Comanagement is a crucial component of day-to-day optometric practice, with a significant impact on both patients and providers. However, the referral relationship can be complicated, and the best approach may not always be clear.
Comanagement ConnectionsCheck out other articles in this series: Be a Retina Referral Rock Star Keep Glaucoma Care Close to Home |
“Comanagement represents cooperation and, in the case of optometry, that means medical eye care in collaboration with our surgical counterparts—ophthalmologists,” notes Paul C. Ajamian, OD, center director of Omni Eye Services of Atlanta. “What it doesn’t mean is referring to the ophthalmologist and losing control of your patient’s care.” That instinct runs deep, though, ingrained through decades of practice in which that was just about all an OD could do.
Not any more. “We should be the general practitioners of eye care,” Dr. Ajamian argues, “and as such it is our responsibility to make the patient feel confident in the fact that they are in the hands of an expert who is going to identify and treat anything they can, and consult with a trusted specialist when something is beyond their scope.”
When comanagement is effective, the entire field will reap the benefits. “Comanagement is critical to the growth of the profession. It improves our clinical and critical thinking skills as well as our ability to deal with medical pathology,” says Aaron Bronner, OD, who practices at a large OD-MD multidisciplinary practice in the Pacific Northwest. Dr. Bronner’s practice literally bears the slogan, “Serving optometric physicians in the spirit of comanagement.” Their doctors seem to have figured out what makes these relationships tick.
To help those ODs who may still find it a struggle, this new six-part series will delve into various areas of optometric practice where comanagement is essential, beginning with cataract care. Each article will take a closer look at the referral relationship, structural challenges and knowledge gaps while offering day-to-day pearls to help ODs elevate their practice.
 |
|
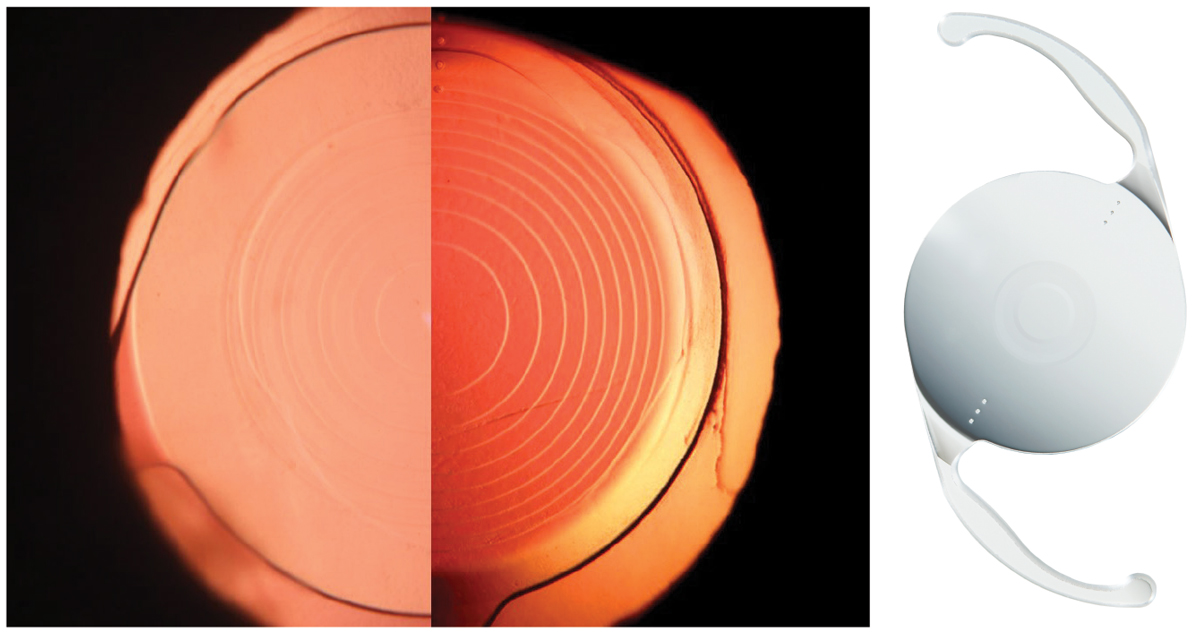
A successful comanagement relationship is one where ODs and MDs are able to rely on each other so that they’re splitting rather than duplicating the work. For instance, the optometrist should understand and be able to articulate the differences between newer IOLs to lead the patient discussion about options. Left to right: PanOptix (Alcon), Symfony (Johnson & Johnson Vision) and Vivity (Alcon) lenses. Photos: Oliver Kuh-Wilken, OD, Alcon. Click image to enlarge. |
Fostering Mutual Respect
The comanagement process is only as strong as the relationship between providers. To collaborate effectively, both parties have to recognize the unique skills each bring to the table. For an optometrist, this starts with finding skilled ophthalmologists who respect the profession and align with the practice’s clinical methods and overall philosophies of care.
