 |
Writing about a disease we know so little about is challenging, especially considering how rapidly this public health crisis is evolving. At the risk of being outdated before the ink on this page dries, I’d like to attempt to share with you what we currently know about coronavirus, highlighting what it means for optometrists in particular.
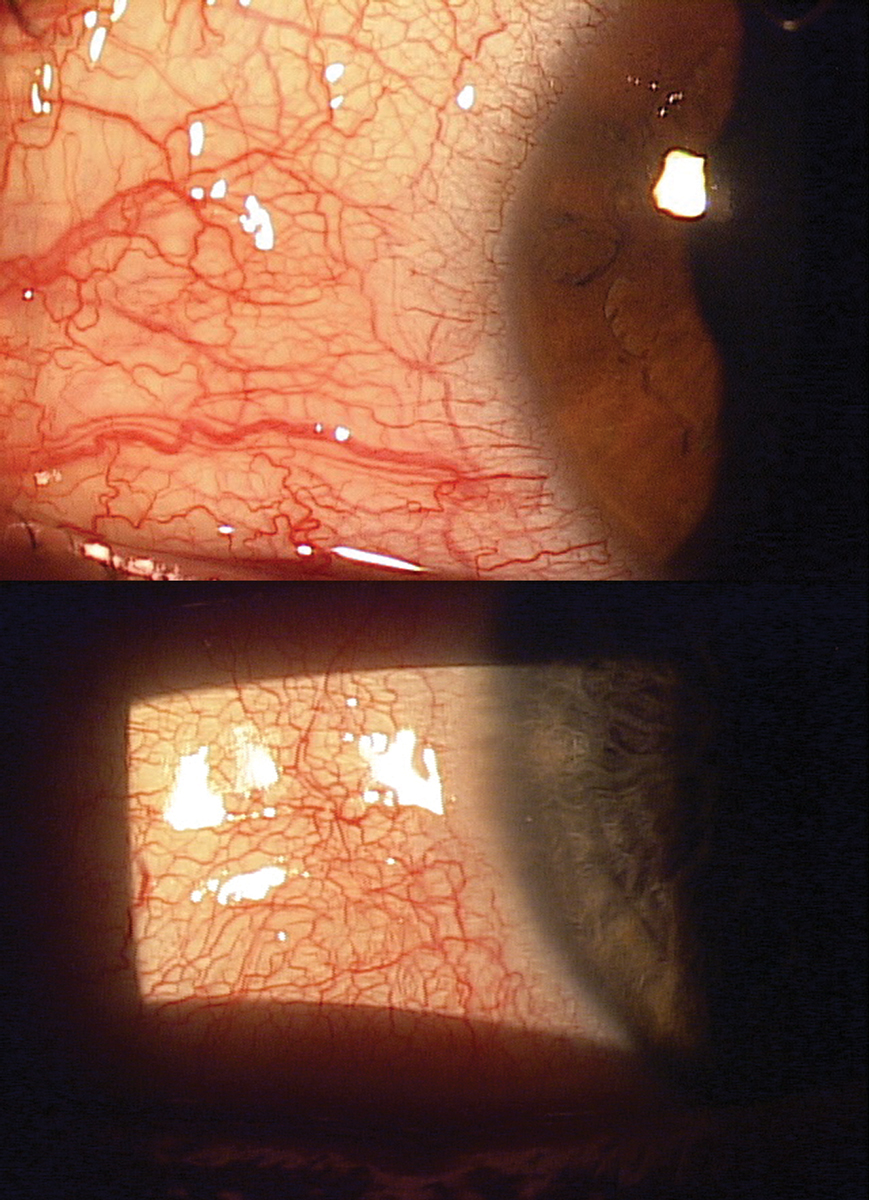 |
These images show different patients with a common disease—viral conjunctivitis. The novel coronavirus currently threatening the planet can present quite similarly to these patients. Click image to enlarge. |
Coronavirus and Influenza Are Not Comparable
Over the past few weeks, our understanding of coronavirus has evolved. Initially, many healthcare providers worried about alarming patients and compared the disease to the flu when discussing prevention. This seemed to quell fears about the unknown virus that patients only heard about on international news broadcasts.
In the long run, making Americans feel too safe may isn’t always ideal either. We see evidence of this every day in patients who assume that common-sense hand washing will stop this virus in its tracks and it will vanish from existence in no time. This approach is one of several reasons why, on March 11, the World Health Organization (WHO) officially declared coronavirus a pandemic, with the agency’s Director General citing “deep concern” about “alarming levels of inaction.”
Unlike influenza, coronavirus has no vaccine, is exceedingly virulent and has a high transmissibility rate. To put it into perspective, every year about 0.1% of people who get the flu die. This is why we advocate so strongly for influenza vaccination. But with no vaccine for coronavirus, the mortality rate of coronavirus is exponentially higher. Consider the mortality data out of Italy, which as of March 10 was above 5% and rising. In other words, for every person who dies of the flu, 50 could die as a result of this coronavirus.
Admittedly, Italy has an unusually high elderly population, but even in communities where mortality is closer to 1%, we’re looking at a disease that’s at least 10 times more deadly and spreads much more quickly. Consider: on February 20, Italy had identified only a single case of coronavirus. Less than 20 days later, more than 9,000 people in Italy had contracted it.
Frames and Contacts are Both a RiskAs is often the case in times of national crises, misinformation can run rampant. Here’s some ways optometrists can use their authoritative positions to keep patients informed. Contacts are safe, but keep hands clean—By now, vigilant hand washing should be a no-brainer, but be sure to emphasize “careful and thorough hand washing with soap and water followed by hand drying with unused paper towels” for contact lens wearers “before every insertion and removal.” Spectacles aren’t immune—Sure, spectacle wearers don’t touch their eyes with the frequency that contact lens wearers do, but that doesn’t mean they’re risk-free. The virus can remain on hard surfaces for hours to days and can be transferred to spectacles from fingers, faces or just from sitting around on other unclean surfaces, as reading glasses especially often do.
|
Promote Preparedness
The WHO didn’t declare a pandemic so the world would fall into a state of hysteria or despair. They did it to prevent the situation from getting worse, assuring a world audience that “all countries can still change the course of this pandemic.”
