Several presentations at this years Association for Research in Vision and Ophthalmology (ARVO) meeting discuss the efficacy and safety of drugs that target vascular endothelial growth factor (VEGF) in patients who have age-related macular degeneration (AMD). Other research looked at the accuracy of imaging technologies and the effects of diet on the vision of AMD patients.
Anti-VEGF Treatments For AMD
Researchers are evaluating several anti-VEGF treatments for AMD patients. VEGF, a protein, is believed to be one of the main mediators of choroidal neovascularization (CNV) in AMD patients.
Macugen (pegaptanib sodium injection, Eyetech/Pfizer) is the only drug currently FDA approved to treat wet AMD. Some retinal specialists also currently use Avastin (bevacizumab, Genentech) off-label to treat wet AMD. The drug is FDA approved, but for the treatment of metastatic colorectal cancer. Lucentis (ranibizumab, Genentech), a drug derived from Avastin, is not yet FDA approved but is being studied. The following studies evaluated the efficacy of these drugs:
 |
 |
|
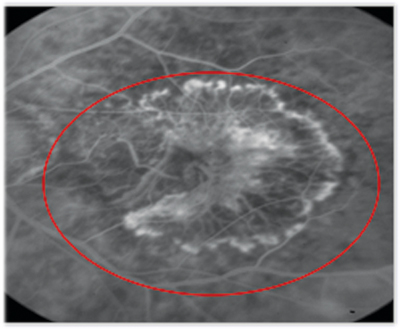
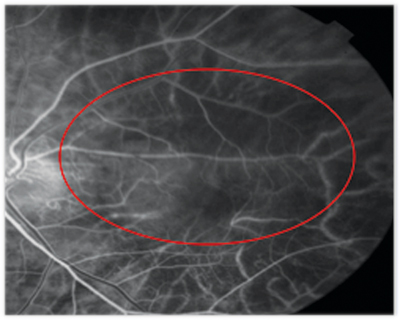
In this patient, who was treated with Macugen, the total lesion size and leak intensity decreased at week 54 (right) compared with baseline (left). |
Avastin. Researchers in Santa Barbara, Calif., examined 81 eyes (79 patients) with subfoveal neovascular AMD that received intravitreal Avastin monthly until macular edema, subretinal fluid and pigment epithelial detachments resolved.3540 Ophthalmic evaluations included non-standardized Snellen visual acuity, complete ophthalmic examination, fluorescein angiography and optical coherence tomography (OCT).
The researchers found that Avastin is well-tolerated and is associated with improved visual acuity, decreased retinal thickness and reduction in angiographic leakage in most patients, many of whom were previously treated with PDT and/or Macugen.
Lucentis. The MARINA (i.e., minimally classic/occult trial of the anti-VEGF antibody ranibizumab [formerly RhuFab] in the treatment of neovascular AMD) study is a phase III multicenter, randomized study of the efficacy and safety of monthly intravitreal injections of Lucentis in patients who have minimally classic or occult CNV secondary to AMD.2959 Researchers for the double-masked study randomized 716 patients to receive 0.5mg of Lucentis, 0.3mg of Lucentis or a sham injection monthly for two years. One-year data showed that nearly 95% of patients who received 0.3mg or 0.5mg of Lucentis lost less than 15 letters of visual acuity vs. 62% of sham-injected patients. Of the 716 patients, 683 have started the second year of the study.
Imaging
Studies at this years meeting confirmed the accuracy of imaging equipment used to detect and monitor AMD.
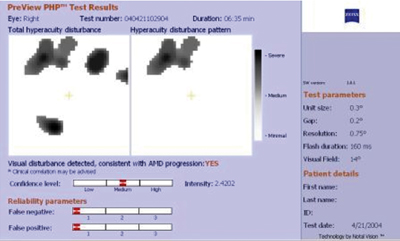
One study assessed the sensitivity of the PreView Preferential Hyperacuity Perimeter (PHP) vs. retinal specialists in grading stereo color photographs to detect CNV based on lesion size and location and a patients visual acuity.5708 Researchers found that:
Among patients whose visual acuity was 20/40 or better, the PHP detected 60% of CNV cases, while the retinal specialists detected about 53%.
