 |
By far, floaters are the most common complaints in a retina practice. Chronic floaters may significantly impact a patient’s quality of life, affecting everything from reading to driving. Their causes can include any number of processes, such as posterior vitreous detachment (PVD), myopic vitreopathy, vitritis, vitreous hemorrhages, retinal detachment, retinal breaks and vitreous liquefaction.
Managing these underlying causes remains the primary treatment approach for the associated floaters. Still, most floaters are benign and are treated simply with observation, which does not always address the patient’s symptomology.
The surgical treatment of floaters remains a topic of conflict, especially given that many patients are young, phakic and have good preoperative visual acuity. Although treatment is associated with significant resolution of symptoms, there is a small but not insignificant rate of complications such as retinal, vitreous or suprachoroidal hemorrhages, cataract formation, endophthalmitis, macular edema and iatrogenic retinal breaks and/or retinal detachments.
In our practice, Dr. Rashid Taher has found floaterectomy—pars plana vitrectomy (PPV) for the treatment of floaters—to be a viable option for well-selected patients, yielding favorable outcomes, high surgical success rate and minimal associated complications. The key to our success lies in our careful assessment of individual inclusion criteria prior to surgical intervention. This ensures we meet patient expectations while also mitigating the risk of complications. Such criteria can include, but are not limited to, complaints exceeding three months, as well as a perceivable, significant impact on quality of life, often measured with the NEI-VFQ-25 questionnaire. To diminish the possibility of iatrogenic retinal breaks or detachments, we typically evaluate for the presence of an observable PVD. Additionally, any vitreoretinal pathology, such as a retinal break, is typically treated during the procedure with endolaser barrier. Core vitrectomy is implemented with preservation of the anterior hyaloid face to delay cataract formation.
We also use ultrasonography as an objective measurement to classify the state of the vitreous. Subjectively, pre-testing contrast sensitivity may have a substantial contribution to patient satisfaction and aid in determining the need for floaterectomy. Sebag’s studies show that floaters have a significant impact on contrast sensitivity, which can correlate to patient complaints and will dramatically improve following the surgical procedure.
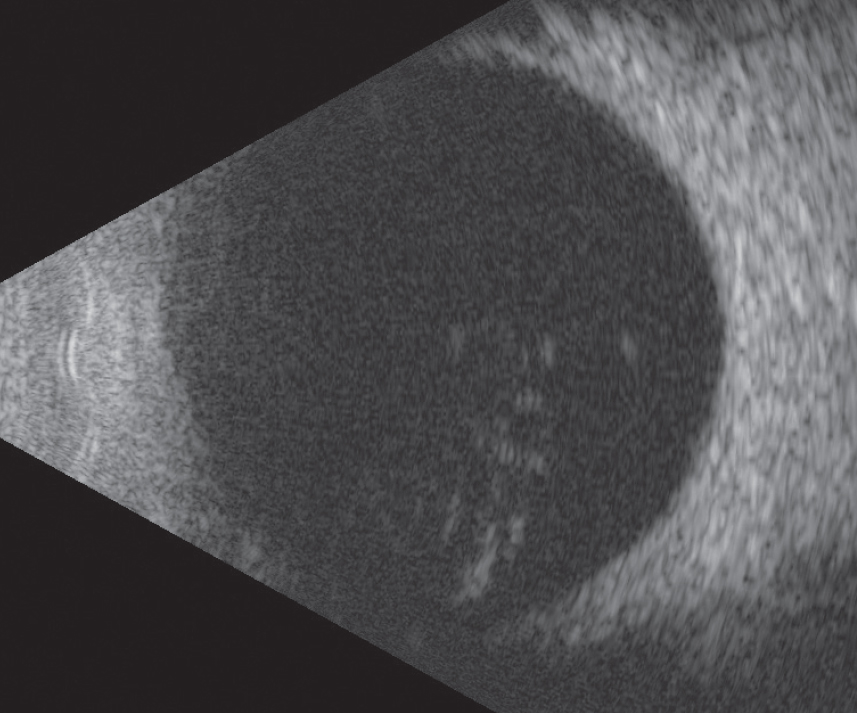 |
| An ultrasound of symptomatic vitreous floaters in a patient considering surgical management. Photo: Jay M. Haynie, OD |
Floaters Be Gone
By Drs. Shechtman and Taher
A 56-year-old white male presented to our clinic with a four-month complaint of floaters affecting his left eye more than his right. Past medical history was unremarkable. His best-corrected visual acuity was 20/20 OD and 20/25- OS. Slit lamp evaluation revealed mild cataracts in both eyes. Dilated fundus exam revealed pink, distinct optic nerves with physiological cupping. The macula was flat and intact OU, and the periphery did not reveal any pathology in either eye. The vitreous revealed syneresis OU, and a PVD was apparent in the left. Ultrasound revealed numerous floaters OU and no evidence of retinal detachments, retinal breaks or mass.
