Retinal holes and tears are commonly encountered during dilated fundus examination of both symptomatic and asymptomatic patients. Retinal defects come in different shapes and sizes and may be either partial or full thickness. Their causes are equally varied.
What follows is a pictorial, instructive guide depicting and describing various types of retinal holes and tears, their possible etiologies and management strategies.
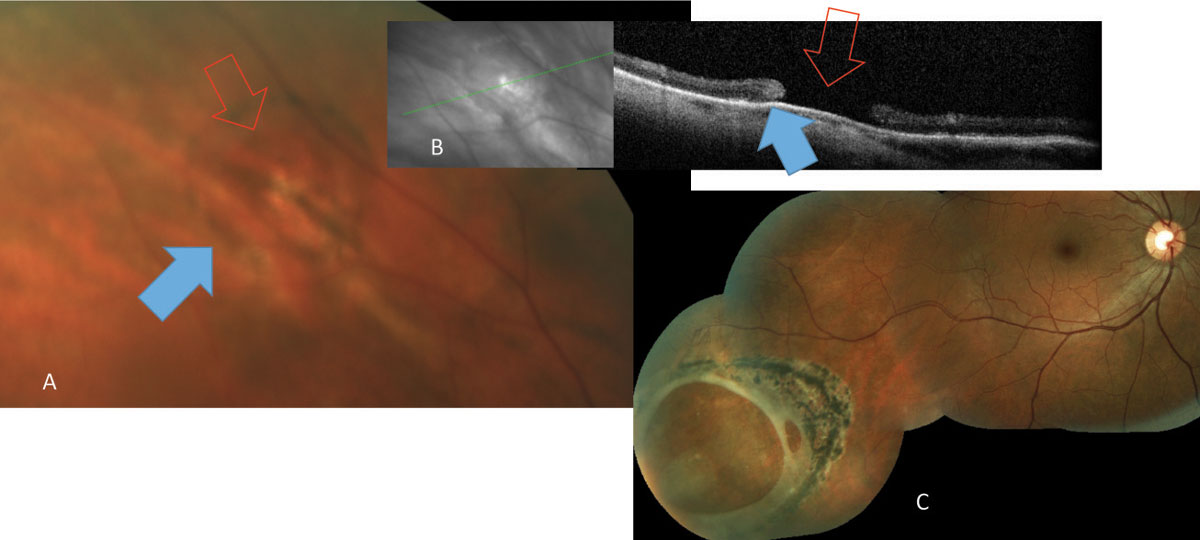 |
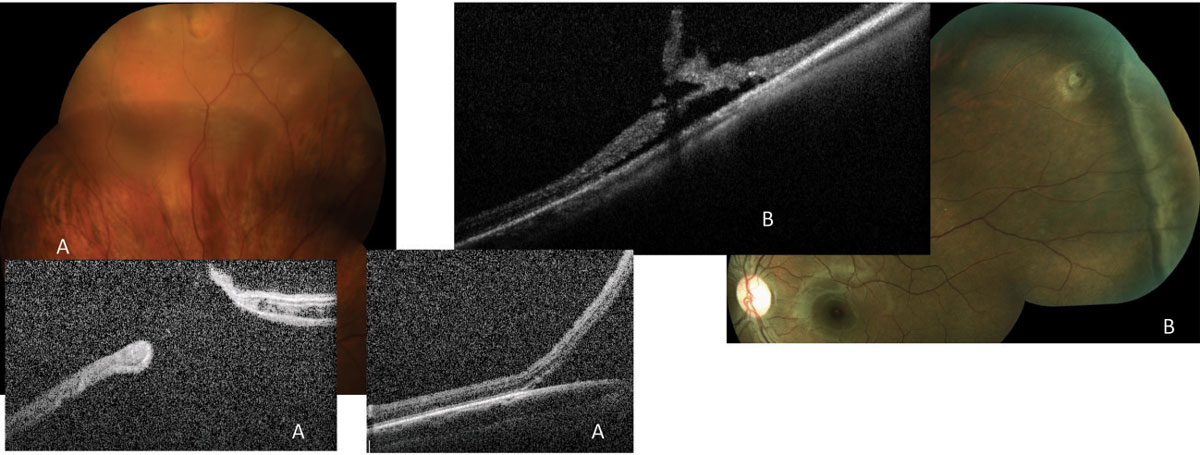
| Fig. 1. Atrophic retinal hole (red arrows) noted both on (A) fundus photograph and (B) OCT. The ring of pigmentation (blue arrows) is a reactive repair due to separation of neurosensory retina and the retinal pigment epithelium. (C) A large atrophic hole noted in routine examination and subsequently treated with laser. Click image to enlarge. |
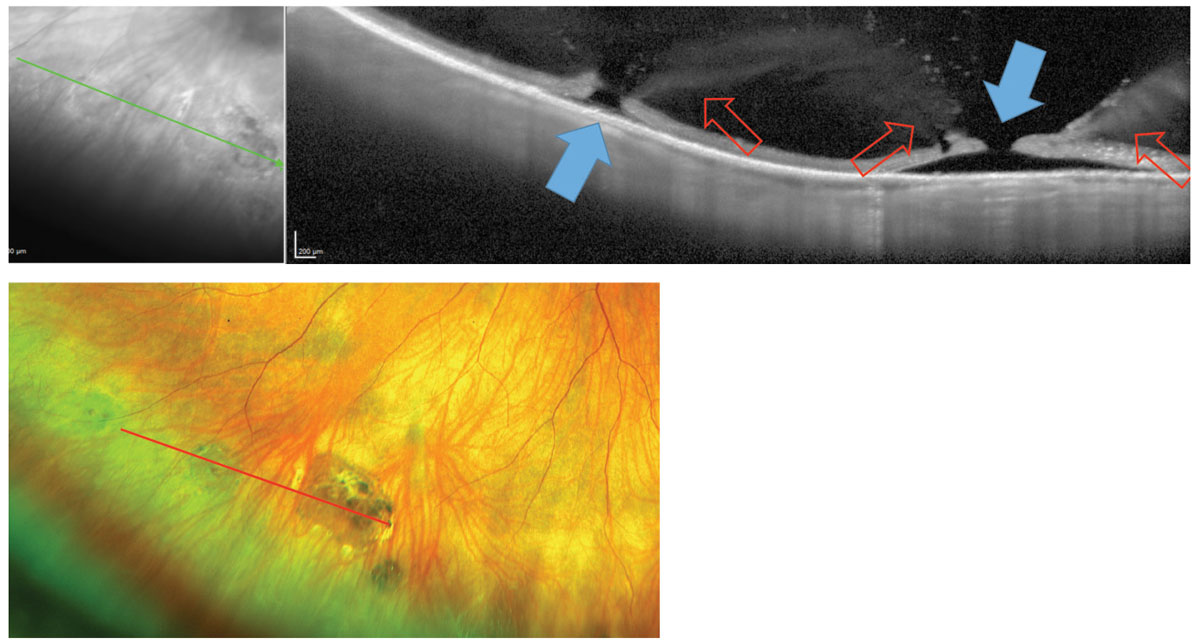 |
| Fig. 2. The above images display atrophic retinal holes (blue arrows) with surrounding regions of vitreoretinal adhesion (red arrows) visible in the images above and below. Click image to enlarge. |
Atrophic Retinal Holes