The first consideration should always be patient outcomes. “Optometrists should limit their relationship building to those individuals who provide optimal results,” notes James Fanelli, OD, a private practitioner from Wilmington, NC. “Then you have to hone that down even further and identify those surgeons who not only provide good surgical outcomes, but also understand and respect the skills of an optometrist.”
It is also important to work with someone who understands your philosophy, says Dr. Fanelli. “Optometrists must convey their comanagement approach to the surgeon and ask them, ‘Are you willing to comanage cataract patients this way?’”
The services offered by an ophthalmologist should also factor into an OD’s decision. Do they offer the newer premium IOLs like trifocals or light-adjusting lenses? Is dropless cataract surgery an option at their practice? Do they perform MIGS procedures? If so, what’s their protocol for selecting prospective candidates? These are some of the questions to ask when considering a comanagement relationship, according to Paul Karpecki, OD, of Lexington, KY.
“A surgeon with a variety of tools at their disposal is a good indicator that they are dedicated to ensuring the best possible outcomes for your patients,” he says, suggesting that optometrists should make the time to shadow an ophthalmologist before referring a patient. This gives you the opportunity to gain first-hand knowledge of not only their surgical skills, but also how they treat and interact with patients. ODs should also get to know ophthalmologists outside of their practice. In a post-COVID world, this could include a lunch or dinner, Dr. Karpecki advises.
Optometrists are in the driver’s seat and have a responsibility to facilitate the best possible care for their patients. “If the right surgeon isn’t nearby, optometrists shouldn’t hesitate to refer their patients to someone further away,” says Dr. Ajamian. “Explain your reasoning to your patients and emphasize your commitment to providing optimal care. And then, take it a step further and schedule the appointment for them before they even leave your office.” That sort of hands-on approach will signal to the patient that you’re their primary eye care doctor and the surgeon, while valued and respected, is only being called in for a limited encounter.
Successful comanagement does not end when an optometrist finds a skilled ophthalmologist. It is a two-way street that requires a commitment from everyone involved. “There’s a burden on both sides to develop a strong relationship,” explains Dr. Ajamian. “Just as optometrists must get to know a surgeon and how they practice, ophthalmologists must also make the effort to get to know us and what we do.”
When comanaging, ODs should not just be content with an MD who has the courtesy to send their patient back. “A comanagement relationship is more than this and it should not be the only basis for continued referrals,” notes Dr. Fanelli. “I’m sending over patients they otherwise would not have had, and they should do the same when the opportunity presents itself.”
Dr. Fanelli offers the example of a glaucoma patient who had yet to find an optometrist. “This is a chance for the ophthalmologist to refer a patient to the OD,” he said. “That’s what it means to have mutual respect between providers. That is a two-way street and true comanagement.”
Building a robust comanagement relationship takes time and dedication. There will be a learning curve, but with continued communication, clear expectations and mutual respect, optometrists and ophthalmologists can create a collaborative environment that benefits everyone, particularly their patients.
 |
|
Patients with an epiretinal membrane may not do as well with some types of premium IOL. The comanaging OD needs to have pre-op ocular health assessment and the anticipation of visual outcomes in their skill set. Doing so will elevate the relationship from simple referral to true collaboration. Photo: Diana Shechtman, OD, Jay Haynie, OD. Click image to enlarge. |
Optimizing Cataract Care
With the number of people in the US who develop cataracts expected to double from 24 million to approximately 50 million by 2050, the need for surgical intervention will only continue to grow.1 At the same time, an impending shortage of ophthalmologists will make the role of optometrists even more critical.
“Working with cataract patients, in my opinion, is one of the pillars of medical optometric practice,” notes Dr. Bronner. “This is not something the profession can escape, nor should we try. We should lean into it and take the opportunity to be leaders in the care of these patients.”
