 |
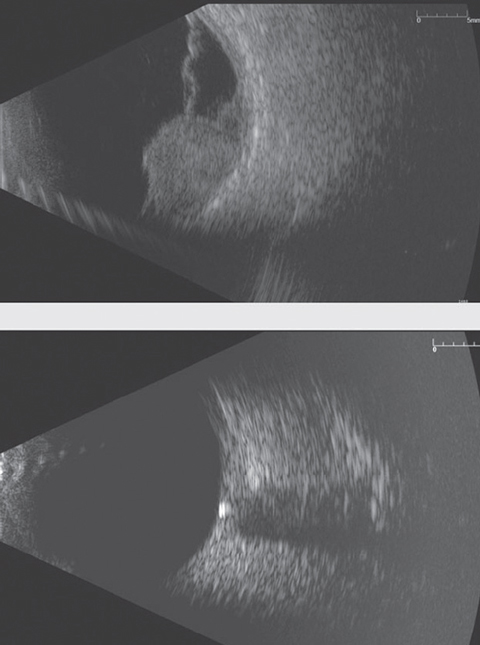
| Ultrasonography can reveal any number of issues, such as choroidal melanoma with overlying retinal detachment, top, and optic nerve drusen, bottom. Recently, reseachers found measuring optic nerve sheath diameter with ultrasonograpy may be a noninvasive method of monitoring ICP. Photos: Nate Lighthizer, OD |
Clinicians have long known intracranial pressure (ICP) plays a critical role in idiopathic intracranial hypertension, and “there has also been debate about its potential role in other disease states such as glaucoma,” says Nate Lighthizer, OD, an associate professor and assistant dean of Clinical Care Services at Oklahoma College of Optometry. “There is current thinking now that perhaps glaucoma is a two-pressure disease: the balance between intraocular pressure and intracranial pressure. So better understanding the role ICP plays in many disease states may be a critical element in the future.”
Unfortunately, the standard test for diagnosing elevated ICP, lumbar puncture (LP), is invasive and painful.1 Recently, researchers have sought noninvasive methods for dynamically monitoring ICP, and think ultrasonography may be the key.1
Researchers in China used ultrasonography to measure the optic nerve sheath diameter (ONSD) in 60 patients admitted for lumbar puncture. After LP, the patients were split into two groups, those with elevated ICP between 200mm H2O and 300mm H2O and those above 300mm H2O. The investigators noted a strong correlation between the ONSD and ICP values on admission, and a strong correlation between the change in ONSD and ICP values one month later. Post-treatment, the elevated ICP and dilated ONSD had returned to normal, the researchers found.1
Other studies have highlighted ultrasonography’s utility in measuring elevated ICP, and this study “adds further evidence for the sensitivity and specificity of ultrasonography for this purpose,” according an editor’s note from Andrew G. Lee, MD, of Houston Methodist Eye Associates in Houston, Texas.
Dr. Lee already uses the diagnostic tool in his practice to: differentiate difficult cases of pseudopapilledema vs. papilledema, follow patients with papilledema with residual post-treatment disc changes, evaluate those whose papilledema may no longer manifest ophthalmoscopically and patients with cerebrospinal fluid shunts and follow patients who refuse or cannot undergo a standard LP for measuring ICP.2
Because of the strong correlation between ONSD and ICP values, and because the ICP decreased as the dilated ONSDs decreased, the researchers believe “ultrasonographic ONSD measurements may be a useful, noninvasive tool for dynamically evaluating ICP.”2
“It is exciting to see that other measurements, such as ultrasound assessments of optic nerve sheath diameter, potentially offer easier, less invasive ways to gain an understanding of a patient’s ICP,” says Dr. Lighthizer. “Certainly, future research will only help to clarify this even more.”
1. Wang L, Chen L, Chen Y, et al. Ultrasonography assessments of optic nerve sheath diameter as a noninvasive and dynamic method of detecting changes in intracranial pressure. JAMA Ophthalmol. 2018;136(3):250-256. |

