 |
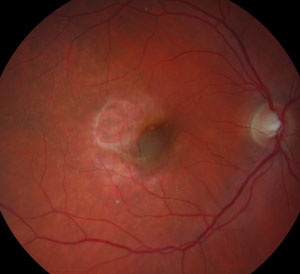
| Cadaver study finds no evidence of accelerated AMD following cataract surgery. Photo: Jay M. Haynie, OD. Click image to enlarge. |
Sunlight exposure and inflammation are both considered risk factors for age-related macular degeneration (AMD) pathogenesis, and researchers have considered whether cataract surgery—with surgically-induced inflammation and increased light exposure due to lens removal—accelerates AMD progression. A new study on human donor eyes, however, found evidence against such a relationship, suggesting that cataract surgery is safe in AMD eyes.
The researchers hypothesized, “If cataract surgery worsened AMD, human donor eyes with a history of cataract surgery would have more advanced AMD and/or more retinal pigment epithelium (RPE) mitochondrial DNA (mtDNA) damage.” The link between them is supported by a prior study that showed decreased number, size and density of RPE mitochondria.
The team obtained eyes from human donors who were at least 55 years of age and graded them for AMD severity according to the Minnesota Grading System (MGS). Each eye underwent quantitative PCR testing to obtain the frequency of mitochondrial DNA lesions in donor tissue. The researchers evaluated associations between cataract surgery and AMD severity and between cataract surgery and mitochondrial DNA lesion frequency.
The researchers included 157 subjects in the study. According to multivariable analysis with age, sex, smoking status and cataract surgery status, only age was associated with AMD grade. The researchers also noted that none of these factors was associated with RPE mitochondrial DNA lesion frequency.
“Our study results show that cataract surgery status is not a significant predictor of MGS grade in human donor eyes after adjusting for covariates including age,” the researchers explained. “Although univariable analysis showed an association between cataract surgery and more advanced AMD based on higher MGS grade in the donor eyes, age was a confounding variable. Advanced age is the strongest risk factor for AMD development and is also a well-established risk factor for cataract formation. Therefore, it is not surprising that our data analysis shows significant associations between (1) age and MGS grade as well as (2) age and bilateral cataract surgery.”
“Our study showed a lack of association between cataract surgery status and RPE mtDNA damage with both univariable and multivariable analysis,” they continued. “Our prior research found that aging in the absence of AMD was accompanied by selective mtDNA damage that was limited to the mitochondrial region known as the common deletion. In contrast, donors with AMD exhibited mtDNA damage in all regions of the mitochondrial genome. Therefore, even though cataract is associated with aging, extensive RPE mtDNA damage does not occur with aging alone, unless associated with advanced AMD. Similarly, we can assume that changes after cataract surgery would not be associated with increased RPE mtDNA damage unless also associated with more advanced AMD.”
The researchers concluded that because their donor eye mitochondrial DNA analysis included all regions of the mtDNA genome, the fact that the bilateral cataract surgery and no cataract surgery groups had similar levels of mtDNA damage suggests cataract surgery doesn’t accelerate AMD progression.
Armbust KR, Karunadharma PP, Terluk MR, et al. No association between cataract surgery and mitochondrial DNA damage with age-related macular degeneration and human donor eyes. PLoS One. October 19, 2021. [Epub ahead of print]. |