These are most often found during routine exam of the peripheral retina (Figure 1). Most patients exhibiting these have no associated symptoms. While atrophic holes occur secondary to focal degeneration of the neurosensory retina and are not resultant from vitreous traction, they can exhibit surrounding areas of abnormal vitreoretinal adhesion (Figure 2).1,2 Often, these holes are contained within, or are adjacent to, lattice degeneration and may be partial or full thickness (Figures 3 and 4).1,2
 |
| Fig. 3. Lattice degeneration with multiple retinal holes. OCT shows a full-thickness break (blue arrow) and surrounding sub-and intraretinal fluid (red arrow) in the so called “cuff of fluid.” The progression of this fluid can lead to a chronically progressive rhegmatogenous retinal detachment. Click image to enlarge. |
 |
| Fig. 4. The small crevices (blue arrow) noted within patches of lattice usually represent a partial excavation of the neurosensory retina. As these can be considered “partial-thickness holes,” there is no threat for chronic flux of fluid to the subretinal space. Careful examination and scleral depression is needed to distinguish between full-thickness and partial-thickness retinal holes, as their management can vary. OCT can help make the distinction. Click image to enlarge. |
There is no clear consensus for management of atrophic retinal holes; therefore, many practitioners elect to monitor.3-5 However, a full-thickness retinal hole can allow transmission of fluid from the vitreous cavity to the subretinal space and may result in subretinal fluid accumulation and a rhegmatogenous retinal detachment (RRD).5
Often, atrophic round holes lead to slow-growing chronic detachments (Figure 5).6 RRDs located in the inferior or temporal retinal quadrants, or both, are often found in completely asymptomatic patients not aware of superior or nasal field loss.5
Laser prophylaxis of atrophic holes may reduce the risk of retinal detachment and carries minimal to no risk (Figure 6).3-5
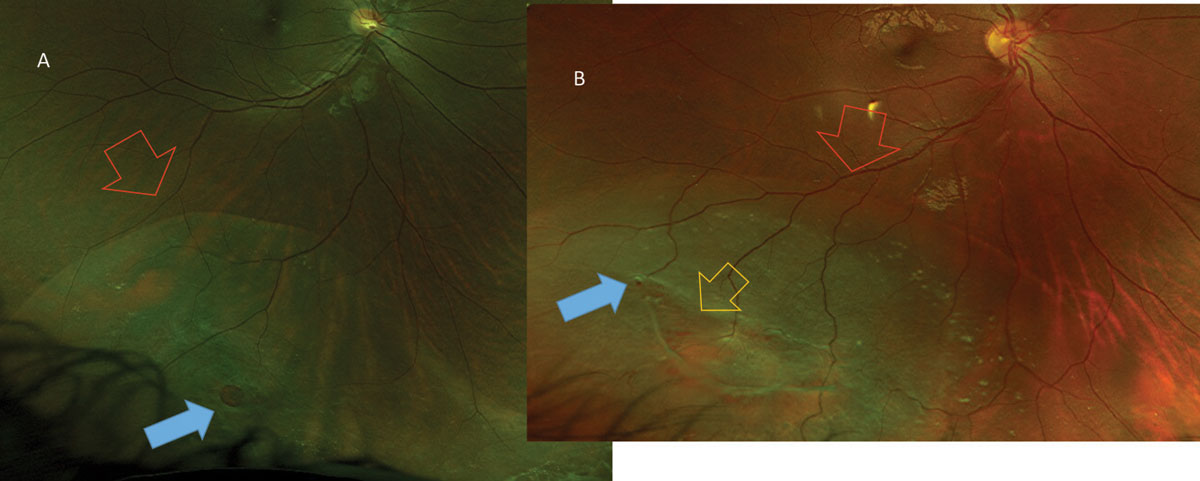 |
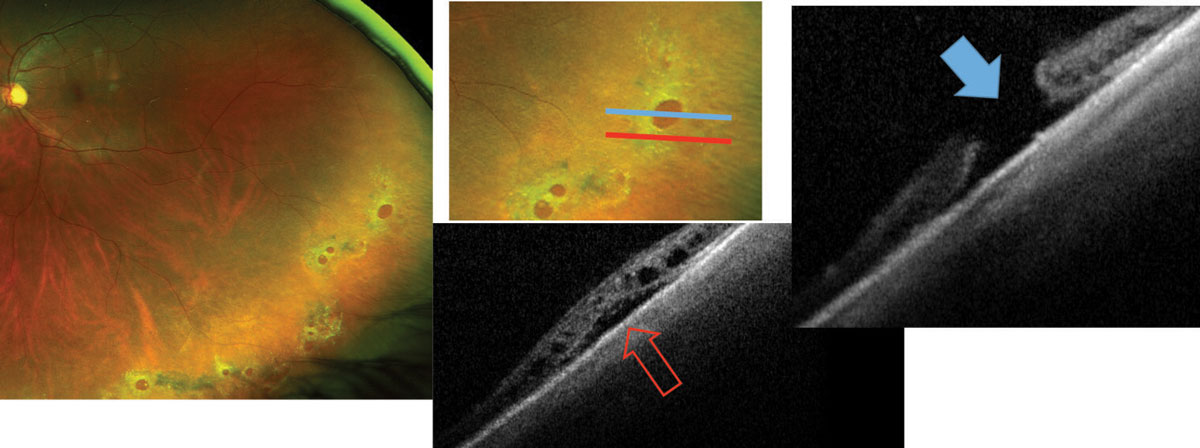
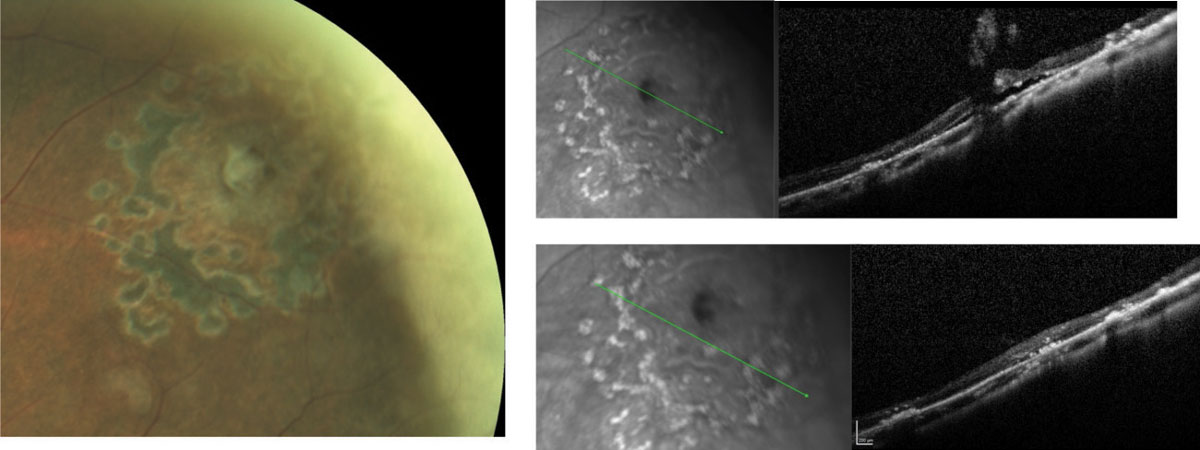
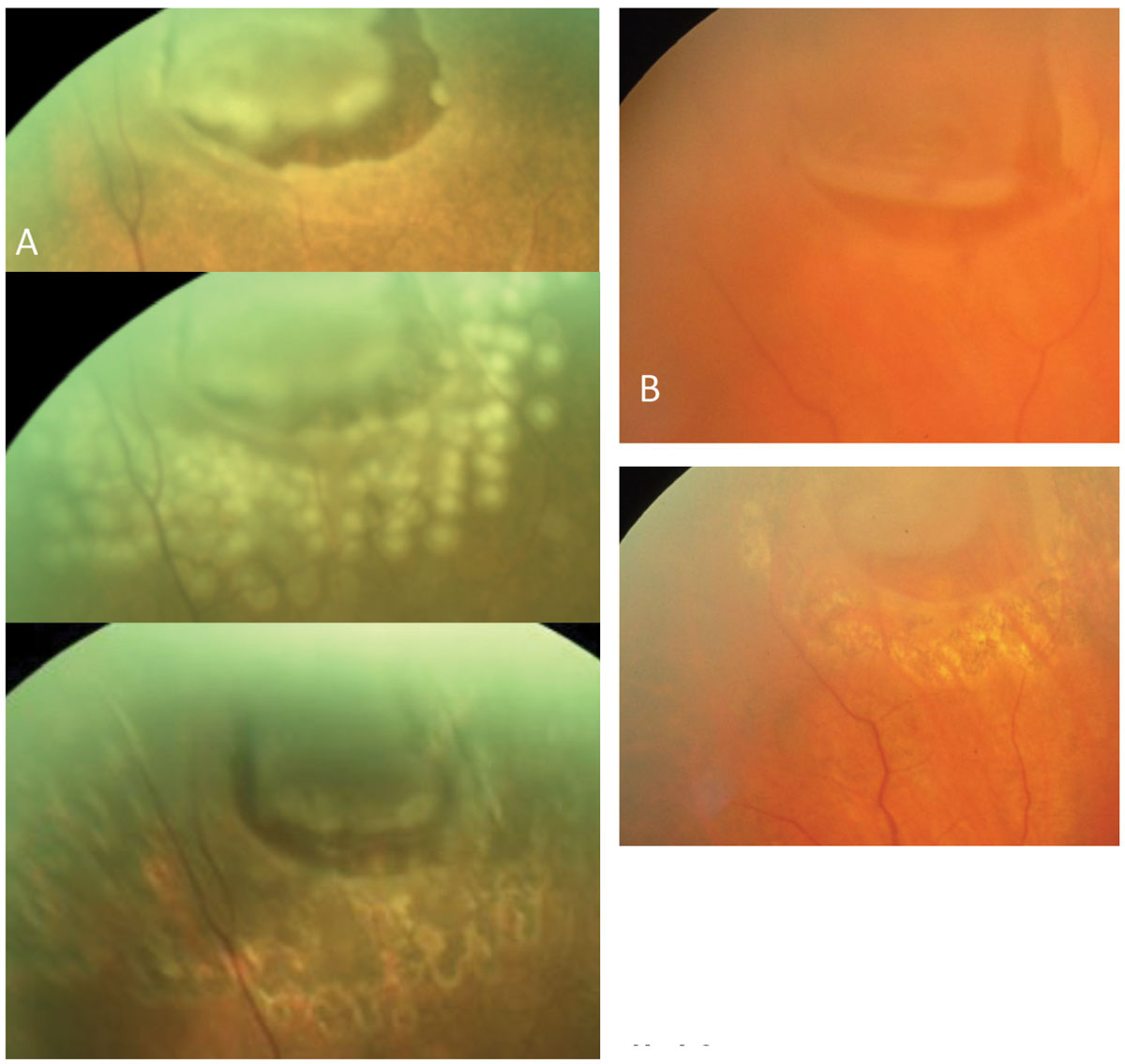
| Fig. 5. Chronic inferotemporal retinal detachments (red arrows) noted in these asymptomatic patients. In one patient (A) the atrophic hole (blue arrows) is an isolated finding, whereas in a different patient (B) the atrophic hole (blue arrow) is associated with lattice degeneration (yellow arrow). |
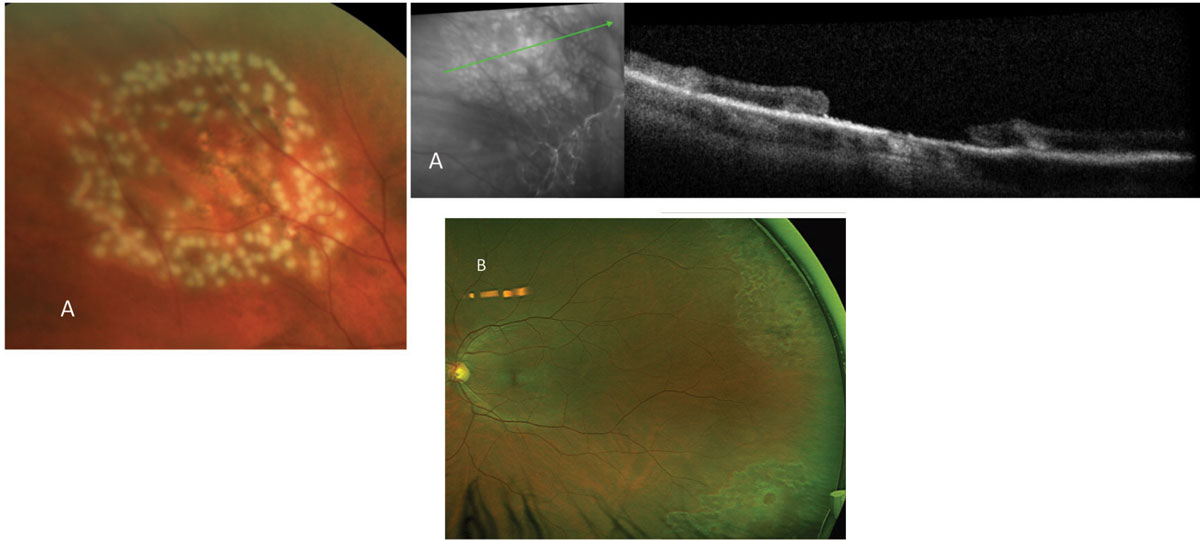 |
