A congenital retinal macrovessel (CRM) is a rare ocular finding that is often noted incidentally on fundus evaluation. Some affected individuals may be visually asymptomatic, while others could present with decreased visual acuity caused by several different etiologies.
A congenital retinal macrovessel is frequently described as an enlarged single vessel that emanates from the optic nerve or retinal arcade and crosses the horizontal raphe. Macrovessels often perfuse a large area of the fundus and may lead to an anastomosis between the arterial and venous vasculatures.
This case report illustrates how you can effectively differentiate a retinal macrovessel from other vascular anomalies, such as racemose hemangioma, arteriovenous malformation (AVM) or other hamartomas of the retina and central nervous system.
 | |
|
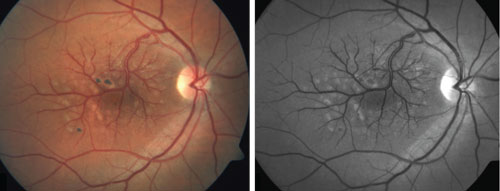
1, 2. Color (left) and red-free (right) fundus photographs of the right fundus
revealed congenital retinal macrovessel (CRM) formation. The parafoveal areas of hypopigmentation were caused by previous focal laser treatment for cystoid macular edema. The aberrant vein does not cross over the foveola; however, the patient may still note a small angioscotoma. |
History
A 45-year-old white male presented for an initial eye examination. His chief complaint was difficulty focusing at near with his current bifocal prescription. He also complained of intermittent irritation in his right eye that had persisted for several months, as well as frontal headaches that had continued for at least eight months. The patient reported that over-the-counter analgesics and bed rest relieved his headaches.
His systemic history was remarkable for hypertension, hyperlipidemia, environmental allergies, major depressive disorder, lower back pain, claw foot, sleep apnea, and a left arm AVM that was surgically corrected in 1994.
Current medications included 40mg citalopram, 25mg hydrochlorothiazide, 800mg ibuprofen TID, 100mg metoprolol, 20mg simvastatin and 25mg trazodone. At a recent physical, his blood pressure measured 118/75mm Hg.
He reported that his last ocular examination three years before uncovered “something in the back of his right eye.” He also stated that he underwent an unknown laser procedure on his right eye approximately 10 years prior.
Diagnostic Data
His best-corrected visual acuity was 20/25 OD and 20/20 OS. Extraocular motility was full and unrestricted OU. Confrontation fields were unremarkable OU. Both pupils were equal, round and reactive to light, with no evidence of an afferent defect in either eye. Slit-lamp examination was unremarkable OU.
The anterior chamber was deep and quiet in both eyes. Intraocular pressure measured 12mm Hg OD and 11mm Hg OS. Fundoscopy with a 78D lens showed a 0.10 x 0.10 cup-to-disc ratio, with healthy neuroretinal rim tissue in both eyes.
 |
|
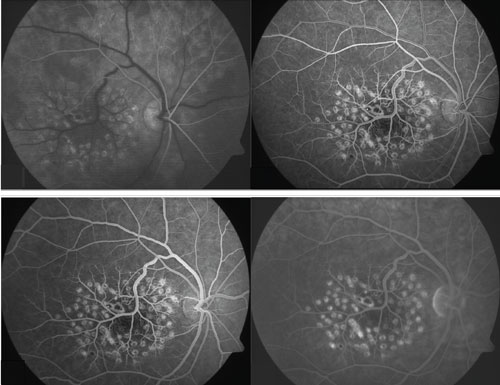
| 3-6. Fluorescein angiography of the right eye. Arterial phase showed full arterial filling in all quadrants (top left); arteriovenous phase demonstrated laminar flow of venous arcades and early CRM filling (top right); venous phase clearly showed the multiple aberrant arteriovenous anastomoses in the foveal avascular zone (bottom left); late-phase fluorescein angiography showed no vascular leakage (bottom right). |
The right fundus had a large retinal vessel branching from the superotemporal arcade, crossing over the horizontal raphe. The macula exhibited several areas of mottling and parafoveal atrophy, which were due to a previous focal laser treatment performed in 2004 (figures 1 and 2). The retinal examination of his left eye was unremarkable. The periphery of both eyes was flat and attached.
Fluorescein angiography of the right eye showed irregular arteriovenous anastomoses, with early filling of the aberrant retinal vessel during the venous phase (figures 3-5). There was no evidence of macular leakage throughout the study (figure 6).
