 |
Refinement of our conception of tear film structure has taken us from seeing mucins as a standalone layer to an integral part of the mucoaqueous matrix.1 Mucins contribute very little to the thickness of the tear film, but their role is much greater than their share of ocular real estate implies. Mucins are vital to ocular surface protection and stability.2,3
Consider this: without mucins, the tear film could not readily adhere to the eye.2,3 As such, it’s no wonder that mucin-deficient dry eye can be so insidious. However, this seemingly rare form of dry eye disease (DED) may be more frequent than we assume. In fact, mucin dysfunction is now said to be common in all forms of moderate to severe DED, which has prompted interest in more thoughtful diagnosis and inspired new research on treatment aimed at fortifying this important structure.4
Mucins Explained
Understanding what stimulates mucin secretions and how to regulate it is an area rich in research potential. Mucins are produced throughout the body, but ocular surface mucins in particular are generated by goblet cells—apical cells of the conjunctiva and cornea and the lacrimal gland.4 Meibomian gland secretions also contribute to the mucin content found on the tear film.1 Mucins are high-molecular weight glycoproteins that contribute to the mucus layer, promoting cell adhesion and defending against ocular surface damage.2,3,5
 |
|
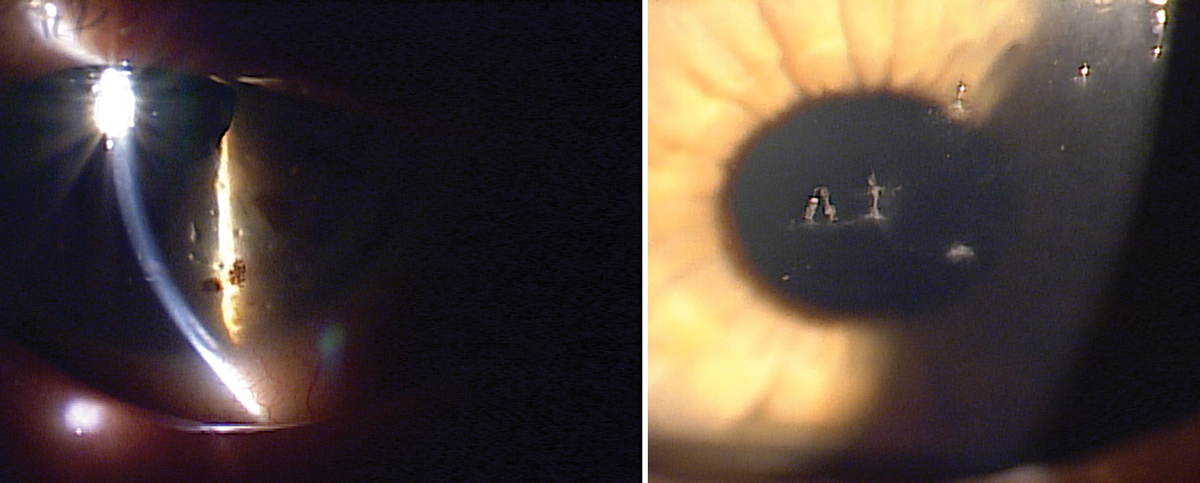
Filamentary keratitis with mucin and epithelial cells adhering to the corneal surface. Click image to enlarge. |
Mucus, on the other hand, is a lubricant that prevents desiccation of the ocular surface during blinking by dissipating energy.1 Mucus gel also traps bacteria and irritants so that they can be removed during blinking.1 Furthermore, mucins help stabilize the tear film and help maintain hydration.6
Some mucins are membrane-bound to epithelial cells, while others are secreted diffusely throughout the tear layers.4 MUC5AC and MUC2 are secreted mucins whereas MUC1, MUC4 and MUC16 are membrane-bound.4 Importantly, both forms contribute to ocular surface health in different ways.4 For example, MUC5AC is a gel-forming mucin that traps allergens and pathogens.7 MUC2 and MUC5AC are gel-forming mucins that affect how much water can be retained in the tear film.1
Diagnosing Dysfunction
It is well-established that dry eye can occur in response to decreased mucin levels. Goblet cell loss is a common feature of every form of DED.8 Relatedly, when goblet cell density decreases, MUC5AC production also decreases and disease severity increases.8 Although some studies have shown the expression of the MUC5AC gene doesn’t change depending on DED status, MUC5AC levels appear in lower concentrations in the tears of patients with DED.9 Interestingly, evidence suggests that mucin deficiency is both a cause and a consequence of DED.4 Specifically, goblet cell loss is related to inflammation subsequent to hyperosmolarity, yet mucus deficiency also has been shown to sustain hyperosmolarity and inflammation.10
