 |
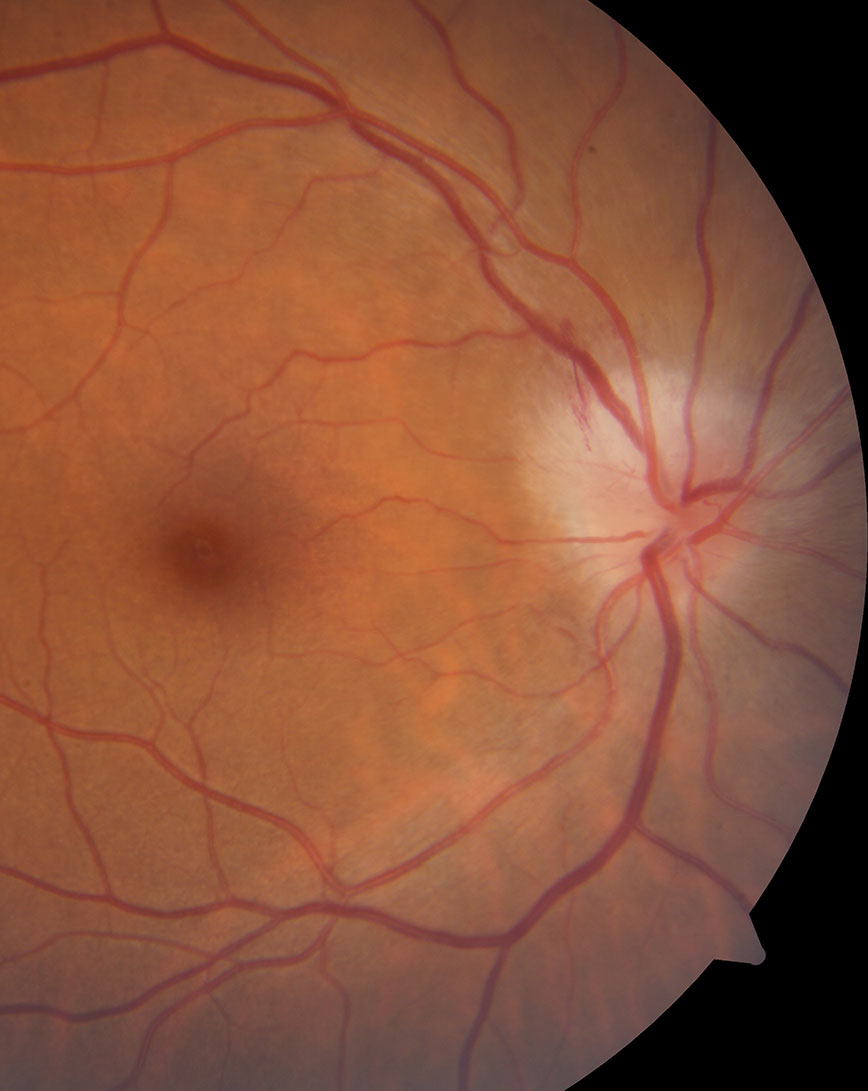
| Patients with pediatric optic neuritis may be at increased risk for neurologic autoimmune conditions. Photo: Nate Lighthizer, OD. Click image to enlarge. |
Pediatric optic neuritis (ON) is a rare disease that has not been well characterized. A recent prospective study was the first to evaluate visual acuity (VA) outcomes, recurrence risk and final diagnosis two years post-enrollment. It included 28 participants from 23 pediatric ophthalmology or neuro-ophthalmology clinics in the United States and Canada. The median enrollment age was 10.3, 46% of patients were female and 68% had unilateral ON at presentation.
Final diagnoses included isolated ON (40%), myelin oligodendrocyte glycoprotein-associated demyelination (29%), multiple sclerosis (14%), neuromyelitis optica spectrum disease (n=11%) and acute disseminated encephalomyelitis (n=7%). Two participants (7%) had subsequent recurrent ON, two (7%) had a new episode in their unaffected eye and all had multiple sclerosis.
Mean presenting high contrast VA was ~20/125, improving to ~20/25-2 at six months, ~20/25-2 at one year and 20/25-1 at two years. Twenty-four patients (79%) had age-normal VA at two years and 21 (66%) had 20/20 vision or better. The participants without age-normal VA had two-year diagnoses of neuromyelitis optica spectrum disease, multiple sclerosis and isolated ON. Mean presenting low contrast VA was ~20/500-2, improving to ~20/125+2 at six months, ~20/100+1 at one year and ~20/100+2 at two years.
Despite poor VA at presentation, most children had marked improvement in VA by six months, which was maintained over two years, the study authors concluded. “The data suggest that a clinical diagnosis of isolated ON at the time of onset may reduce the risk of recurrence and the development of an associated neurologic condition,” they explained in their paper on the study.
Pineles SL, Henderson RJ, Repka MX, et al. The Pediatric Optic Neuritis Prospective Outcomes study—two-year results. Ophthalmology. March 29, 2022. [Epub ahead of print]. |

