 |
A 75-year-old male presented with sudden vision loss in his left eye that had occurred earlier that same day. He reported that his vision was somewhat clearer in the periphery than centrally. There were no accompanying flashes and, although he had a history of floaters, they did not increase in incidence with the loss of vision. He denied eye pain, new-onset headache and jaw claudication. He had not experienced any trauma.
Case
The patient’s ocular history included open-angle glaucoma, for which he was using latanoprost 0.005% in each eye at bedtime. He was also pseudophakic in both eyes. He had phacoemulsification cataract surgery with posterior chamber (PC) intraocular lens (IOL) implantation 27 years earlier. At that time, he was corrected for monovision, with his right eye set for distance and his left eye set for near. He noted that he had never been satisfied with his monovision prescription. He also had YAG laser capsulotomies in both eyes 16 years ago. His medical history was positive for benign prostatic hypertrophy, for which he was taking tamsulosin.
The patient’s entrance acuities with his current glasses were 20/20-1 OD and count-fingers at six feet OS. His vision improved to 20/175 OS with pinhole, but he was still unable to see the near-point chart with his near-corrected left eye. Manifest refraction of the left eye yielded 20/20-2 with a +6.00D sphere lens. Pupils, extraocular motility and confrontation visual fields were normal. Intraocular pressures were 13mm Hg OD and 14mm Hg OS.
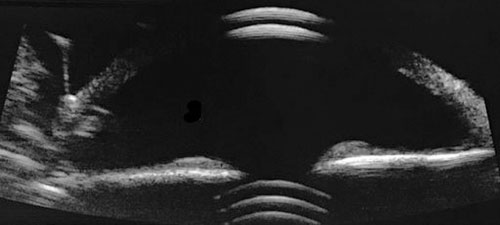
The slit lamp exam showed a stable posterior chamber IOL in the right eye. There was an apparent void with no PC-IOL seen behind the pupil of the left eye. Otherwise, the anterior segments of both eyes were unremarkable. The fundus exam found an optic nerve cup-to-disc ratio of 0.75 but was otherwise unremarkable. The posterior chamber IOL was not visible in the vitreal cavity of the left eye; only when the patient was placed in Trendelenburg’s position did it finally emerge. The PC-IOL was still within the capsular bag and attached by zonules at the six o’clock position, causing a hinge-like phenomenon. It positioned itself inferiorly when the patient sat up. This was confirmed with anterior segment B-scan ultrasonography (Figure 1).
 |
|
Fig. 1. Reverberations of sound waves can be seen from the dislocated posterior chamber IOL/capsular bag complex behind the iris. Click image to enlarge. |
We were able to review the patient’s eye records from 32 years prior. He was a moderate myope in both eyes. His pre-cataract surgery glasses correction was -5.00+1.25x082 OS, and his keratometry measurement was 40.25x41.12 OS. We found that he had significant axial myopia OS, with an A-scan measurement of 28.48mm (axial myopia defined as axial length >26.00mm). Nowhere was there any indication of pseudoexfoliation (PEX) or uveitis history. The patient did not have any connective tissue disorders.
Discussion
IOL dislocation is an uncommon complication following cataract surgery. With respect to time, posterior chamber IOL dislocation is divided into early and late cases. Early cases occur within the first three months of cataract surgery, while late cases happen after.1,2 In general, early cases of PC-IOL dislocation are the result of inadequate posterior chamber IOL fixation within the capsular bag but can also result from a zonular rupture during a traumatic cataract surgery.3,4 Late cases result from progressive zonular weakness and capsular bag contraction years after even uncomplicated cataract surgery.5
More specifically, posterior chamber IOL dislocation can be divided into five catagories:6
- A lens that is decentered within an intact capsular bag. This is most often seen in patients with PEX.
- A lens that is partially subluxed out of the capsular bag, with one haptic in the bag and one haptic out or one haptic in and the optic and other haptic out. This can also result in uveitis-glaucoma-hyphema (UGH) syndrome.
- A lens that is in the ciliary sulcus. An IOL is surgically positioned in the sulcus if there is a compromised capsular bag, meaning there is a tear in the posterior capsule or rupture of the equatorial capsule. Posterior chamber IOL dislocation in this case is referred to as sunset (inferior displacement) or sunrise (superior displacement) syndrome.2
- A PC-IOL that’s in the capsular bag, both of which are dislocated. This is what our patient presented with.