Although there is no conclusive marker for mucin-deficient dry eye, several tests can help us tease out the extent to which mucins are responsible for each patient’s unique presentation. These include ocular surface staining, particularly conjunctival staining, fluorescein corneal staining for mucin plaques and filaments, impression cytology, laser scanning confocal microscopy and tear film instability measurements.4
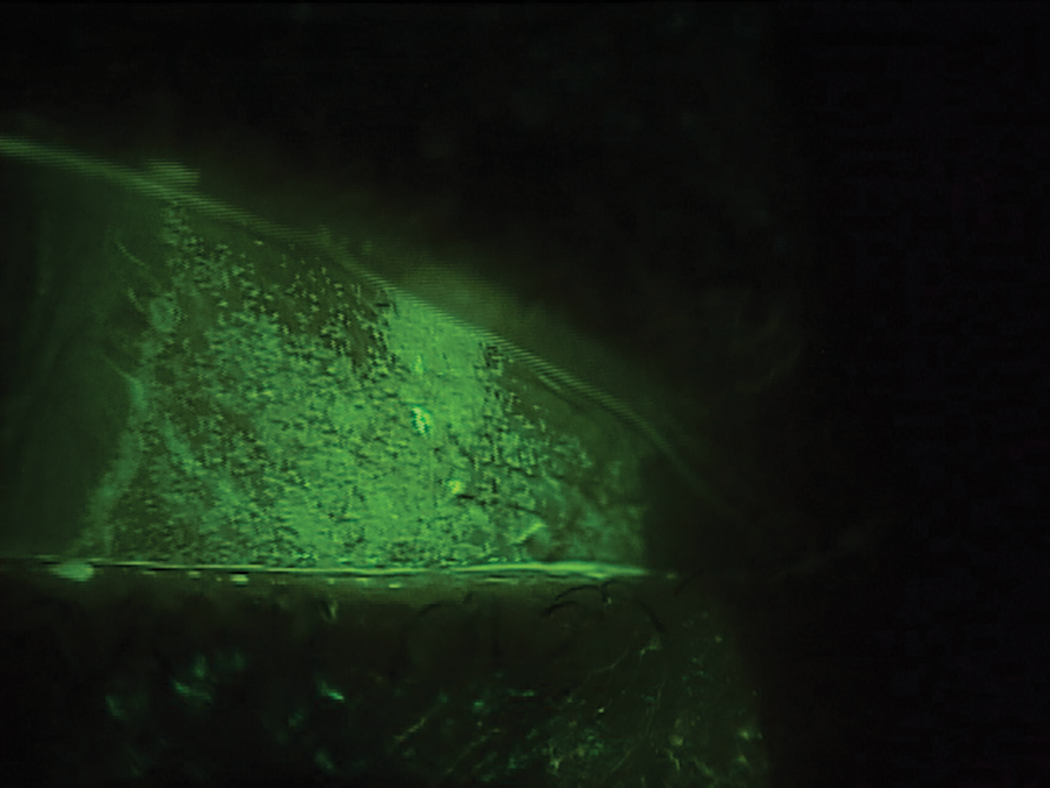
Specifically, the use of rose bengal can demonstrate reduced goblet cell density and epithelial cell mucin expression. However, due to discomfort and phototoxicity, rose bengal is not used as frequently as the nontoxic vital dye lissamine green, which can detect dead and degenerated cells.4
For ocular staining assessments that extend beyond the conjunctiva, fluorescein sodium is most suitable, as it allows for corneal examination.4 Note that staining both structures is preferred to obtain a comprehensive clinical picture. For instance, without conjunctival staining, mucus fishing syndrome would be difficult to diagnose. Although dyes can be used to assess tear film instability, interferometry and topography allow for quantifiable non-invasive measurement.
Keep in mind that inflammation and mucin expression are closely linked. In fact, inflammatory mediators act directly on goblet cells, modulating proliferation, differentiation, apoptosis and function.4 Furthermore, neurogenic inflammation is connected to mucin dysfunction, owing to the fact that goblet cell secretion is stimulated via a reflex arc from the afferent sensory nerves in the cornea to the efferent sympathetic and/or parasympathetic nerves of the conjunctiva.4 Importantly, nerve growth factor can stimulate mucin secretion and has been shown in animal studies to increase goblet cell numbers.11,12
Other inflammatory diseases associated with mucin dysfunction include filamentary keratitis, superior limbic keratoconjunctivitis and mucus fishing syndrome.
Treating Dysfunction
Several agents have been proposed as potential treatments to restore mucin function.4 For example, viscoelastic gel lubricant drops containing hyaluronic acid, carbomers and HP-guar are said to be “mucin-like” in function.4 In addition, recombinant human lubricin was shown to reduce signs and symptoms in patients with moderate dry eye.13
 |
|
Staining of the conjunctiva in a mucin-deficient dry eye. Click image to enlarge. |
Three mucin secretagogues (diquafosol tetrasodium, rebamipide and vitamin A) are also potential treatments.4 Diquafosol tetrasodium facilitates mucin production and tear secretion and is currently approved as an ophthalmic solution at 3% concentration outside the United States.4 The quinolone derivative rebamipide is also under investigation due to its anti-inflammatory and antioxidant properties.4
Both oral and topical vitamin A have been investigated as treatments.14 Vitamin A ointment for DED recently became available in the US as Optase Hylo Night and is a practical and important option doctors can use and implement right away. Using vitamin A supplementation is also logical, considering that deficiency is linked to goblet cell loss.4
In terms of anti-inflammatories, studies of approved agents frequently address issues relating to goblet cell function as well as clinical signs consistent with mucin deficiency or expression. As discussed above, nerve growth factor is also an area of current investigation.
