 |
Epithelial basement membrane dystrophy (EBMD) is the most common of the anterior corneal dystrophies and one of the most likely etiologies of recurrent corneal erosion syndrome (RCE).1,2 More than 2% of the population is affected.3
The condition typically develops between ages 20 and 50.1 Although considered an age-dependent corneal degeneration, it also seems to have an autosomal dominant method of inheritance.1,4,5 EBMD stems from an inherent dysfunction in basal epithelial cells that results in secretion of abnormal basement membrane extending into the epithelium, as well as accumulation of fibrillogranular material between Bowman’s and the basement membrane and also within the epithelium.3
Over the years our understanding of EBMD has matured, as has our ability to diagnose and manage it. Here, we review causes, symptoms and treatments.
|
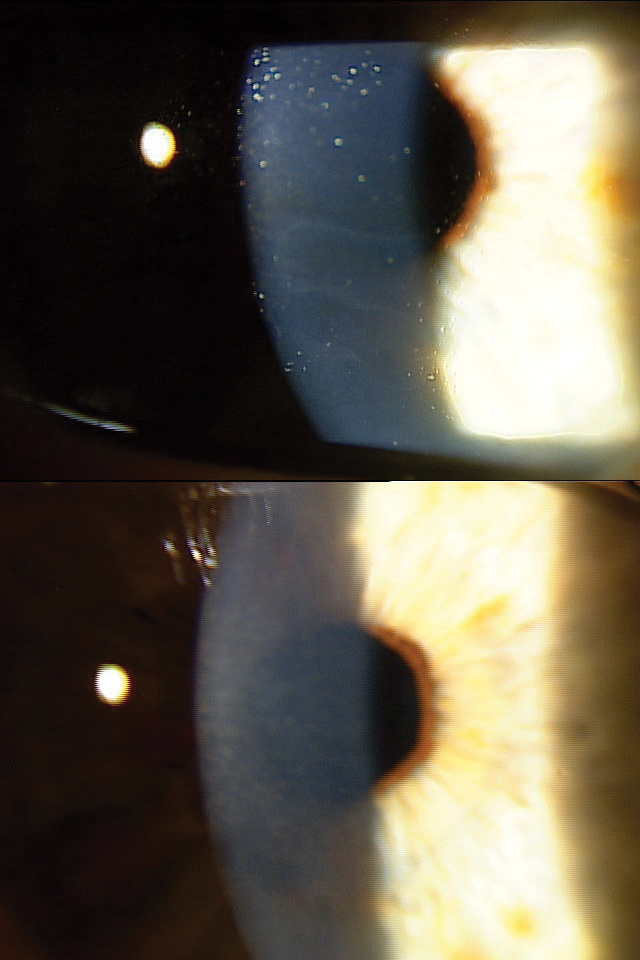
| An EBMD patient before (top) and after (bottom) epithelial debridement and amniotic membrane application. Click image to enlarge. |
Diagnosing EBMD
EBMD is characterized by an abnormal basement membrane that protrudes into the epithelium and the presence of intraepithelial microcysts.1
Diagnosis begins with a careful history and review of symptoms. EBMD is usually asymptomatic, but patients may present with dryness, fluctuating vision, grittiness or photophobia.1 In fact, EBMD patients are often misdiagnosed with dry eye.6
Approximately 10% of patients develop painful, recurrent epithelial erosions.1,3 On slit lamp exam, EBMD is characterized by bilateral (and frequently asymmetric) subepithelial fingerprint lines, geographic map-like lines and epithelial microcysts.1
An obvious feature is the presence of a thickened basement membrane, easily detectable on OCT.1 This thickening can be either localized or diffuse; when substantial, it can account for the corneal surface irregularity, blurred vision and pain that sometimes can accompany EBMD.1 Corneal epithelial cystic lesions appear as hyperreflective dots on OCT and range in size from 20µm to 1000µm.1
EBMD in Cataract Patients
Intervention is important in all EBMD patients, but it’s of particular concern in cataract surgery candidates since accurate keratometry and biometry depend on a clear cornea and smooth surface.7 Any corneal lesion, including EBMD, can have an adverse effect on the reliability of such measurements.7 This, in turn, can impact IOL selection and postoperative visual outcomes.7
In a small retrospective review of EBMD, cataract patients were preemptively treated with superficial keratectomy or phototherapeutic keratectomy (PTK) to evaluate the impact of treatment on biometry, IOL power prediction and suggested IOL toricity.7 Researchers found that spherical IOL power decreased for 18 eyes and increased for three.7 The decrease in power was more than 1.0D for four eyes, 1.0D for seven eyes and 0.5D for seven eyes.7 There were two instances of power increase by 0.5D and one by 3.0D.7 Approximately 67% of patients eligible for toric IOLs had adjustments to the recommended IOL cylinder power after intervention, with a mean change of 1.2D.7
These findings speak to how essential corneal surface optimization is and the difference it can make. For every degree of misaligned toric power, there is a 3.3% loss of correcting effect of the cylindrical power.8 Considering that this study found a mean absolute change of more than 39 degrees of the axis of astigmatism, toric IOL alignment inaccuracies could be quite significant.7
Treating EBMD
First-line therapies for mild asymptomatic cases include artificial tears, ointments, punctal plugs and bandage contact lenses.3,9 More advanced options such as autologous serum eye drops, corticosteroids and cryopreserved amniotic membrane also may be used.9 Medically refractory cases are recommended for surgical treatments, including epithelial debridement before applying amniotic membrane.3 Both debridement with diamond-dusted burr polishing and PTK ablation to the level of Bowman’s have proven effective.3,10-14
