 |
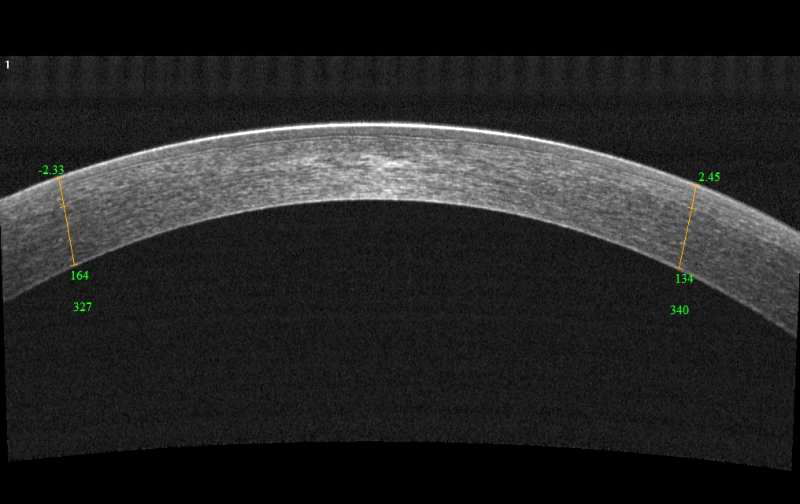
| OCT measurements were found to accurately quantify corneal astigmatism in keratoconus patients. Photo: Visionix. Click image to enlarge. |
Optometrists and ophthalmologists have long relied on placido disc topographers to measure astigmatism and other corneal shape irregularities. Newer devices that use Scheimpflug imaging—which measures both the anterior and posterior corneal curvature—have certain advantages over placido disc topography, especially when used to guide keratoconus treatment protocols. With anterior segment OCT continuing to mature, some wonder if this approach confers benefits as well.
“OCT has several advantages over Scheimpflug imaging; modern OCT systems have higher axial resolution, scan at faster speeds, and can use custom topography software to reduce motion error,” wrote the authors of a recent prospective, cross-sectional, observational study comparing the two. The paper, published in Journal of Cataract & Refractive Surgery, notes that the authors have a financial interest in the OCT technology used; the manufacturer provided financial support but was not involved in data collection or analysis, the paper notes.
The study found that net corneal astigmatism measurements using an as-yet-unreleased OCT software module can be more accurate than Scheimpflug imaging-based topography for keratoconus patients. The researchers calculated net corneal astigmatism in keratoconic and normal eyes with OCT and Scheimpflug imaging. They used four settings: pupil or vertex centration settings with a 3mm or 4mm circular analytical zone. To obtain net corneal astigmatism, corneal elevation maps were taken from OCT images and fitted with Zernike polynomials. The study authors evaluated the accuracy of net corneal astigmatism measurements by using manifest refraction astigmatism.
The analysis included 46 eyes with manifest or subclinical keratoconus and 52 normal (control) eyes. When looking at OCT measurements in keratoconus, the researchers reported that better accuracy was achieved with vertex centration and the 4mm analytical zone. Additionally, the data showed that agreement with manifest refraction was significantly better with OCT when compared with Scheimpflug imaging.
No significant difference between instruments and settings in control eyes was observed, according to the study authors, who noted that the accuracy and repeatability of net corneal astigmatism were comparable between the technologies in normal eyes. This is consistent with prior literature.
“OCT was able to measure net corneal astigmatism with better accuracy and precision,” the researchers concluded. “Measurements may be more accurate using pupil centration and a smaller analytical zone in subjects with keratoconus.”
They also noted that, while significant progress has been made in OCT imaging, further work is required since the accuracy and repeatability for keratoconic eyes are still worse vs. those obtained for normal eyes.
Llorens-Quintana C, Lee DJ, Pavlatos E, et al. Measuring corneal astigmatism using optical coherence tomography in keratoconus. J Cataract Refract Surg. May 26, 2022. [Epub ahead of print]. |


