 |
Q: Many gas permeable (GP) lens wearers rinse their lenses with water. There seems to be a consensus that scleral lens exposure to water carries an even greater risk. Is this true? If so, what makes this modality different than small-diameter GP lenses?
"Both GP and soft lenses can act as vectors for microbes, ultimately resulting in ocular infections,” according to Mile Brujic, OD, of Ohio, David Kading, OD, of Washington and Nikhita Jacobs, an incoming optometry student. Lenses exposed to water are of significant concern, especially due to the presence of Acanthamoeba.1-3 This organism exists in both cystic and trophozoite forms and, as such, is extremely resistant and exists within water.3
Best Care Practices
GP contact lens wearers have a bad habit of rinsing their lenses in water, note Drs. Brujic and Kading and Ms. Jacobs. Lens rinsing can occur prior to storage in multipurpose disinfecting solution, after removal from the solution in preparation for lens application to the eye or after manual lens cleaning.4 Some patients even go as far as storing their lenses in water. Drs. Brujic and Kading have seen all of these scenarios in their practices.
 |
|
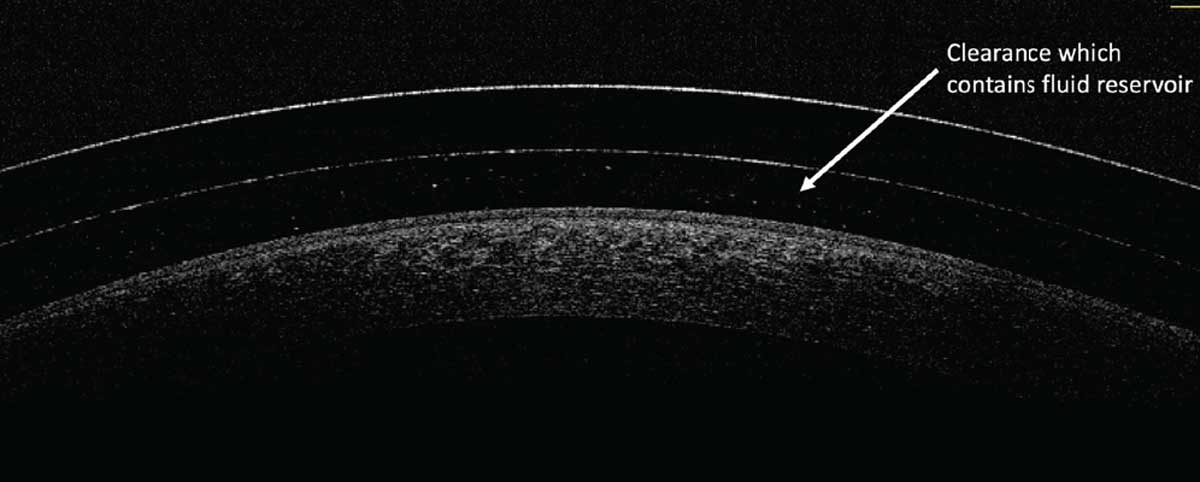
The space between the posterior lens surface and the anterior corneal surface contains the fluid reservoir. Click image to enlarge. |
Contact lenses should never come in contact with water, Drs. Brujic and Kading and Ms. Jacobs emphasize. The trio adds that contamination of lenses with Acanthamoeba specifically can cause sight-threatening infections and should be avoided at all costs. They highlight patient education as a possible solution to breaking bad habits. Also, observing patients apply and remove their lenses may help pinpoint shortcomings in the lens care process.
If swimming in contact lenses, Drs. Brujic and Kading and Ms. Jacobs recommend wearing goggles that effectively minimize exposure to water. If showering in lenses, direct contact with water should be avoided.
Scleral lenses present an additional challenge, they caution. Small-diameter GPs move with every blink, increasing the chances that microbes will be removed from the lens surface. On the other hand, scleral lenses, when fit appropriately, should maintain very little movement on the surface of the eye. Consequently, the fluid reservoir that is present between the cornea and the posterior surface of the lens will remain in contact with the cornea throughout the day. As such, appropriate care of this lens modality is critical to optimize corneal safety. Any contact between water and scleral lenses exposes the cornea to unnecessary and avoidable risk.5
Scleral lenses are often fit using diagnostic fitting sets, Drs. Brujic and Kading and Ms. Jacobs note. Accordingly, it is critical to understand and follow contemporary scleral lens disinfecting protocols to ensure they are appropriately and properly disinfected. Several organizations, including the American Optometric Association, American Academy of Optometry, Gas Permeable Lens Institute and Contact Lens Manufacturers Association, collaborated to create a consensus on in-office disinfection protocols.6 After any scleral lens is placed on a patient’s eye, it should go in a 3% hydrogen peroxide non-neutralizing case for three hours. The lens should then be rinsed with multipurpose solution, patted and stored dry. It shouldn’t be exposed to water at any point during this process.
Additionally, contemporary hydrophilic surface treatments, such as Tangible Science’s Hydra-PEG, provide a more comfortable wearing experience. They also minimize surface deposits, as lens exposure to water can remove the surface treatment.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.1. Zimmerman AB, Richdale K, Mitchell GL, et al. Water exposure is a common risk behavior among soft and gas-permeable contact lens wearers. Cornea. 2017;36(8):995-1001.
2. Cope JR, Collier SA, Schein OD, et al. Acanthamoeba keratitis among rigid gas permeable contact lens wearers in the United States, 2005-2011. Ophthalmology. 2016;123(7):1435-41.
3. Sharma S, Ramachandran L, Rao GN. Adherence of cysts and trophozoites of Acanthamoeba to unworn rigid gas permeable and soft contact lenses. CLAO J. 1995;21(4):247-51.
4. Lindsay RG, Watters G, Johnson R, et al. Acanthamoeba keratitis and contact lens wear. Clin Exp Optom. 2007;90(5):351-60.
5. Cubuk MO, Al FD, Usluca S, Bilgiham K. Acanthamoeba keratitis associated with scleral contact lens use in a keratoconus patient. Beyoglu Eye J. 2020;5(1):53-6.
6. In-office disinfection of multi-patient use diagnostic contact lenses. www.gpli.info/wp-content/uploads/2020/03/2020-01-15-in-office-disinfecting-of-diagnostic-lenses.pdf. Accessed February 14, 2022.