Proper cataract care should include a good assessment, patient education, referral for surgery, and the necessary follow-up eye and vision care. Successful comanagement occurs when both the optometrist and ophthalmologist are on the same page, which can only happen with effective communication from the very beginning of the process.
Preoperative care. As with any condition, effective treatment begins with a thorough exam. In the case of cataracts, optometrists must rule out any other causes of the reduced vision as well any potential complications.
“These are all things we’re called to do every day,” notes Dr. Ajamian. “It is then our responsibility to thoroughly educate a patient on available treatments and what the best approach is for their specific case.”
While you know your patients very well, be mindful not to make assumptions. It is imperative to educate them on all options, including premium IOLs that come with a substantial out-of-pocket cost. “It is incumbent on the OD to carefully describe all lens implant options,” emphasizes Dr. Ajamian. “Patients have every reason to be upset if they find out about a potentially beneficial treatment option after the fact.”
Thorough education is also important because it strengthens your relationship with the patient and positions you as their primary resource. “If a patient receives information from the ophthalmologist instead of from their OD, it can undermine their faith in you as a provider,” warns Dr. Ajamian.
Once the optometrist has discussed the different treatment approaches with their patient and determined the best course of action, it is their responsibility to communicate this to the surgeon. Sharing as much information as possible with the surgery center sets the stage for smooth handoffs and positive outcomes.
“When a case involves more than one provider, balls can be dropped,” says Dr. Bronner. “Clear and consistent communication can help avoid this. Everyone needs to be on the same page and using similar verbiage when speaking with patients to eliminate any mixed messages.”
Oftentimes, the OD has worked with this patient for years, making them experts on not only their visual status, but also their personality and individual needs. This is why the referral letter is one of the most important components of cataract comanagement.
“I have received referral letters from ODs who have treated a patient for 30 years, and yet include only minimal details for the cataract surgeon,” Dr. Ajamian says. “Others offer a comprehensive treatment plan that outlines what has been discussed with a patient and how they want to proceed. This is very valuable for the ophthalmologist and also ensures that the optometrist is guiding the surgical process and the desired refractive outcomes.”
Postoperative care. Just as optometrists should be leaders preoperatively, they must continue guiding a patient’s care after cataract surgery. “All postoperative care can be handled by the OD,” says Dr. Fanelli, noting that there are very few cataract complications that require a return to the operating room. “As optometrists, we are the ones driving the bus, before and after cataract surgery.”
Why is it important for optometrists to take charge postoperatively? There are a number of benefits for all parties involved, according to Dr. Fanelli. “If an optometrist has a practice where they are generating revenue based on office visits and medical care, it makes sense from a fiscal perspective,” he explains. It’s also a more efficient use of everyone’s time and talents.
“Importantly, it also ensures the patient doesn’t lose their bond with the OD,” he continues. “You have been their primary eye care provider for years, and when someone they know needs a cataract referral, they will share your name rather than the surgeon’s.”
Day one post-surgery is critical, notes Dr. Karpecki. “The optometrist loses a valuable opportunity by not comanaging that early,” he warns. Post-op care contributes to the optometrist’s growth, allowing them to hone their skills and strengthen their relationship with the patient.
It’s also reassuring for patients. “On day one a patient may be anxious, and their familiar optometrist should be the one to ease their concerns,” Dr. Karpecki adds. “There is also a lot of excitement immediately following surgery and ODs should be there to celebrate that moment with their patients.”
As with any aspect of comanagement, post-op communication is a two-way street. If an optometrist observes a postoperative complication, they need to share that with the surgeon, especially if it is happening more than once, Dr. Bronner advises.
“ODs need to make the ophthalmologist aware of any issues—no matter how small—so they can minimize these complications in the future,” he elaborated. “Surgery centers also have a responsibility to tell ODs about any complications that occurred during surgery so the patients can receive the necessary care and support.”