What does this mean for optometrists? In short, although we should continue to reassure patients, we must balance our rhetoric so that we impress upon them how important it is to prevent the spread of disease to at-risk patients. As citizens, it is our social responsibility to protect the welfare of elderly patients, newborns and anyone else in harm’s way. Primary care providers must make this a key takeaway when counseling patients.
Social media is buzzing with debate on this hot topic, and patients’ views are highly politicized and polarizing, but the one piece of advice that I personally took to heart came from a doctor who reminds us that “the opposite of panic isn’t calm—it’s preparedness.”
ODs to the Front
Eye care practitioners have a unique role to play in preparedness. Coronavirus is predominantly transmitted through direct or indirect contact with mucous membranes in the eyes, mouth or nose.1 In fact, according to an American Academy of Ophthalmology alert, several reports suggest the virus can cause conjunctivitis and possibly be transmitted by aerosol contact with the conjunctiva.
The conjunctivitis presents similarly to other viral conjunctivitis cases with conjunctiva injection and hyperemia and discharge that is typically clear or mucin-like. A study of 30 patients hospitalized for COVID-19 in China suggests that it can infect the conjunctiva and cause conjunctivitis, and virus particles are present in ocular secretions.2 As such, a report in Lancet says doctors examining suspected cases should wear protective eyewear and gloves.3
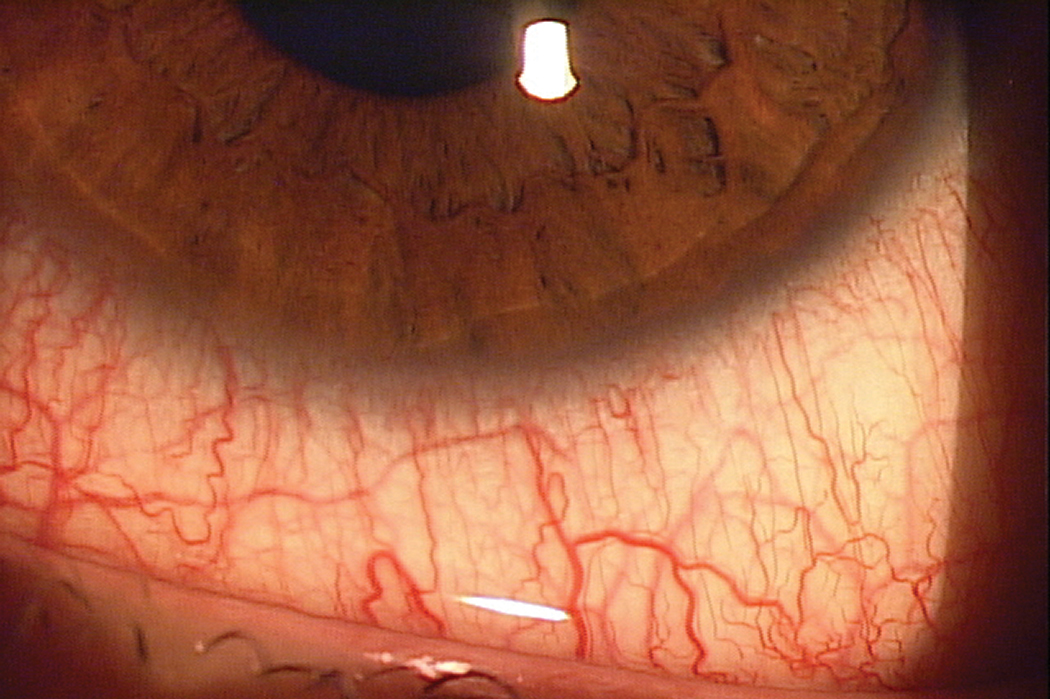 |
| The conjunctiva is among the tissues that are likely to be penetrated by the conronavirus. No treatment exists yet, but identifying infection early can assist in management. Click image to enlarge. |
Until we know more about virus, we need to focus on prevention. This begins with a healthy diet, plenty of rest and vigilance about good hygiene. I’ve taken active steps to remind every patient to wash their hands often, stay hydrated and eat healthy foods. I also recommend they consider taking vitamin C and purchasing hypochlorous acid spray. Hypochlorous acid demonstrates broad-spectrum activity and may help prevent or treat ocular symptoms, while vitamin C is currently in Phase II trials for the clinical management of severe acute respiratory infection due to coronavirus.4
We must question patients with conjunctivitis about recent or current flu-like symptoms, including fever, cough or respiratory difficulties. We may need a thermometer such as a tympanic or forehead type device on hand.
The optometrist’s role here is to educate patients who present to us regularly on the importance of good hygiene habits, nutrition and health. Additionally, ODs must be especially cognizant of any conjunctivitis that presents to our clinics at this time.
1. Peiris J, Yuen K, Osterhaus A, Stohr K. The severe acute respiratory syndrome. N Engl J Med. 2003;349:2431-41. 2. Xia J, Tong J, Liu M, et al. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. February 26, 2020 [Epub ahead of print]. 3. Lu C, Liu X, Jia Z. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395(10224):e39. 4. Wang L, Bassiri M, Najafi R, et al. Hypochlorous acid as a potential wound care agent: part I. Stabilized hypochlorous acid: a component of the inorganic armamentarium of innate immunity. J Burns Wounds. 2007;6:e5. |

