 |
Q:
I just saw a 64-year-old female patient who casually mentioned that she noted a ‘black shade’ temporarily obscuring her superior field in one eye. How seriously do I take this?
A:
“A chief complaint of transient monocular vision loss (TMVL) should always raise a red flag,” says Kristen Thelen, OD, assistant professor of ophthalmology at Emory Eye Center in Atlanta. “Slow down, and take a detailed look at the patient’s medical history and chief complaint to assess the gravity of the situation.”
Retinal Ischemia
There are ample causes of TMVL, but transient ischemic attack (TIA) is the most common. Retinal ischemia can be a result of underlying vascular disease, such as giant cell arteritis (GCA), atherosclerosis or cardiac abnormalities. These conditions can be visually devastating or, worse yet, result in a stroke.
Due to the gravity of these vascular etiologies, evaluate patients with TMVL urgently. “Age is a key factor when determining the most appropriate next step,” Dr. Thelen says. “Patients older than 50 who experience TMVL need a work-up to rule out GCA.”
Asking your patients about jaw claudication, headache and scalp tenderness is important, but even in the absence of symptoms, order blood work in a timely fashion. Also consider cartotid artery disease and listen for bruits in-office as an initial screening.
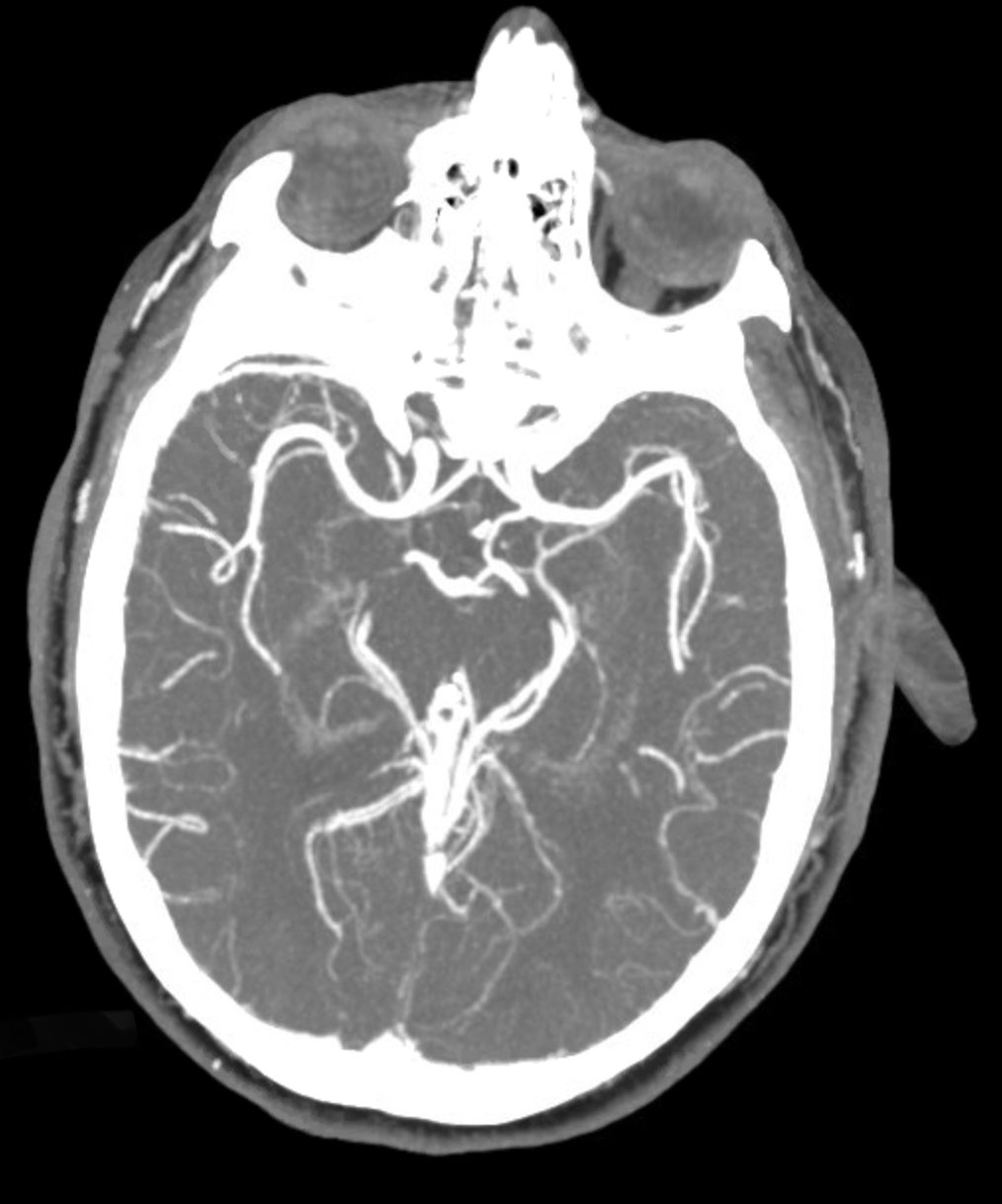 |
| A well-timed CTA can rule out an ischemic or hemorrhagic event for your patient. Click image to enlarge. |
Symptom Assessment
Transient vascular events are typically painless and occur within seconds. Patients often describe a progressive “shade” or “curtain” that leads to “dim” or “black” vision. The entire episode usually lasts a few minutes but never more than an hour.
Photopic symptoms such as flashes, jagged lines and colors are rarely associated with vascular occlusive events. Those tend to be more migrainous or caused by retinal traction. “Remember that ocular migraines with visual auras are typically binocular,” Dr. Thelen points out. Showing your patient a picture of a typical migraine aura can help in ruling that diagnosis in or out.
Don’t Delay
Retinal TIAs, such as branch retinal, central retinal and ophthalmic artery occlusions, have the same mechanism as central nervous system TIAs and carry the same risk of stroke and cardiovascular disease. According to a 2012 study, nearly 25% of patients with acute retinal ischemia had acute brain infarctions.1
“We should refer our TMVL patients with a suspected vascular etiology to a stroke center or hospital emergency department (ED) for a same-day work-up,” Dr. Thelen advises. “We send hemispheric TIAs without a second thought, so we should have the same standard for retinal TIAs.”
Make sure to follow appropriate stroke guidelines. Calling the ED ahead of time and sending patient records always helps, Dr. Thelen adds. The initial work-up will include a CT scan of the brain to rule out bleeding, and labs to rule out GCA. If the patient is a six or higher on the NIH stroke scale, computed tomography angiography (CTA) is usually ordered to rule out large vessel occlusion (i.e., middle cerebral artery stroke). Additional tests include carotid duplex, MRI of the brain and orbits and MRA of the head and neck.
“I connect with the patient a week after sending them to the ED to make sure everything went smoothly,” Dr. Thelen notes. “Patients are typically grateful you sent them for a work-up, and they appreciate the follow-up call as well.” There is usually no need for a follow-up eye exam, so use the phone call as an opportunity to remind them to keep their annual eye appointments.
| 1. Dattilo M, Newman NJ, Biousse V. Acute retinal arterial ischemia. Ann Eye Sci. 2018; 3:28. |