Effective postoperative communication goes hand-in-hand with a strong relationship that recognizes the contributions and expertise of each provider. “If it is purely a referral relationship, you lose a lot of what you—and your patients—potentially could gain,” reiterates Dr. Bronner.
 |
|
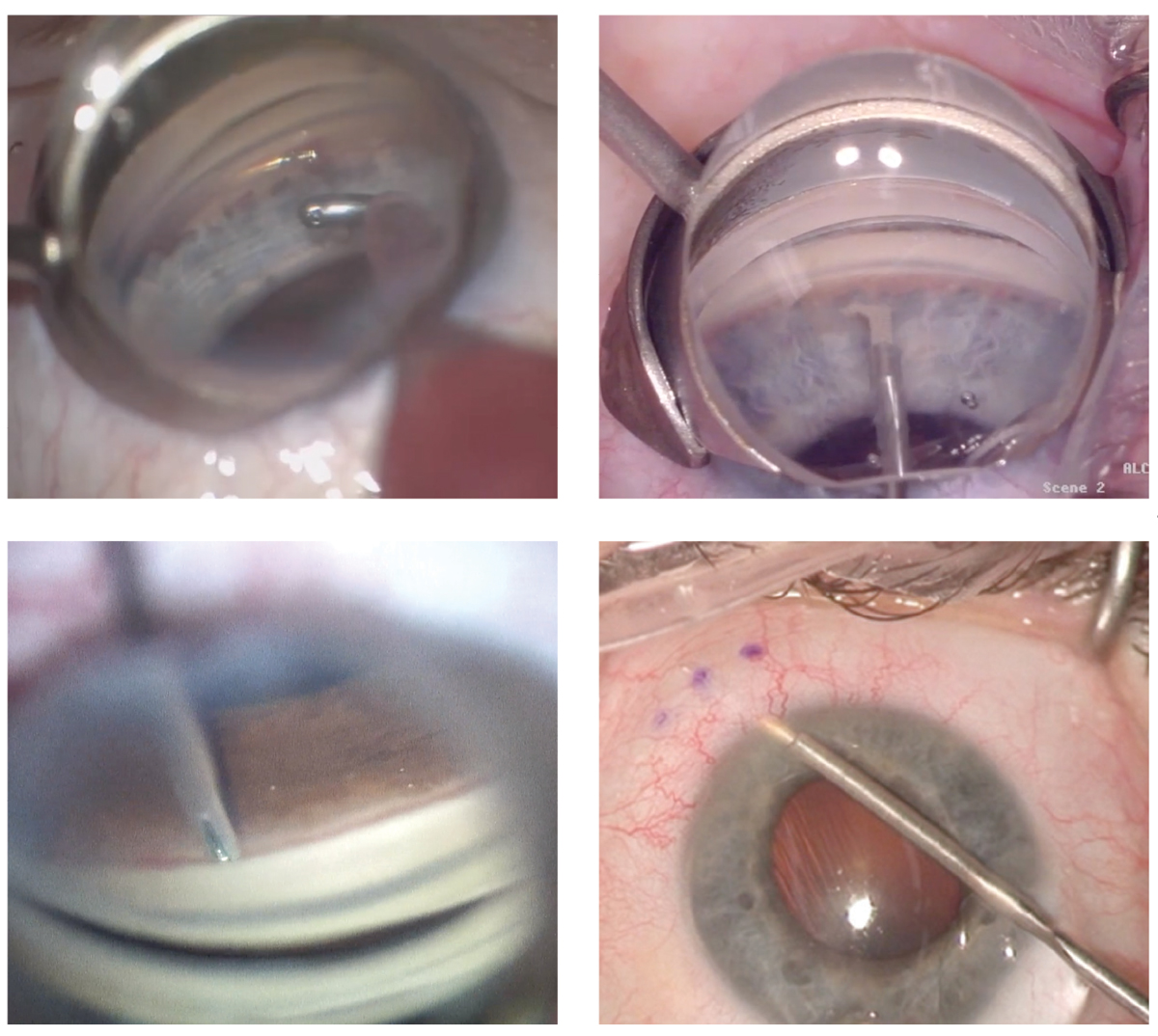
The development of minimally invasive glaucoma surgeries for use at the time of cataract surgery has increased the capabilities of surgeons—and the expectations placed on comanaging optometrists, who need to be able to sort out the many proceudres and make well-informed recommendations to the ophthalmologist. Clockwise from upper left: Hydrus Microstent (Ivantis), Kahook Dual Blade (New World Medical), Xen implant (Allergan), iStent (Glaukos). Photos: Brooke Mathie, OD, Justin Schweitzer, OD, Rachel Caywood, OD. Click image to enlarge. |
Addressing Gaps in Care
As a patient’s primary eye care provider, it is the optometrist’s responsibility to be both an educator and facilitator of treatment. While comanagement opens the door for a comprehensive, team-driven approach, ODs must take the lead and address any potential gaps in care.
