not correlate. Patients with dry eye frequently have CLD, and lens wearers with CLD often present without clinical signs of DED.13 In contrast to dry eye, the relationship between age and CLD remains an enigma. Some investigators suggest CLD is inversely associated with age, others report that younger wearers may have more intense dryness symptoms and some even suggest no association between CLD and age exists.14-17 Regardless, factors that promote lens comfort are integral to lifetime contact lens success.
 |
| Normally functioning meibomian glands are integral to a healthy tear film, while blockage can lead to evaporative dry eye |
Managing Coexisting Disease
Caring for patients with allergy and dry eye becomes more complicated when the two conditions coexist. DEWS defined DED as “a multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance and tear film instability with potential damage to the ocular surface. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface.”8 Inflammation is also inherent in the expression of allergy, which is defined by its hypersensitive state following exposure to an antigen.18 Other reports have also highlighted the connection between AC and dry eye.19 For example, significant symptoms of itching in conjunction with dry eye suggest coexisting atopic disease.19 Moreover, patients with AC who exhibit disruptions in tear film integrity, symptoms of burning or both may have coexisting DED.8
While acknowledging that AC and dry eye can coexist, one condition often overshadows the other when it comes to patient symptoms. The clinician can use the dominant symptoms to customize a treatment plan to the needs of each patient.
Lifelong Success
Clinicians may consider modifying a patient’s contact lens wear regimen depending on the symptoms of AC and DED. The severity of the disease will help determine whether to initiate treatment prior to lens wear in neophyte wearers or whether lens wear should be discontinued in established wearers. Modifying the replacement schedule or lens material may help combat allergy and dry eye symptoms. Daily replacement is often ideal, as it provides a clean lens surface and minimizes exposure to lens care products.
While patients often turn to OTC lubricants to relieve dry, itchy eyes, these agents can have both a positive and negative effect on contact lens wear. The vehicle can provide short-term relief of ocular symptoms, yet other ingredients such as preservatives may aggravate the ocular surface. Clinicians should recommend preservative-free or contact lens “approved” options to avoid toxicity often exacerbated by the chemicals binding to the lens material.
 |
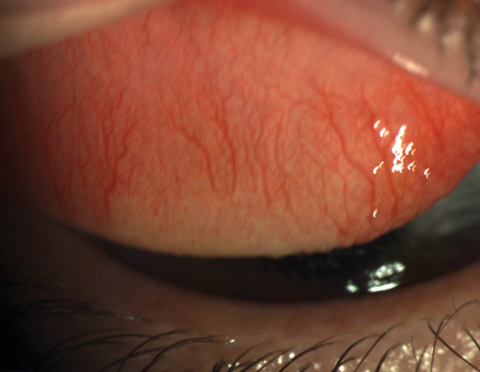
| Ocular allergy often includes chemosis, conjunctival injection and eyelid edema. Click image to enlarge. |
While consensus exists that lens material and comfort are intertwined, it is difficult to be prescriptive regarding lens materials. Despite advances in technology, our understanding of the impact of varying contact lens designs is limited.20 Today’s lens materials defy traditional FDA groupings, and older dogma relating to water content or even the inclusion of silicone is too simplistic to characterize recent technological advances. Consequently, practitioners must use their best professional judgment and consider the unique needs of each patient when prescribing contact lenses.
Beyond the lens material, preservative-free lens care regimens or multipurpose brands with known formulations are suitable choices, given the association of lens-solution interactions with adverse events.21 Clinicians should caution patients on using store brands, which may not incorporate the newest products or may shift in formulation over time. Educate patients that the lens care system may influence comfort, particularly for sensitive wearers.