Of particular interest was the presence of capillary vasculature in the foveal region of the right eye. Here, the aberrant vessel had formed additional anastomoses with inherently normal arterioles. A macular cube optical coherence tomography scan taken on Cirrus HD-OCT (Carl Zeiss Meditec) revealed the absence of a foveal pit, as well as multiple areas of superficial hyper-reflectivity that corresponded to the presence of retinal vasculature branches located within the foveal avascular zone (figure 7).
Diagnosis
We diagnosed the patient with a congenital retinal macrovessel in the right eye.
Follow-Up
Due to his recent onset of headaches and previously discovered left arm AVM, we referred the patient for a neurologic workup to rule out an intracranial and central nervous system hemangioma. He underwent an MRI with gradient-recalled echo sequencing, which showed no evidence of cerebral AVM.
The examining neurologist diagnosed him with tension headaches and started him on 10mg cyclobenzaprine TID and 25mg nortriptyline QHS. Then, he was scheduled for a six-month follow-up evaluation. Since then, the patient has remained asymptomatic, with no additional sequelae.
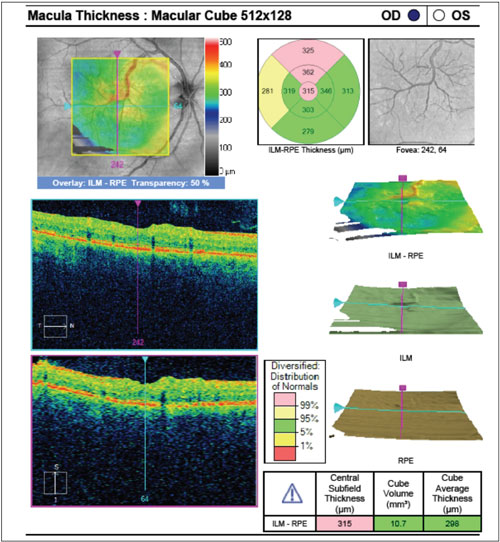 | |
| 7. Spectral-domain optical coherence tomography macular cube of the right eye. The scan was centered on the fovea and exhibited an irregular foveal architecture. The CRM disrupts the foveal avascular zone, creating shadows caused by the prominent retinal vasculature. Shadowing on an OCT scan also may be seen with vitreal floaters, congenital hypertrophy of the retinal pigment epithelium (CHRPE), dense collection of blood, cotton-wool spots, exudates, retinal pigment epithelium hyperplasia, intraocular foreign body, dense pigmented scars, choroidal nevi and thick subretinal neovascular membranes.14,15 |
Discussion
Congenital retinal macrovessels were first identified in 1869 and were later defined as a large aberrant artery or vein that crosses the horizontal raphe, with minimal to no effect on vision or color perception.1,2
CRMs are rare, with an estimated prevalence of one in 200,000 individuals.3
The presentation is often described as a single, enlarged vessel that emanates from the optic nerve. Venous CRMs are far more common than arteriolar CRMs. These vessels usually perfuse a large area of the fundus and also may lead to an anastomosis between the arterial and venous vasculature.4-6
A patient with a congenital retinal macrovessel may present with normal or reduced visual acuity.5,7,8 Etiologies of decreased visual acuity include foveal ectopia, subfoveal retinal pigment epithelium alteration, foveal cysts and angioscotomas created by the path of the retinal vascular abnormality coursing through the central fovea.5,7,8 Less commonly, valsava retinopathy and retinal macroaneurysm also have been identified as secondary causes of CRM-associated visual loss.7,9
Several other similarly appearing retinal vascular disorders may complicate accurate diagnosis of the abnormality. These include retinal arteriovenous communication, retinal hamartoma, capillary hemangioma, prepapillary vascular loops, hereditary or acquired retinal tortuosity, and racemose hemangioma or arteriovenous malformations associated with Wyburn-Mason syndrome.3,5 Although a congenital retinal macrovessel can be diagnosed on clinical examination alone, it is critical to rule out other retinal and systemically associated conditions.
Racemose hemangioma is a benign AVM that can occur independently or as a component of Wyburn-Mason syndrome.10 The terms “racemose hemangioma” and “Wyburn-Mason syndrome” are often used interchangeably; however, Wyburn-Mason syndrome is characterized by the subsequent finding of an AVM of the midbrain in the presence of an ipsilateral AVM of the retina.