An example of this in the cataract realm is the use of minimally invasive glaucoma surgery (MIGS) at the time of cataract surgery. A notable advancement in the management of glaucoma, MIGS offers an opportunity for patients to reduce their dependence on IOP-lowering medications.
In one study, four years after a MIGS procedure with the Hydrus implant on glaucoma patients taking one topical medication, over 70% of patients had IOPs low enough to remain medication free. There was a 25% to 30% advantage over patients who only had cataract surgery alone and a 65% reduction in the number of patients requiring invasive surgical procedures such as trabs and shunts.2 However, less than half of MIGS candidates actually receive these procedures, according to Dr. Karpecki.3
There are a number of factors that could contribute to the underutilization of MIGS, Dr. Karpecki notes, including a lack of awareness among providers. “As a relatively recent advance, education until now has been limited,” he explains. “Newer technologies have vastly improved patient outcomes, and it is imperative that optometrists are aware of the benefits.”
Given that MIGS procedures are not approved after cataract surgery in the US, there is only one opportunity for patients to take advantage of these procedures, emphasizes Dr. Karpecki. Optometrists must educate eligible patients on their options while also communicating effectively with the cataract surgeon.
Key Takeaways
|
“Our intake forms include a question on glaucoma; however, the comanaging doctor’s office doesn’t always include this information,” Dr. Karpecki says. “And, if a case of glaucoma is mild or missed during the exam at the surgical practice, the patient loses the opportunity for a potentially life-changing procedure.” This, he says, highlights the importance of comanagement as well as the leadership role optometrists must take in educating patients and communicating their needs to the ophthalmologist.
A deeper understanding of available procedures is important not just to ensure patients receive the care they need, but to also stop them from undergoing a treatment that isn’t right for them. “Problems arise when the optometrist does not communicate the needs of their patent to the surgeon,” notes Dr. Fanelli. “For instance, an OD should be well aware of the nuances of an individual’s glaucoma and whether or not a MIGS device is indicated. That information needs to be shared with the surgeon to ensure a patient is not given an unnecessary intervention.”
Another area where optometrists can better serve their patients is how they explain options from a refractive cataract perspective, according to Dr. Karpecki. “A lot of people come in at age 55 for LASIK and truthfully, in most cases, they’d be better served with a lens-based procedure,” he explains. “Otherwise, they’re doing a corneal procedure now and then turning around within a decade or two and having cataract surgery,” which, as a result, will be more difficult. Furthermore, a cornea-based surgery won’t help with presbyopia the way a refractive lens surgery can.
“Many times we say, ‘Let’s wait until you’re 65 and insurance covers it.’ The truth is, insurance still doesn’t cover the premium lens, so you might as well consider doing it sooner, if it is beneficial and a patient is inclined to do so,” he continues. “At the very least, having this discussion with our patients is important so we can help them make the decision that is best for them.”
An Opportunity for Growth
Comanagement is a crucial part of medicine, with benefits well beyond a single specialty. For ODs, a partnership built on mutual give-and-take helps their practice grow while providing a higher level of care.
“I believe strongly that comanagement is the most effective way to provide care, especially among the cataract population,” says Dr. Bronner. “It has been well-established that centers with higher volumes of surgery, up to a point, have a lower risk of complications and, on average, best corrected visual acuity outcomes.”
By focusing more of their time on surgery, ophthalmologists become better at this aspect of their work. Delegating non-surgical matters to optometry facilitates this growth, according to Dr. Bronner. “Sharing care with optometry, a profession that’s well-trained to take on non-surgical responsibilities, is going to make both surgeons and optometrists better at their respective roles while increasing access to care,” he concludes. “Arguments against comanagement just don’t hold water, given its many benefits.”
1. National Eye Institute. Cataract Data and Statistics. nei.nih.gov/eyedata/cataract. 2. Rhee DJ. 4-year findings from the HORIZON trial AGS 2020, Washington, DC. 3. MarketScope. Q1 Glaucoma Quarterly Update 2020. www.market-scope.com. |