The patient was advised of the risks and benefits associated with floaterectomy, after which he opted to schedule surgery.
The patient was followed at one day and one week postoperatively, the fundus showed cleared vitreous with no peripheral pathology. Ultrasonography revealed resolution of floaters with no evidence of retinal detachments, retinal breaks or mass. The patient expressed satisfaction regarding the resolution of floaters and was asked to return to clinic within one month. He was educated on the signs and symptoms of retinal breaks and detachments and was asked to return to the clinic sooner if he noticed them.
How Our Practice Compares
By Dr. Haynie
Managing symptomatic floaters in my practice first involves differentiating acute vs. chronic symptoms. Acute symptoms secondary to a PVD will often resolve over time, and the discussion to consider surgical removal is not part of the management strategy. The priority for acute symptoms is to ensure there is no peripheral retinal breaks or holes that could be associated with a higher risk of complications such as a retinal detachment. In most cases, the vitreous floaters will settle and resolve, providing resolution of symptoms.
Management of chronic floaters—present for one year or more in my practice—can include laser vitreoloysis or vitrectomy surgery. Although laser vitreolysis has been available for two decades, my practice has yet to embrace this as a treatment for symptomatic floaters. In my area, a few anterior segment surgeons offer this treatment. Several of my patients have had laser vitreolysis and, unfortunately, continue to have symptoms; in some cases, the number of floaters increased. Of course, I likely only see those patients for whom treatment failed, not those who are satisfied with their outcomes. Some complications of vitreolysis I have seen personally include posterior capsule tears, retinal burns, foveal burns, choroidal rupture and choroidal hemorrhages. In addition, the predictability of success is highly variable. Thus, my surgeons prefer PPV as the definitive treatment for chronic floaters.
Evaluating a patient for vitrectomy surgery for symptomatic floaters first involves patient selection. This begins with a clinical examination of the vitreous to determine if a PVD has occurred. In the absence of a PVD, the surgeon will need to mechanically induce a PVD, which can increase postoperative complications or peripheral retinal breaks. We next determine the magnitude and effects of floaters. I like to look at patients with a 20D condensing lens on the visual axis to see if I can appreciate any shadows of floaters cast on the retina. If I can, then it is likely the patient will have fewer symptoms following surgery. Other ways of demonstrating the “shadow effect” are widefield red-free photography or optical coherence tomography.
Once we have determined surgery is appropriate, we provide the patient a detailed explanation of the risks, benefits and alternatives. The risks of vitrectomy surgery parallel those of cataract surgery; fortunately, the risk of any sight-threatening complication is quite low. In addition, if the patient is phakic, it is important that they understand that having vitrectomy surgery will accelerate the formation of a nuclear cataract earlier than the natural history.
One hang-up with vitrectomy for symptomatic floaters from a referring doctor’s stand-point is the risk of the surgery itself; however, the evolution of cataract surgery minimizes even this concern. Thirty years ago, when cataract surgery was associated with a higher incidence of complications, patient selection was key, and it was not indicated for everyone. Today’s cataract surgery has had major upgrades and is now the most common ocular surgery performed—and with great success in the majority of cases.
Likewise, retina surgery has also evolved. Current systems use much smaller-gauge instruments (25 or 27) compared with the 20-gauge needles used less than 15 years ago. Today’s smaller vitrectomy instruments allow for sutureless procedures, less inflammation, fewer complications and, in the end, a much greater success rate.
For each patient presenting with floaters, think about someone with cataracts and why that surgery is being done: in most cases, the patient has developed functional vision loss and secondary symptoms of glare and night driving difficulties that are impacting their quality of life. Similarly, the retina patient with symptomatic floaters also has functional vision loss with symptoms of reading difficulties, loss of contrast acuity and the burden of distraction. Vitrectomy surgery is the definitive option, and patients with symptoms greater than one year in duration deserve the opportunity to discuss surgery with a vitreoretinal surgeon.
We never think twice about referring someone for a cataract evaluation; it’s time we provide similar enthusiasm for patients looking to manage their chronic floaters.

