Is it possible to have keratoconus in only one eye? At least some patients seem to. Their good eyes show no detectable sign of keratoconus.
The question of unilateral keratoconus sounds strictly theoretical, without any clinical relevance. Indeed, if it werent for the popularity of LASIK, this entire question would not even arise. But when one of these uncommon patients asks you if he can have LASIK on the so-called good eye, this question goes from theory to hard, worrisome reality. Case in point: The recent $7 million malpractice award involving LASIK in a case of equivocal keratoconus.1
Diagnostic Data
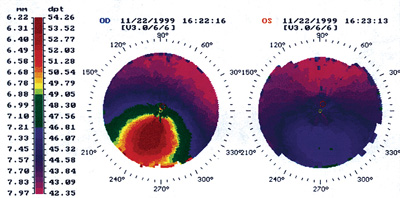
Regardless of the legal ramifications, does unilateral keratoconus exist in individual patients? Take Jack for example. He is a 47-year-old white male with apparent unilateral keratoconus (see below). His good left eye demonstrates a best spectacle-corrected acuity of 20/15, with no Vogts striae, Fleischers ring or corneal scarring. Can Jack undergo LASIK on his good left eye without incurring undue risk?
 |
|
Normalized corneal topographies show apparent unilateral keratoconus in this 47-year-old male patient. |
But, by all accounts, Jacks left eye looks normal. Also, hes 47; waiting several more years will not likely produce signs of keratoconus, as the onset of keratoconus rarely begins after age 30.4 In fact, keratoconus progression typically arrests during the third or fourth decade of life.5 But is it possible that his left eye, despite appearances, really does have keratoconus?
Bilateral Evidence
My recommendation: Patients like Jack should not undergo LASIK.
Until research proves otherwise, the literature suggests there is no such thing as unilateral keratoconus. Most likely, presentations of unilateral keratoconus are actually highly asymmetric presentations of a bilateral disease. Our existing clinical measurements may simply lack sensitivity in detecting the disease in both eyes.
Researchers showed a decade ago that many cases of unilateral keratoconus were actually bilateral.6 At that time, very few clinicians had corneal topographers to assist in detecting keratoconus. These researchers led a retrospective review of 200 patients diagnosed with keratoconus. Using examination data, including slit-lamp findings and Polaroid Corneascope photographs, they identified eight patients as having unilateral disease. They recalled those eight patients for topographical measurements using a computer-assisted videokeratoscope. On corneal topography, seven of the eight apparently normal eyes showed inferior steepening, which suggested keratoconus.
Similarly, another study used videokeratography to observe progression of keratoconus in clinically normal eyes.7 The researchers found that half the patients identified with unilateral keratoconus progressed to the bilateral form within 16 years; most of these patients (83%) progressed to the bilateral form within the first six years of onset.
By extension, patients like Jack might have milder keratoconus in their good eye to the point that even corneal topography does not demonstrate any abnormalities. Studies have shown that 1.83% to 4% of patients who have keratoconus show a unilateral presentation at the time of examination, even when considering appearance of corneal topography.8,9
As new diagnostic technologiessuch as wavefront aberrometry, pan-corneal pachymetry and posterior corneal topographyenter the mainstream, perhaps one or more will demonstrate that those unilateral cases are indeed bilateral. As an example, one study of wavefront aberrometry showed an elevated amount of higher-order aberrations among keratoconus patients, especially coma.10 Characteristic changes in wavefront patterns over time might signal keratoconus.
Ultimately, the proof of bilaterality may require genetic lab tests for detecting the presence of certain corneal proteases and inhibitors. (Several studies have implicated keratoconus with the presence of elevated levels of degradative enzymes and/or reduced levels of protease inhibitors.11) Until then, we should assume that all keratoconus is bilateral.
Patients who have highly asymmetrical keratoconus should not have LASIK, even on a good eye. Conservative treatment with glasses or contact lenses is more appropriate. Only a select number of keratoconus patients are adequate candidates for refractive surgery, namely non-ablative procedures such as intracorneal ring or phakic intraocular lens implantation.
|
Study Enrollment Under Way |
1. Lin A. Former banker awarded $7M in damages from LASIK eye surgery. New York Law Journal 2005 Aug 1. www.law.com/jsp/article.jspid=1122627916703. (Accessed 21 Feb 2006).
2. Amoils SP, Deist MB, Gous P, et. al. Iatrogenic keratectasia after laser in situ keratomileusis for less than -4.0 to -7.0 diopters of myopia. J Cataract Refract Surg 2000 Jul;26(7): 967-77.
3. Argento C, Cosentino MJ, Tytiun A, et al. Corneal ectasia after laser in situ keratomileusis. J Cataract Refract Surg 2001 Sep;27(9):1440-8.
4. Hall KGC. A comprehensive study of keratoconus. Br J Physiol Opt 1 963; 20:215-256.
5. Rabinowitz YS. Keratoconus. Surv Ophthalmol 1998 Jan-Feb;42(4):297-319. Review.
6. Rabinowitz YS, Nesburn AB, McDonnel PJ. Videokeratography of the fellow eye in unilateral keratoconus. Ophthalmology 1993 Feb; 100(2):181-6.
7. Li X, Rabinowitz YS, Rasheed K, Yang H. Longitudinal study of the normal eyes in unilateral keratoconus patients. Ophthalmology 2004 Mar;111(3):440-6.
8. Holland DR, Maeda N, Hannush SB, et. al. Unilateral keratoconus. Incidence and quantitative topographic analysis. Ophthalmology 1997 Sept;104(9):1409-13.
9. Lee LR, Hirst LW, Readshaw G. Clinical detection of unilateral keratoconus. Aust N Z J Ophthalmol 1995 May;23(2): 129-33.
10. Maeda N, Fujikado T, Kuroda T, et al. Wavefront aberrations measured with Hartmann-Shack sensor in patients with keratoconus. Ophthalmology. 2002 Nov;109(11):1996-2003.
11. Zhou L, Sawaguchi S, Twining SS, et al. Expression of degradative enzymes and protease inhibitors in corneas with keratoconus. Invest Ophthalmol Vis Sci 1998 Jun;39(7): 1117-24.