Fig. 6. Laser prophylaxis is noted around a single atrophic hole (previously noted in Figure 1A) and multiple holes (noted in Figure 3B). Here, in (A), you can see blanching of the laser immediately after application, while in (B) a typical hyperpigmentation is noted with time. Click image to enlarge. |
Operculated Retinal Holes
Unlike atrophic holes, operculated holes usually originate in focal areas of vitreoretinal abnormalities. Their predecessors may be defined as retinal tufts or any other pathology causing either an excessively strong vitreous adhesion or especially weak retinal structure. A formative event may then be precipitated by trauma or a natural release of vitreous traction resulting in a full-thickness hole and an overlying retinal operculum.7,8
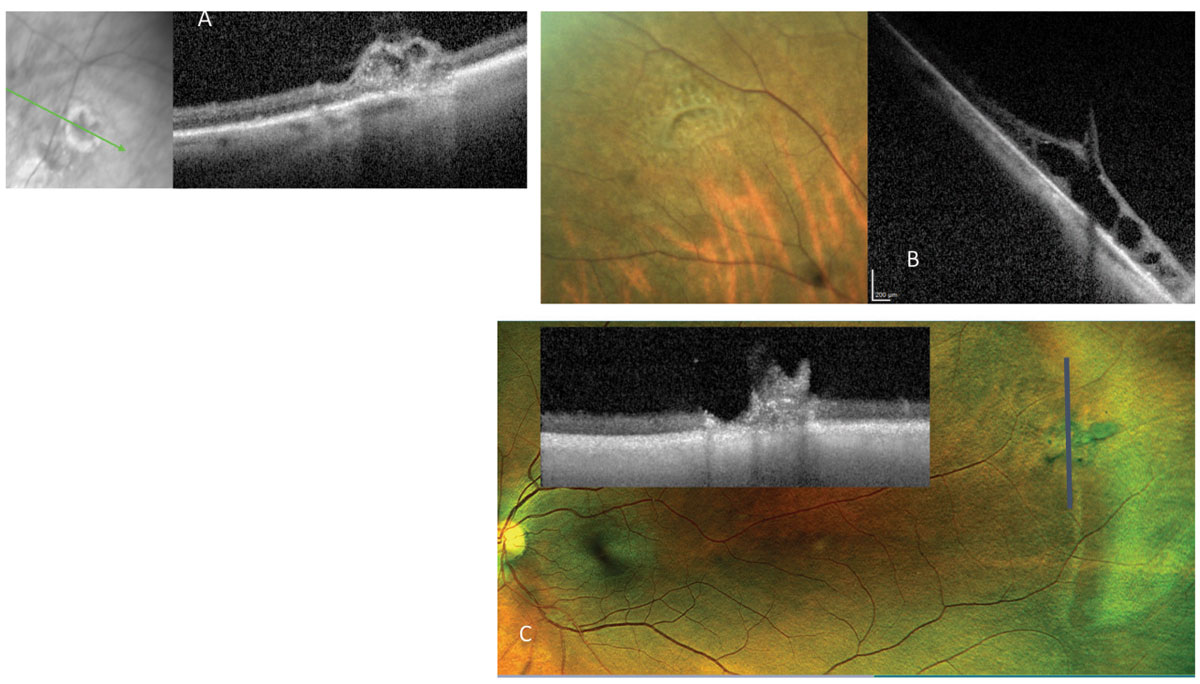 |
| Fig. 7. Vitreous tufts are congenital vitreoretinal developmental anomalies. They can present as (A) non-cystic tuft, (B) cystic tufts or (C) tufts with an adjacent partial-thickness hole, seen here on fundus and OCT images. Click image to enlarge. |
 |
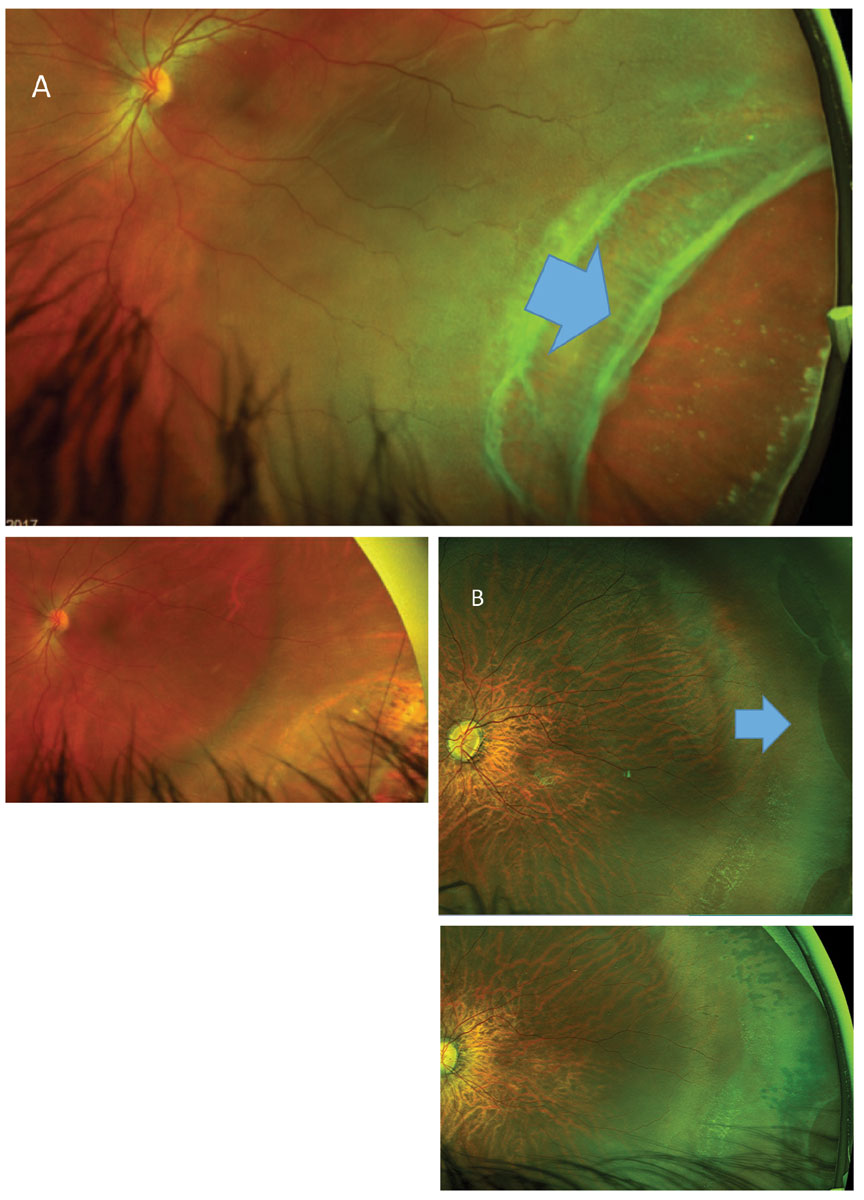
| Fig. 8. These images show examples of round operculated holes. In (A) the patient’s operculum remains attached to the edge of the retinal hole. On OCT the cuff of fluid is noted surrounding the hole. In a different patient (B), although the operculum is released in the vitreous cavity (blue arrow), the edge of the retinal hole is lifted, allowing fluid to access the subretinal space (blue circle). Click image to enlarge. |