We have long been aware of the risks EBMD can pose in LASIK patients: severe corneal epithelial sloughing, epithelial ingrowth (73%), diffuse lamellar keratitis (55%), flap microfolds (18%) and flap melting (36%).15,16 Knowing this, take great care to detect subclinical EBMD prior to elective refractive procedures. Although we also endeavor to diagnose all forms of RCE prior to cataract surgery, sometimes the necessity of the procedure will lower our treatment threshold. But as comanaging optometrists, we must be on the lookout for EBMD in all anterior segment surgical patients. By treating them to the best of our ability prior to referral, we help overcome significant risks, and at the very least, we reduce the likelihood that eager surgical candidates will experience disappointment when their procedure is delayed. ν
Dr. Karpecki is medical director for Keplr Vision and the Dry Eye Institutes of Kentucky and Indiana. He is the Chief Clinical Editor for Review of Optometry and chairman of the affiliated New Technologies & Treatments conferences. A fixture in optometric clinical education, he provides consulting services to a wide array of ophthalmic clients. Dr. Karpecki’s full disclosure list can be found here.
| 1. El Sanharawi M, Sandali O, Basli E, et al. Fourier-domain optical coherence tomography imaging in corneal epithelial basement membrane dystrophy: a structural analysis. Am J Ophthalmol. 2015;159(4):755-763. 2. Lin SR, Aldave AJ, Chodosh J. Recurrent corneal erosion syndrome. Br J Ophthalmol. 2019;103(9):1204-1208. 3. Lee WS, Lam CK, Manche EE. Phototherapeutic keratectomy for epithelial basement membrane dystrophy. Clin Ophthalmol. 2016;11:15-22. 4. Werblin TP, Hirst LW, Stark WJ, Maumenee IH. Prevalence of map-dot-fingerprint changes in the cornea. Br J Ophthalmol. 1981;65(6):401-409. 5. S. Boutboul, G.C. Black, J.E. Moore, et al. A subset of patients with epithelial basement membrane corneal dystrophy have mutations in TGFBI/BIGH3. Hum Mutat. 2006;27(6):553-557. 6. Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II Diagnostic Methodology report. Ocul Surf. 2017;15(3):539-574. 7. Goerlitz-Jessen MF, Gupta PK, Kim T. Impact of epithelial basement membrane dystrophy and Salzmann nodular degeneration on biometry measurements. J Cataract Refract Surg. 2019;45(8):1119-1123. 8. Bauer NJC, de Vries NE, Webers CAB, Hendrikse F, Nuijts RMMA. Astigmatism management in cataract surgery with the AcrySof toric intraocular lens. J Cataract Refract Surg 2008;34:1483-1488. 9. Miller DD, Hasan SA, Simmons NL, Stewart MW. Recurrent corneal erosion: a comprehensive review. Clin Ophthalmol. 2019;13:325-335. 10. Reidy JJ, Paulus MP, Gona S. Recurrent erosions of the cornea: epidemiology and treatment. Cornea. 2000;19(6):767–771. 11. Orndahl MJ, Fagerholm PP. Phototherapeutic keratectomy for map-dot-fingerprint corneal dystrophy. Cornea. 1998;17(6):595–599. 12. Geggel HS. Successful treatment of recurrent corneal erosion with Nd:YAG anterior stromal puncture. Am J Ophthalmol. 1990;110(4):404–407. 13. Tzelikis PF, Rapuano CJ, Hammersmith KM, Laibson PR, Cohen EJ. Diamond burr treatment of poor vision from anterior basement membrane dystrophy. Am J Ophthalmol. 2005;140(2):308–310. 14. Pogorelov P, Langenbucher A, Kruse F, Seitz B. Long-term results of phototherapeutic keratectomy for corneal map-dot-fingerprint dystrophy (Cogan-Guerry) Cornea. 2006;25(7):774–777. 15. Rezende RA, Uchoa UC, Cohen EJ, et al. Complications associated with anterior basement membrane dystrophy after LASIK. J Cataract Refract Surg 2004;30(11):2328-31. 16. Perez-Sntonaja JJ, Galal A, Cardona C, et al. Severe corneal epithelial sloughing during LASIK as a presenting sign for silent epithelial basement membrane dystrophy. J Cataract Refract Surg 2005;31(10):1932-7. |

