 |
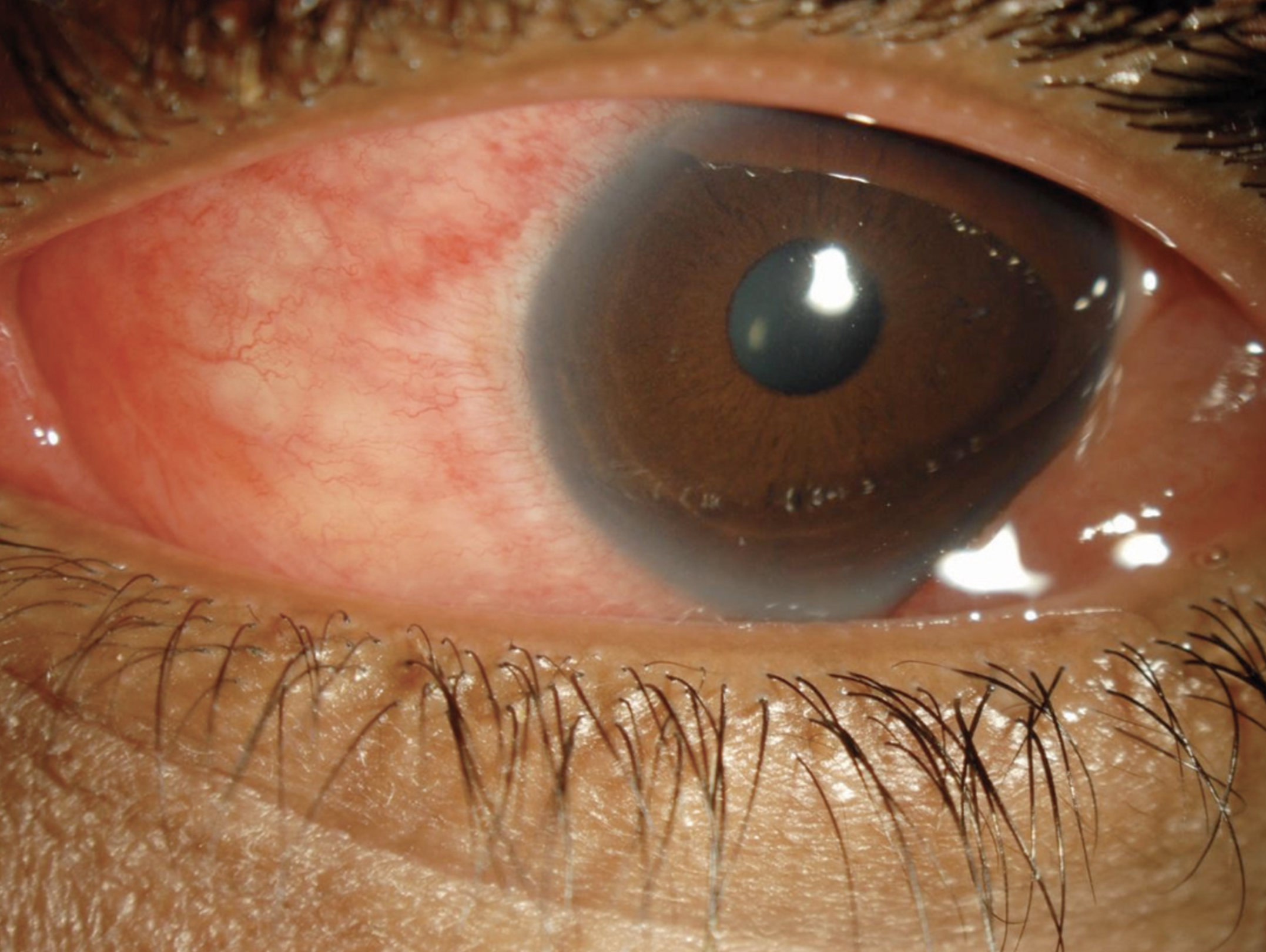
| Lessening the risk of EKC in the acute phase is key. Photo: Joseph W. Sowka, OD. |
Epidemic keratoconjunctivitis (EKC), also known as viral keratoconjunctivitis, is highly contagious, can cause chronic visual disturbances and may result in patients missing work and school. Therefore, shortening the duration of signs and symptoms in the acute phase (when individuals can transmit the infection to the fellow eye and to other people) is key.
To summarize current findings on topical pharmacologic interventions, researchers recently conducted a Cochrane systematic review. They found low-certainty evidence that interventions such as povidone-iodine are more effective than artificial tears and, when combined with steroids, are more effective than steroids alone at reducing acute EKC signs and symptoms.
The Cochrane systematic review included 10 randomized controlled trials (n=892) comparing the efficacy of topical treatments vs. artificial tears or steroid-containing agents for the treatment of acute or chronic EKC. Four studies compared artificial tear or saline interventions, four compared steroid interventions and two three-armed trials compared both approaches. They also compared treatments for patients with subepithelial infiltrates, since these occur in the delayed, chronic phase of EKC.
The review demonstrated that ganciclovir 0.15% and povidone-iodine were both more effective than artificial tears in resolving signs and symptoms of acute EKC within 10 days; they also lowered the risk of subepithelial infiltrate development. Trials comparing the use of povidone-iodine or polyvinyl alcohol iodine combined with steroid vs. steroid alone favored combined therapy for lowering the risk of subepithelial infiltrate development within 21 days in acute EKC. None of the treatments demonstrated improved resolution, eradication or rebound prevention of preexisting infiltrates vs. artificial tears or steroids, the researchers wrote.
Povidone-iodine or polyvinyl alcohol iodine with steroid may have some benefit in acute EKC cases, but the researchers pointed out that the diverse study methodologies and small sample sizes limited the certainty of evidence. For example, EKC was a clinical diagnosis at study entry, and participants were enrolled at various times after infection onset, which likely resulted in different treatment responses.
With such low certainty and no treatments demonstrating significantly greater efficacy against subepithelial infiltrates, the authors concluded that “prevention of subepithelial infiltrates in patients with acute EKC may be more important than eradication of subepithelial infiltrates.”
Liu S, Hawkins BS, Ren M, et al. Topical pharmacologic interventions versus active control, placebo, or no treatment for epidemic keratoconjunctivitis: findings from a Cochrane systematic review. Am J Ophthalmol. March 21, 2022. [Epub ahead of print]. |