Vitreous tufts are congenital vitreoretinal developmental anomalies. These have cystic and non-cystic variations (Figure 7).2 The separation of this abnormally adhered vitreous clump during a broad or localized posterior vitreous detachment (PVD) can result in round operculated holes (Figure 8). Others can result in irregular-shaped operculated retinal holes (Figure 9). These holes can cause chronic or acute RRDs (Figures 9 and 10). 9,10
No consensus exists on treating symptomatic and asymptomatic operculated holes. Prophylactic laser is usually recommended for symptomatic cases. Treatment of asymptomatic holes may reduce the risk of retinal detachment with minimal to no risk to the patient (Figure 11).4,5
 |
| Fig. 9. These cases display irregular retinal breaks with localized subretinal fluid, causing subclinical rhegmatogenous retinal detachments. The first patient (A) requires surgical intervention, either pneumatic (followed by retinopexy) or vitrectomy with gas and laser to repair the retinal detachment, since the excessive fluid around the retinal hole will not allow laser alone to be effective. The second (B) can be treated by prophylactic laser. Click image to enlarge. |
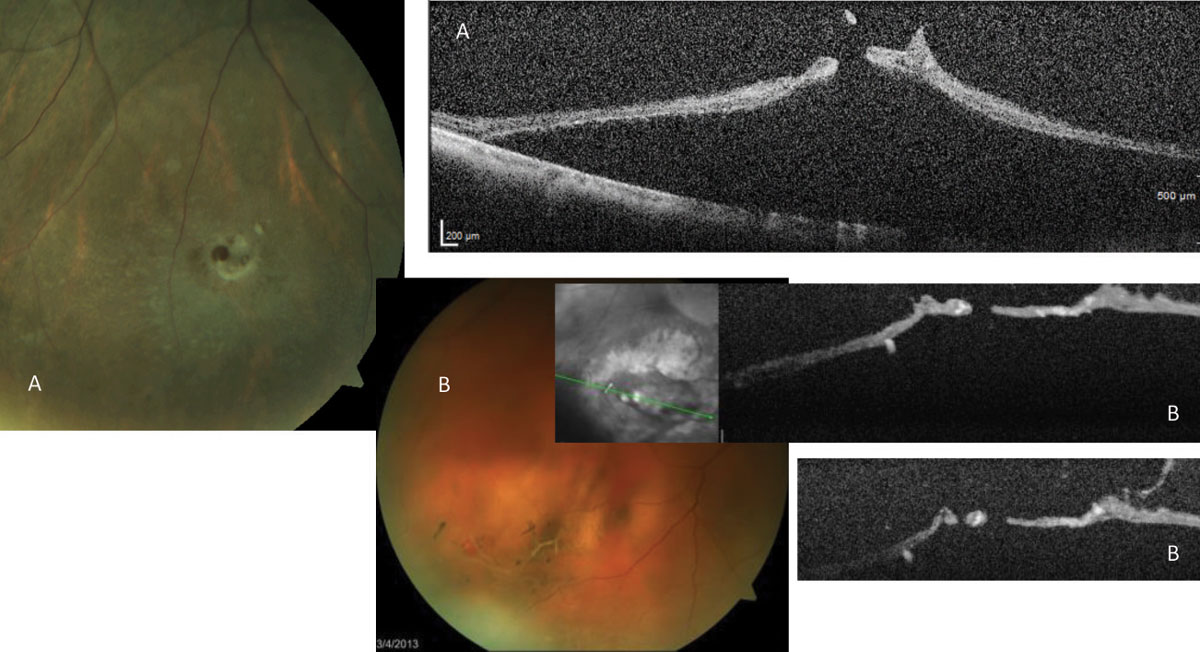 |
Fig. 10. Patient (A)’s images reveal an operculated hole resulting in an acute RRD. Patient (B), who had a pre-existing lattice, displays an operculated hole during PVD resulting in acute RRD. Click image to enlarge. |
 |
| Fig. 11. The patient in Figure 8B is shown here following prophylactic laser treatment. The partial resolution of the fluid cuff is noted while progression to retinal detachment is avoided. Click image to enlarge. |
Horseshoe or Flap Tears
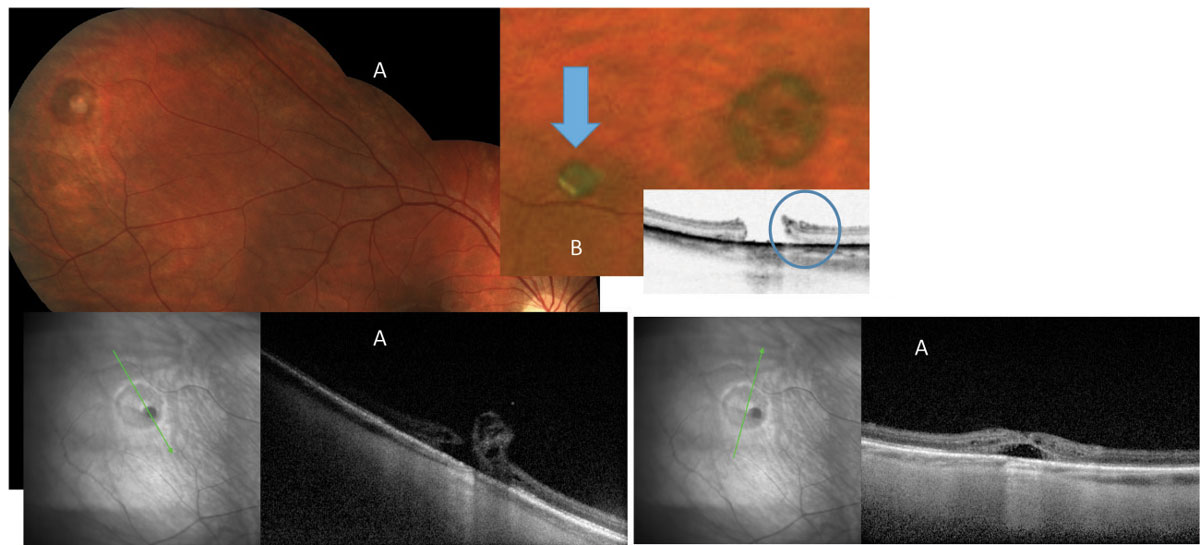
Horseshoe retinal tears (HSRT) are full-thickness breaks of the neurosensory retina that occur as a result of vitreous traction and are usually caused by PVD. Risk factors for HSRT include aging, pre-existing lattice degeneration, myopia and trauma. Although flashes of light and floaters are common symptoms associated with this finding, these can be observed in asymptomatic patients, particularly in the absence of RRD (Figure 12).9,10
Horseshoe retinal tears are the cause of most RRDs (Figure 13).9,10 All HSRT should be surrounded by laser soon after diagnosis (Figure 14).