In addition to treatments aimed at restoring function, mucolytics can decrease mucus discharge.4 Specifically, topical 5% N-acetylcysteine (NAC) has mucolytic, anti-inflammatory and antioxidant properties, and regulates mucus secretion while reducing mucus accumulation in the conjunctival sac in dry eye patients.4 Studies demonstrate that NAC reduces symptoms these patients, as well as improves signs and symptoms in MGD patients and improves TBUT and mucus ferning patterns in blepharitis patients.15-18 Oral mucolytics may also be considered, although these may further disturb the tear film.4
On Closer Inspection
Changes in mucins are not only present in advanced disease; rather, this can be the very first signal that a patient has ocular surface disease.4 Furthermore, although historically mucin deficiency was thought to be a rare cause of DED, renewed attention highlights the need for more careful examination during the diagnostic process.4 With newer treatments demonstrating targeted effects, the imperative to conduct more thorough investigations is pronounced.4
Dr. Karpecki is medical director for Keplr Vision and the Dry Eye Institutes of Kentucky and Indiana. He is the Chief Clinical Editor for Review of Optometry and chairman of the affiliated New Technologies & Treatments conferences. A fixture in optometric clinical education, he provides consulting services to a wide array of ophthalmic clients. Dr. Karpecki’s full disclosure list can be found here.
| 1. Portal C, Gouyer V, Gottrand F, Desseyn JL. Ocular mucins in dry eye disease. Exp Eye Res. 2019;186:107724. 2. Gibson IK, Kunert KS, Argueso P. Regulation of mucin gene expression in the ocular surface epithelia. Cornea 2000;19:6:S97. 3. Rolando M, Zierhut M. The ocular surface and tear film and their dysfunction in dry eye disease. Surv Ophthalmol. 2001;45(45 Suppl 2):S203-10. 4. Baudouin C, Rolando M, Benitez Del Castillo JM, et al. Reconsidering the central role of mucins in dry eye and ocular surface diseases. Prog Retin Eye Res. 2019;71:68-87. 5. Watanabe H. Significance of mucin on the ocular surface. Cornea 2002;21(2 Suppl 1):S17-22. 6. Willcox MDP, Argüeso, P, Georgiev, GA, et al. TFOS DEWS II Tear Film Report. Ocul Surf. 2017;15(3):366-403. 7. Ablamowicz AF, Nichols JJ. Ocular surface membrane-associated mucins. Ocul Surf. 2016;14(3)331-41. 8. Bron, AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report. Ocul Surf. 2017;15(3):438-510. 9. Uchino Y, Uchino M, Yokoi N, et al. Alteration of tear mucin 5AC in office workers using visual display terminals: The Osaka study. JAMA Ophthalmol. 2014;132(8):985-92. 10. Baudouin C, Irkeç M, Messmer, EM, et al. Clinical impact of inflammation in dry eye disease: proceedings of the ODISSEY group meeting. Acta Ophthalmol. 2018; 96(2):111-9. 11. Ríos JD, Ghinelli E, Gu J, et al. Role of neurotrophins and neurotrophin receptors in rat conjunctival goblet cell secretion and proliferation. Invest Ophthalmol Vis Sci. 2007;48(4):1543-51. 12. Coassin M, Lambiase A, Costa N, et al. Efficacy of topical nerve growth factor treatment in dogs affected by dry eye. Graefes Arch Clin Exp Ophthalmol. 2005;243(2):151-5. 13. Lambiase A, Sullivan BD, Schmidt TA, et al. A two-week, randomized, double-masked study to evaluate safety and efficacy of lubricin (150 μg/mL) eye drops versus sodium hyaluronate (HA) 0.18% eye drops (Vismed) in patients with moderate dry eye disease. Ocul Surf. 2017;15,(1)77-87. 14. Alanazi SA, El-Hiti GA, Al-Baloud AA, et al. Effects of short-term oral vitamin A supplementation on the ocular tear film in patients with dry eye. Clin Ophthalmol. 2019;13:599-604. 15. Pokupec R, Petricek I, Sikić J, et al. Comparison of local acetylcysteine and artificial tears in the management of dry eye syndrome. Acta Med Croatica. 2005;59(4):337-40. 16. Akyol-Salman I, Azizi S, Mumcu U, Baykal O. Efficacy of topical N-acetylcysteine in the treatment of meibomian gland dysfunction. J Ocul Pharmacol Therapeut. 2010;26(4):329-33. 17. Akyol-Salman I, Azizi S, Mumcu UY, et al. Comparison of the efficacy of topical N-acetylcysteine and a topical antibiotic combination therapy in the treatment of meibomian gland dysfunction. J Ocul Pharmacol Therapeut. 2012;28,(1):49-52. 18. Yalçin E, Altin F, Cinhüseyinoglue F, Arslan MO. N-acetylcysteine in chronic blepharitis. Cornea. 2002;21(2):164-8. |