While some strategies are appropriate for all contact lens wearers, others are specific to certain ages and life phases:
Childhood. In the past, children younger than 10 were fit only when contact lenses were deemed medically necessary—as in the case of unilateral pediatric aphakia or other circumstances where amblyopia may result from high or anisometropic refractive error.22 Recently, however, the interest in fitting children with contact lenses has shifted from correcting refractive error to slowing progression of myopia.23 Given the prevalence of myopia and the potential benefits of intervening with contact lenses, this trend is likely to continue.24,25
Atopic conditions can be a concern in this group, given the propensity for allergies in pediatric patients.18 Parents and other caregivers are integral to the successful management of both contact lenses and adjunctive therapy for allergies. Children generally will benefit from straightforward lens care regimens, avoidance of eye drops when possible and management of coexisting conditions.
Adolescence to young adulthood. Most providers are adept at managing these patients, as they are traditionally motivated to wear contact lenses and are often easy to please. This population is highly involved with activities away from home. While parents may oversee the care of a young adolescent between the ages of 10 and 14, independence increases with age and older adolescents ages 15 to 19 and young adults ages 20 to 24 learn to manage their own ocular health.22
Providers can work with teens (and parents) and young adults to schedule periodic follow-up for contact lens evaluations and anterior segment conditions. Patients who attend school out of town merit special consideration; they benefit from additional education in proactively scheduling health care visits, managing health insurance, ordering ophthalmic materials and accessing prescription medications. While dry eye is relatively rare in this group, atopy is common.8,18 Furthermore, corneal inflammatory events are more prevalent in older teens and young adults than in younger or older contact lens wearers.26,27 An ample supply of lenses (i.e., ‘pantry effect’), back-up spectacles and instructions for accessing care when away from home go a long way to minimize the sequela of adverse events.28 Older teens and young adult wearers may benefit from advice about risky behaviors that are associated with corneal infectious or inflammatory events and are more prevalent in this age group, such as water exposure, napping in contact lenses and overnight lens wear.29
Pre-presbyopic adults. These patients are also relatively easy to manage regarding vision expectations, access to care and patient education. As discomfort and dryness are the primary reasons for contact lens discontinuation, these patients often benefit from preemptive management of coexisting dry eye, allergy or both.10,11 Moreover, the Vision Council reports that more than 60% of these patients report digital eyestrain and they may be candidates for contact lenses designed for digital device users.30
Pregnancy. This has been associated with contact lens intolerance and changes in refractive error.31,32 Contact lens wearing experiences during this time frame are unpredictable and vary with the patient and the pregnancy.33 Proactive advice on contact lens management and anterior segment conditions can help patients plan accordingly. This might be an ideal time to update spectacles for part-time wear and maximize convenience with daily disposables.
Presbyopia and beyond. While refractive management may be more complex in patients with presbyopia, practitioners have a plethora of products to choose from, increasing the chance of meeting the patient’s vision needs. This population may benefit from increased emphasis on dry eye management, potentially with less concern about atopic disease. Furthermore, additional care may be required with more mature patients who may present with other ocular and systemic conditions.
Post-surgery. Most patients choose refractive surgical options to decrease their dependence on vision correction. However, contact lenses may be necessary post-surgery to fine-tune vision (astigmatism, presbyopia) or manage unexpected outcomes (anisometropia, corneal ectasia). As LASIK is an established risk factor for dry eye, practitioners may devote additional attention to signs and symptoms of dry eye in this population.8
Although dry eye and allergy often present additional deterrents to contact lens wear, they shouldn’t prevent most patients from successfully wearing contact lenses. The first step to ensuring success is properly educating patients on the particulars of lens wear when experiencing dry eye, allergy or both—including lens replacement and care products. Clinicians can further tailor dry eye disease and allergic conjunctivitis management to individual patients of all ages and life phases to promote healthy and comfortable lens wear. Don’t let allergy or dry eye prevent lifelong contact lens success.
Dr. Wagner is a professor of clinical optometry and director of extern programs at Ohio State University. She is a diplomate in the Cornea, Contact Lens and Refractive Technologies Section of the American Academy of Optometry and a distinguished practitioner and fellow in the National Academies of Practice in Optometry.
1. Rosario N, Bielory L. Epidemiology of allergic conjunctivitis. Curr Opin Allergy Clin Immunol. 2011;11(5):471-6. |