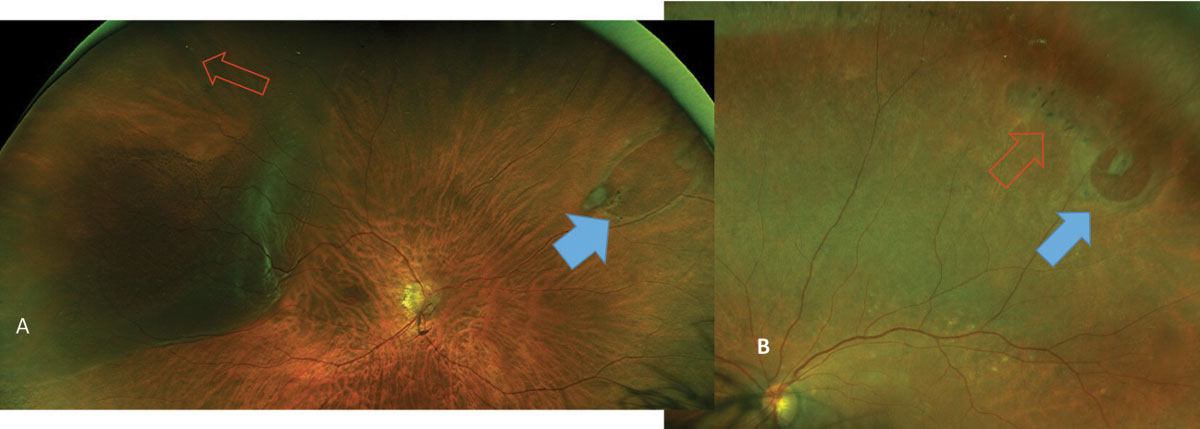 |
| Fig. 12. Image (A) reveals HSRT (blue arrow) with no associated symptom or retinal detachment; however, a small retinal hole (red arrow) has resulted in a slowly progressing retinal detachment, causing a slow-moving shadow in the patient’s peripheral vision. In (B), a horseshoe retinal break (blue arrow) associated with lattice degeneration (red arrow) is seen in an asymptomatic patient. Click image to enlarge. |
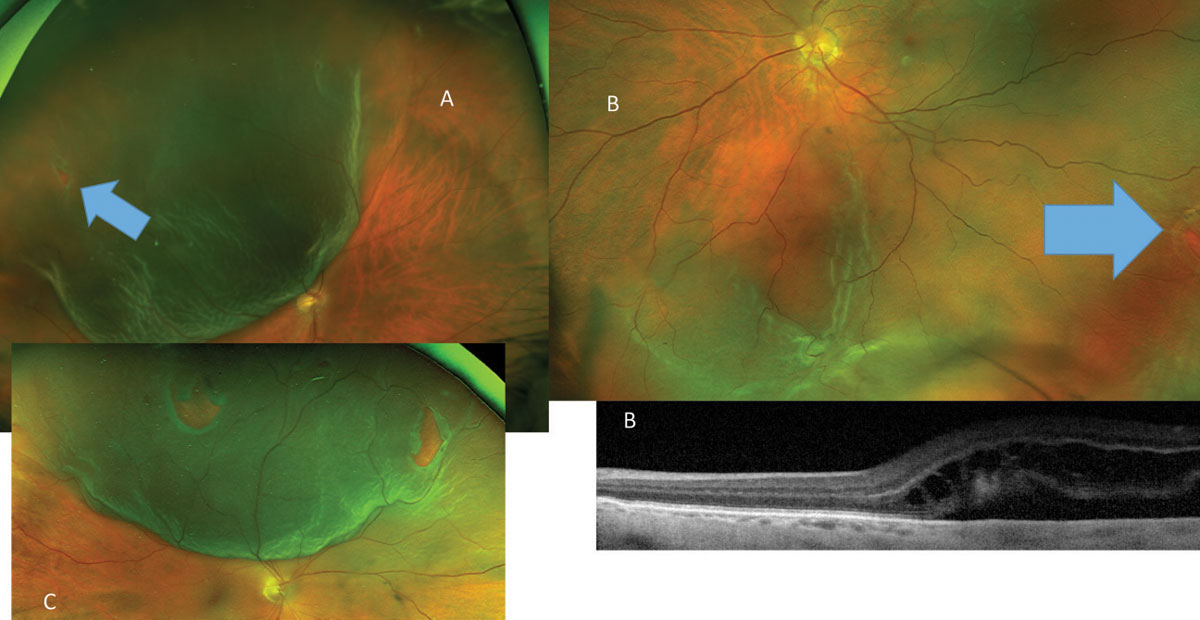 |
Fig. 13. Following PVD symptoms this patient (A) developed a superotemporal RRD caused by a small HSRT (blue arrow), while another patient (B) has developed an inferior macula off RRD from HSRT (blue arrow). These patients required surgical intervention. The RRD in (C) is caused by more than one retinal tear, not an uncommon finding. Click image to enlarge. |
 |
| Fig. 14. Far left, horseshoe tears without retinal detachment (A) are treated with laser. The immediate and long-term of effect of laser (B) is shown, while in long-term hyperpigmentation. Click image to enlarge. |
Giant Retinal Breaks and Retinal Dialysis
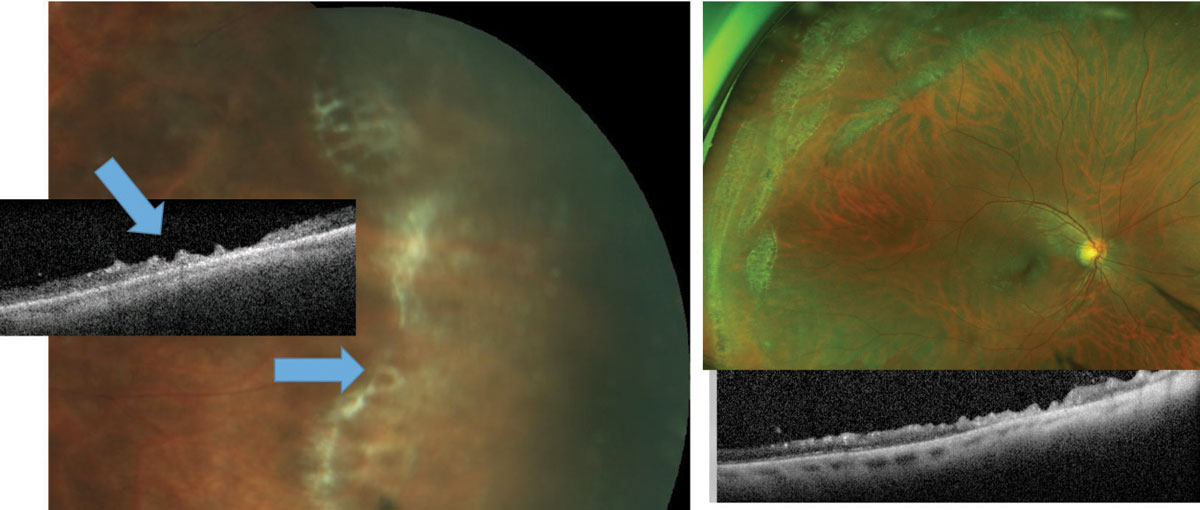
Giant retinal breaks are full-thickness tears that extend at least three clock hours (Figure 15). Retinal detachments caused by giant breaks may require different surgical modalities compared to other RRDs. For instance, perfluorocarbon (PFO) may be used to unfold a retinal detachment intraoperatively.11,12
Retinal dialysis is a break in which the anterior portion is adjacent to the ora serrata (Figure 16A). The majority of these cases are associated with ocular trauma, and most are diagnosed in young patients without posterior vitreous detachment. Managing retinal dialysis can be challenging as well.