Among the patients whose lesion size was 2DA (disc area) or smaller, the PHP detected 81% of CNV cases, and the retinal specialists detected 59%.
Among patients whose lesion size was 4DA or smaller, the PHP detected 77% of CNV cases vs. the retinal specialists, who detected 64%.
Among patients who had nonfoveal CNV, the PHP had a sensitivity of 81% vs. 62% for retinal specialist grading.
Among patients whose visual acuity was 20/80 or better and whose lesions were 4DA or smaller and located outside the fovea, the PHP had a sensitivity of 81%. Grading by the retinal specialists had a 62% sensitivity.
The researchers concluded that PHP is at least as good as retinal specialists grading of stereo color photographs in detecting early-onset CNV, particularly when CNV is small, nonfoveal and associated with relatively good visual acuity.
 |
|
This PreView PHP image shows that the patient has a choroidal neovascular membrane. |
Researchers from Colorado found that primary-care physicians can be trained to read fundus images from a non-mydriatic camera.330 Sixteen primary-care physicians received training on basic retinal anatomy and physiology related to diabetic retinopathy. Next, 1,227 patients with diabetes were seen by the primary-care physicians and a retinal specialist. They took one 45-degree photo centered on the fovea through an undilated pupil. The referral rate for diabetic retinopathy by the primary care physicians was 10.8% vs. 10.2% by the retinal specialists. Primary-care physicians detected diabetic retinopathy with about 74% sensitivity and 96% specificity compared to retinal specialists, who were considered the gold standard. The researchers concluded that training primary-care physicians to screen for diabetic retinopathy may be viable with continued training and improved imaging with digital technology and mydriasis.
Diet
Researchers from the National Eye Institute and Harvard Medical School found that patients who have AMD and consumed high amounts of docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) were 20% and 25%, respectively, less likely to progress to vision loss, even after controlling for AMD status and baseline and follow-up lens opacity.2193 They also found that the likelihood of vision loss was greater among patients who reported the highest monosaturated fatty acid intake. They did not find any significant associations with saturated fat intake, total cholesterol, arachidonic acid, linoleic acid or a-linolenic acid.
Their findings are based on an eight-year, multicenter follow-up study of 2,381 participants in the Age-Related Eye Disease Study (AREDS). The participants had early or intermediate AMD in at least one eye at enrollment, best visual acuity of 20/32 or better in both eyes and no history of cataract extraction. The researchers estimated baseline lipid intake with a validated food frequency questionnaire; determined demographic, lifestyle, medical and ocular data from standardized questionnaires; and obtained AMD and cataract information through annual fundus and lens photographs.
Dr. Dunbar is director of optometric services at Bascom Palmer Eye Institute in Miami, and author of Review of Optometrys Retina Quiz column.
330. Mandava N, Prall R, Carsky C, Parnes B, Farley T. Screening for diabetic retinopathy in primary care using a non-mydriatic camera.
367. Li C, Peracha M, Gao H. Comparison of pegaptanib (Macugen) and photodynamic therapy with verteporfin combined with intravitreal triamicinolone (PDT + TAC) as treatment for subfoveal choroidal neovascularization due to age-related macular degeneration.
2193. SanGiovanni JP, Chew EY, Agron E, et al. Dietary lipid intake and vision loss in the Age-Related Eye Disease Study.
2959. Heier JS, Shapiro H, Singh AA, MARINA Study Group. Randomized, controlled phase III study of ranibizumab (Lucentis) for minimally classic or occult neovascular age-related macular degeneration: two-year efficacy results of the MARINA study.
3540. Pieramici D, Avery R, Rabena MD, et al. Bevacizumab (Avastin) in the treatment of neovascular age-related macular degeneration.
5708. Goldstein M, PHP study group. Sub-analysis comparison between the sensitivity of the PreView PHP and retinal specialists grading of stereo color photographs in detecting recent onset CNV.
5729. Mizota A, Sakuma T, Miyauchi O, et al. Measurement of retinal thickness from three-dimensional image obtained from OCT ophthalmoscopic images.

