 |
Q:
The cataract surgeon I use paints a rosy picture of presbyopic intraocular lenses (IOLs) to every patient, but I manage some who aren’t happy post-surgery. How should I best counsel patients about multifocal/presbyopic IOLs to maximize success?
A:
“The best advice to maximize success is proper patient selection and education before the referral—and to hope for a little luck,” says Walter O. Whitley, OD, MBA, director of optometric services at Virginia Eye Consultants. Patients with unreasonable expectations, reduced visual potential, uncontrolled ocular surface disease and significant higher-order aberration should be discouraged at the start. A perfect patient selection process doesn’t exist, Dr. Ajamian adds. “We have had a few I would have bet the farm would do well with a multifocal who didn’t.” Given that, the best a clinician can do is to carefully follow these steps:
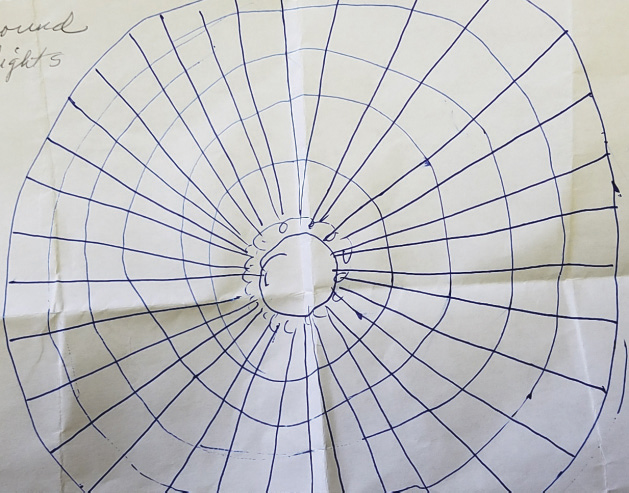 |
| A drawing of postoperative glare by a seemingly “perfect” multifocal candidate. |
1. Manage expectations. “Some technologies may not be able to meet our patient’s vision needs,” says Dr. Whitley. “Each option is a compromise that patients and providers must accept.”
“Tell patients up front that they will wear glasses for certain situations,” says Dr. Whitley. “If they expect to throw their spectacles away, they are not a good candidate.”
Night vision requirements could be another deal-breaker. Although newer IOL designs minimize glare and haloes, some patients may not be able to tolerate them, says Dr. Whitley. As such, he would not recommend presbyopic IOLs to patients with night vision demands, high myopia or large pupils.
Be sure to educate patients who are not ideal candidates for presbyopic IOLs about why they aren’t a good candidate, and would be better suited for a standard IOL and a near prescription post-surgery, he adds. “We also need to let our surgeons know why we aren’t recommending presbyopic IOLs for the patient.”
2. Learn the technology. “Discuss with your surgeon the pros and cons of the various IOL options and their experience with each,” says Dr. Whitley. Coming to an understanding about the various technologies is imperative so your messages to your mutual patients are consistent.
Current options for these patients include the Restor 2.5D and 3.0D IOL (Alcon), and the Tecnis Symfony IOL (Abbott Medical Optics), which are available in toric versions as well. In Dr. Whitley’s experience, the Restor 2.5D maximizes distance vision while providing good intermediate and some near with the least glare. The Tecnis Symfony IOL, meanwhile, uses diffractive echelettes to elongate range of focus and reduce chromatic aberration. Dr. Whitley has seen numerous positive outcomes, and a few negatives, with each option.
3. Optimize the ocular surface. This should be done for all patients prior to the referral. “Dry eye disease can and does affect IOL calculations, leading to residual refractive error, in addition to post-op decrease in vision,” Dr. Whitley says. To minimize the risk of poor visual outcomes post-surgery, he recommends paying attention to the ocular surface pre-op and aggressively treating dry eye signs and symptoms prior to referring for a cataract evaluation.
Other ocular surface conditions that must be addressed prior to surgery include epithelial basement membrane dystrophy, Salzmann’s nodules and pterygium. “If a patient has any of these conditions, multifocal candidate or not, consider a superficial keratectomy or pterygium removal prior to cataract surgery,” Dr. Whitley suggests.
Overall, the optimal presbyopic IOL candidate has realistic expectations, minimal ocular surface disease and higher-order aberrations and good vision potential, Dr. Whitley says. “Remember, it’s all about matching the patient to the ‘lifestyle’ technology and the ‘lifestyle’ technology to the patient. Not everyone will be a candidate for presbyopic IOLs, but taking these steps into account can help make some very happy patients.”