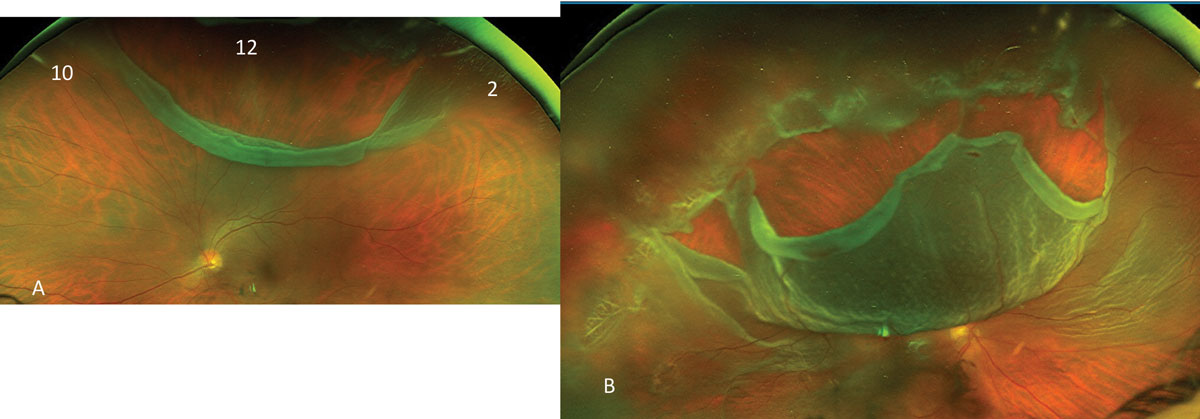 |
| Fig. 15. This more-than-three-clock-hour wide retinal break (A) with limited retinal detachment is seen, while (B) shows a near total RRD. Click image to enlarge. |
Retinal detachment may be prevented by treating the extent of the dialysis with laser retinopexy. If retinal detachment is present, treatment needs to be tailored to the individual patient. Options include: vitrectomy with gas or oil, scleral buckling with or without vitrectomy, and laser retinopexy may still be used if the detachment is limited (Figure 16B). Making the appropriate surgical decision leads to good outcomes in the vast majority of patients.13-15
 |
| Fig. 16. Above, (A) retinal dialysis associated with RRD treated by scleral buckle. At right (B), multiple dialyzed areas in the absence of retinal detachment were treated by prophylactic laser. Click image to enlarge. |
In Conclusion
Retinal holes and tears come in all shapes and sizes with varying management strategies and risk for complication. The one complication associated to some degree with all forms of retinal breaks is retinal detachment, which can result in significant vision loss. As such, all retinal holes and tears —regardless of size, location or shape—should be thoroughly evaluated and properly managed to reduce risk of vision loss for affected patients.
Dr. Rafieetary is an optometrist with Charles Retina Institute in Germantown, TN.
Dr. Huddleston is a vitreoretinal surgeon at the Charles Retina Institute in Germantown, TN.
| 1. Kothari A, Narendran V, Saravanan VR. In vivo sectional imaging of the retinal periphery using conventional optical coherence tomography systems. Indian J Ophthalmol. 2012;60(3):235-9. 2. Choudhry N, Golding J, Manry MW, Rao RC. Ultra-Widefield Steering-Based Spectral-Domain Optical Coherence Tomography Imaging of the Retinal Periphery. Ophthalmol. 2016;123(6):1368-74. 3. Sheu SJ, Lee YC, Chen CJ, Wu TT. Should asymptomatic atrophic retinal holes be treated prophylactically in pseudophakic eyes after Nd:YAG laser posterior capsulotomy? Zhonghua Yi Xue Za Zhi (Taipei). 2001;64(1):31-8. 4. Wilkinson CP. Interventions for asymptomatic retinal breaks and lattice degeneration for preventing retinal detachment. Cochrane database Syst Rev. 2014;9(9):CD003170. 5. Blindbaek S, Grauslund J. Prophylactic treatment of retinal breaks - a systematic review. Acta Ophthalmol. 2015;93(1):3-8. 6. Williams KM, Dogramaci M, Williamson TH. Retrospective study of thegmatogenous retinal detachments secondary to round retinal holes. Eur J Ophthalmol. 2012;22(4):635-40. 7. Byer N. Cystic retinal tufts and their relationship to retinal detachment. Arch Ophthalmol. 1981;99(10):1788-90. 8. Murakami-Nagasako F, Ohba N. Phakic retinal detachment associated with cystic retinal tuft. Graefes Arch Clin Exp Ophthalmol. 1982;219(4):188-92. 9. Combs JL, Welch RB. Retinal breaks without detachment: natural history, management and long term follow-up. Trans Am Ophthalmol Soc. 1982;80:64-97. 10. Davis MD. Natural History of Retinal Breaks Without Detachment. Arch Ophthalmol. 1974;92(3):183-94. 11. Berrocal M, Chenworth M, Acaba L. Management of giant retinal tear detachments. J Ophthalmic Vis Res. 2017;12(1):93. 12. Ao J, Horo S, Farmer L, Chan WO, Gilhotra J. Primary laser photocoagulation for the treatment of giant retinal tears. Retin Cases Brief Rep. 2018;12(4):371-374. 13. Hamrick KE, Helgeson MK. Retinal dialysis. Optom Clin. 1992;2(3):93-112. 14. Qiang Kwong T, Shunmugam M, Williamson TH. Characteristics of rhegmatogenous retinal detachments secondary to retinal dialyses. Can J Ophthalmol. 2014;49(2):196-9. 15. Chang JS, Marra K, Flynn HW, Berrocal AM, Arroyo JG. Scleral Buckling in the Treatment of Retinal Detachment Due to Retinal Dialysis. Ophthalmic Surgery, Lasers Imaging Retin. 2016;47(4):336-40. |