The retinal manifestations of Wyburn-Mason syndrome include generalized tissue ischemia, retinal hemorrhage, venous occlusion and vitreal hemorrhage. Orbital or optic nerve AVM development can lead to papilledema, proptosis, cranial nerve palsies, conjunctival vasculature dilatation and ptosis. Wyburn-Mason syndrome is a systemic condition that can cause hamartomas of the brain with severe neurologic deficits.11
Intravenous fluorescein angiography is useful in determining the etiology of vision loss, as well as differentiating CRM from other vascular disorders, such as an AVM or the phacomatoses.
The characteristic angiographic findings of a CRM include an early filling and delayed evacuation of venule, dilated surrounding capillary plexus, areas of capillary nonperfusion, hyperfluorescence due to retinal pigment epithelium alterations and leakage from the vascular wall.3,5,7 In contrast, racemose hemangiomas exhibit a direct arteriovenular communication, with retinal vessel stability and evenly distributed staining.13
A congenital retinal macrovessel is a rare ocular finding with an impressive and characteristic pattern that is’s often detected incidentally during ocular examination. Although CRMs do not typically affect vision, secondary alteration of the foveal architecture and the presence of angioscotomas could reduce visual acuity. Fluorescein angiography and ancillary tests, such as optical coherence tomography, may aid in this diagnosis.
CRM are usually benign, however, you must rule out Wyburn-Mason syndrome in the presence of neurologic symptoms. Clinicians should consider an MRI in those who present with suspicious retinal arteriovenous malformations and neurologic symptoms, such as mental changes, headaches, seizures, papilledema and unexplained homonymous hemianopsia. n
Dr. Zimbalist practices at the Harry S. Truman Memorial Veterans’ Hospital in Columbia, Mo.
1. Mauthner L. Lehrbuch der ophthalmoscopie. Vienna, Austria: Tendler; 1869:249.
2. Brown GC, Donoso LA, Magargal LE, et al. Congenital retinal macrovessels. Arch Ophthalmol. 1982 Sep;100(9):1430-6.
3. Gurwood AS, Bailey JT, Pelino CJ. Congenital retinal macrovessel: a case report. Optometry. 2001 Sep;72(9):597-602.
4. Alexander LJ. Congenital and Acquired Anomalies of the Optic Nerve Head In: Primary Care of the Posterior Segment, 2nd ed. Norwalk, Connecticut: Appleton & Lange; 1994:96.
5. Pérez-Carro G, Miranda-Rollón M, Junceda-Moreno C, et al. Congenital retinal macrovessels: A discovery by chance. Arch Soc Esp Oftalmol. 2008 Apr;83(4):273-6.
6. Polk TD, Park D, Sindt CW, Heffron ET. Congenital Retinal Macrovessel. Arch Ophthalmol. 1997 Feb;115(2):290-1.
7. de Crecchio G, Alfieri MC, Cennamo G, Forte R. Congenital macular macrovessels. Graefes Arch Clin Exp Ophthalmol. 2006 Sep;244(9):1183-7.
8. Yanuzzi LA. Pediatric Retina. In: The Retinal Atlas, 1st ed. New York: Saunders-Elsevier; 2010:184.
9. Koizumi H, Iida T, Mori T, et al. Retinal Arteriolar Macroaneurysm and Congenital Retinal Macrovessel. Ophthalmic Surg Lasers Imaging. 2009 Sep-Oct;40(5):513-5.
10. Materin MA, Shields CL, Marr BP, et al. Retinal racemose hemangioma. Retina. 2005 Oct-Nov;25(7):936-7.
11. Lee AG, Roy H. Wyburn-Mason Syndrome. Medscape. Available at: http://emedicine.medscape.com/article/1219502-overview. Accessed November 7, 2014.
12. Marks ES, Adamczyk DT, Thomann KH. Primary Eyecare in Systemic Disease. Aksionoff EB (ed.). In: Wyburn-Mason Syndrome. Norwalk, Connecticut: Appleton & Lange; 1995:344-7.
13. Richard G, Soubrane G, Yanuzzi L. Neoplastic Diseases. In: Fluorescein and ICG Angiography: Textbook and Atlas, 2nd ed. New York: Thieme; 1998:338.
14. Reed B, Glabe, D, Yudcovitch L. Ocular Coherence Tomography Guide. Pacific University: Common Knowledge. Available at: http://commons.pacificu.edu/cgi/viewcontent.cgi?article=1011&context=coofac. Accessed November 7, 2014.
15. Upender K. Clinical Applications of Optical Coherence Tomography in Ophthalmology: Selected Topics in Optical Coherence Tomography. Intech. Available at: www.intechopen.com/books/selected-topics-in-optical-coherencetomography/clinical-applications-of-optical-coherence-tomography-in-ophthalmology. Accessed November 7, 2014.