- A PC-IOL dislocated into the vitreal cavity or sitting on the retina.
The first three categories are usually seen within the first three months after cataract surgery (early cases), while the last two usually occur in late cases.
Late, spontaneous PC-IOL dislocation occurs with a cumulative rate of 0.1% after 10 years and 1.7% after 25 years.2 One study found late-case PC-IOL dislocation occurred with virtually all posterior chamber IOL materials and lens designs.7 The same series found that PEX accounted for 50% of all PC-IOL dislocations.7
Other causes included high myopia, trauma, vitreoretinal surgery, retinitis pigmentosa, connective tissue disorders, diabetes, atopic dermatitis, previous angle-closure attacks and even older age, as zonules become more friable with age.2,7 Any condition, including uveitis, that results in the breakdown of the blood-aqueous barrier is also likely to be associated with progressive zonulysis and potentially late-case PC-IOL dislocation.8
Management
Surgery for secondary IOL implantation in the absence of capsular support may include an anterior chamber IOL, an iris-fixed IOL, a transscleral, sutured PC-IOL or a flanged, intrascleral PC-IOL fixation technique.9 In one study, dislocated, in-the-bag PC-IOLs were replaced with anterior chamber IOLs in 60% of patients or repositioned or exchanged and then fixed to the sclera in 40% of patients.1 Surgeons usually try to reuse the current PC-IOL if it is not damaged and if the patient reacted well up until the dislocation.8
Our patient was never satisfied with his monovision correction, so he chose a lens exchange with the new posterior chamber IOL to be set for optimal distance correction.
The corrective surgery was performed with the assistance of a retina surgeon. The surgeon performed a vitrectomy and prolapsed the dislocated posterior chamber IOL/capsular bag complex into the anterior chamber. This lens/bag complex was then removed through a temporally placed scleral tunnel incision. A three-piece acrylic monofocal posterior chamber IOL was passed through this same surgical incision and into the anterior chamber. It was then maneuvered into the posterior chamber with its two haptics externalized through the sclera and secured using the flanged, intrascleral fixation technique.9
At the three-month post-op visit, the patient was no longer on any post-op medications. His uncorrected distance vision was 20/30+2 OS. With a refraction of -0.50 +0.50x174 OS, he was able to see 20/20-1 OS. A +2.50 add yielded 20/20 OS at near. He was happy he did not need distance glasses and satisfied that he only had to use simple reading glasses for near work.
Dr. Skorin is a consultant in the Department of Surgery, Community Division of Ophthalmology at the Mayo Clinic Health System in Albert Lea and Austin, MN. He has no financial interests to disclose.
Dr. Mangan is a board-certified consultative optometrist from Boulder, CO, and a fellow of the American Academy of Optometry. He is an assistant professor in the department of ophthalmology at the University of Colorado School of Medicine. His focus is on ocular disease and surgical comanagement. He has no financial interests to disclose.
1. Gross JG, Kokame GT, Weinberg DV. In-the-bag intraocular lens dislocation. Am J Ophthalmol. 2004;137(4):630-5. 2. Ascaso FJ, Huerva V, Grzybowski A. Epidemiology, etiology and prevention of late IOL-capsular bag complex dislocation: review of the literature. J Ophthalmol. 2015;2015:805706. 3. Matsumoto M, Yamada K, Uematsu M, et al. Spontaneous dislocation of in-the-bag intraocular lens primarily in cases with prior vitrectomy. Eur J Ophthalmol. 2012;22(3):363-7. 4. Wilson DJ, Jaeger MJ, Green WR. Effects of extracapsular cataract extraction on the lens zonules. Ophthalmology. 1987;94(5):467-70. 5. Krėpštė L, Kuzmiene L, Miliauskas A, et al. Possible predisposing factors for late intraocular lens dislocation after routine cataract surgery. Medicina. 2013;49(5):229-34. 6. Stephenson M. How to manage dislocated IOLs. Rev Ophthalmol. 2018;25(10):54-60. 7. Davis D, Brubaker J, Espandar L, et al. Late in-the-bag spontaneous intraocular lens dislocation. Ophthalmology. 2009;116(4):664-70. 8. Stephenson M. How to handle dislocated IOLs. Rev Ophthalmol. 2020;27(11):76-8. 9. Yamane S, Sato S, Maruyama-Inoue M, et al. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-42. |

