The popularity of paintball—a strategic “war game” where the goal is to eliminate opponents by “tagging” them with gelatin-covered capsules containing a non-toxic, water-soluble dye—has grown immensely and is even used in military, law enforcement and security training. The paintballs themselves are propelled from a “gun” (referred to as a paintball marker), which uses a compressed air or CO2 tank. The muzzle velocity from a compressed CO2 powered paint gun can meet or exceed 300 ft/s. Eye doctors will naturally recognize the game’s distinct risk: ocular injury. In fact, since the game’s popularity has grown, the incidence of ocular injury has increased significantly. Optometrists aren’t the only ones picking up on this. The American Society for Testing and Materials includes eye protective devices among its minimum safety requirements for paintball games due specifically to the high risk of ocular injury. Still, most paintball-related ocular injuries occur when players neglect or remove protective eyewear.4
 | |
| This slit lamp image shows traumatic IOL dislocation, a potential complication of ocular trauma, such as being struck with a projectile paintball. Photo: Mark T. Dunbar, OD. |
This article reviews managing patients who present with urgent injuries sustained from these, and other sports-related, activities.
Casualty Presentation
An 18-year-old male with a right eye injury presented with entrance acuity at the level of hand motion (HM) and an intraocular pressure (IOP) of 17mm Hg. An anterior segment examination revealed right upper lid edema and bruising. A slit-lamp examination confirmed corneal edema with mild folds centrally, a subconjunctival hemorrhage with chemosis and 3+ cell and flare with a 2mm hyphema in an adequately formed anterior chamber. The cornea and conjunctiva were Seidel negative. The right pupil was 5mm with poor reactivity. The lens appeared centered, but it was difficult to assess with clarity. Funduscopic exam was limited due to severe vitreous hemorrhage. A B-scan ultrasound did not suggest retinal detachment.
The patient was referred to our staff retinal specialist the next day. A biometry was repeated and, once again, did not suggest retinal detachment.
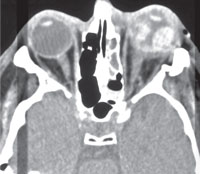 | |
| This CT scan reveals a ruptured globe following ocular trauma. It can be difficult to make such a diagnosis without a CT scan if profuse hemorrhaging obscures visibility. Photo: Dante J. Pieramici, MD. |
However, as the vitreous hemorrhage began to clear, a fundus examination did reveal a retinal detachment in the superior quadrant with an associated sub-macular choroidal rupture. A pars plana vitrectomy (PPV), lens extraction and IOL implantation were performed. In the patient’s final examination, the retina was attached and his visual acuity was recorded as 20/200.
Types of Trauma
Paintball-related ocular trauma most frequently consists of coup and contrecoup trauma resulting in a significant increase in IOP and equatorial expansion. Blunt trauma from paintball projectiles can cause anterior segment injury resulting in hyphema, traumatic cataract, crystalline lens dislocation, angle recession and iridodialysis. Posterior segment injury may include vitreous hemorrhage, commotio retinae, choroidal rupture, traumatic macular hole and retinal tear or detachment. Scleral rupture related to a suspected centerline hit at relatively close range has also been reported.5,6
A Bascom Palmer data analysis found 28% of patients with paintball-related eye injuries suffered from a ruptured globe, 19% had a retinal detachment, 81% required surgery and, ultimately, 22% of eyes required enucleation.
When confronted with a patient who has suffered a sports-related traumatic ocular injury, be sure to determine the nature of the injury. The impact from larger objects, such as basketballs, soccer balls, boxing gloves, etc., are likely to be partially absorbed by the periorbital rim. These objects can still cause significant ocular injury, but smaller and fast-traveling objects like paintballs have greater potential to adversely affect the globe.
| The Stats Due to increased regulation and improvements in EPDs, ocular paintball injuries in general and especially during organized regulated play appear to be on the decline. ASTM international investigated the patterns of ocular paintball trauma that presented to 100 emergency room departments (EDs) in the United States from 2001 to 2010. Using the National Electronic Injury Surveillance System, they identified 11,827 paintball related ocular injuries.1 They determined the following: | ||
Gender: 92.2% were male
Locale:
1. US Consumer Product Safety Commission. National Electronic Injury | Year of Injury:
| |
Friendly Fire
In our case, the patient indicated that he was wearing an eye protective device during an organized paintball competition. When the signal sounded that the game was over, he immediately took his mask off and was struck by an errant round. He did not know the distance or direction from which the projectile was fired.
Assessment of an eye immediately following such an injury can be difficult due to significant edema, haze or blood obscuring the view. As this case shows, even B-scan ultrasound can be inconclusive when addressing posterior segment damage.
Ordering restricted activity, proper head positioning (minimum 45 degree upright angle) cycloplegics, IOP lowering agents, a Fox shield and close monitoring are sometimes warranted until the view of ocular structures improve.
 | |
| Hyphema, like the kind seen in this slit lamp photograph, is often caused by blunt trauma, such as being struck with a projectile paintball. Photo: Alan G. Kabat, OD. | |
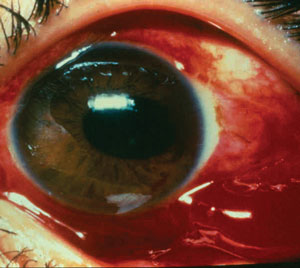 | |
| This ocular hemorrhage following trauma may be accompanied by a ruptured globe. Photo: Dante J. Pieramici, MD. |
The main goal at the initial visit is to rule out signs of a ruptured globe. Risk factors for an open globe include penetrating lid injury, hyphema, hypotony, peaked pupil, shallowed or absent anterior chamber, 360 degree bullous subconjunctival hemorrhage, iridodialysis, lens dislocation, relative afferent pupillary defect, positive Seidel test and significant reduction in vision.7 If you suspect a ruptured globe, consult a retinal specialist immediately. The patient will likely be started on oral antibiotics and scheduled for exploratory or globe reconstruction surgery within 24 hours.
Not all ruptured globe cases will present with each and every finding listed above. If there is any question regarding the integrity of the globe, consider a CT scan of the eye and orbit, or refer.
Finally, make sure all patients participating in eye-threatening sports are educated on the importance of wearing eye protection and—take a lesson from our patient—remind patients not to remove their EPD until they have exited the field of play.
1. American Society for Testing and Materials. Standard practice for paintball field operation. In: 1997 Annual Book of ASTM Standards. West Conshohocken, Pa: American Society for Testing and Materials;1997:1391–4012. Zwaan J, Bybee L, Casey P. Eye injuries during training exercises with paint balls. Mil Med. 1996;161:720–2
3. Benson W. The effects of blunt trauma on the posterior segment of the eye. Trans Pa Acad Ophthalmol Otolaryngol. 1984;37:26–33.
4. Easterbrook M, Pashby T. Ocular injuries and war games. Int Ophthalmol Clin. 1988;28:222–4.
5. Taban M, Taban M, Sears JE. Ocular findings following trauma from paintball sports. Eye (Lond). 2008;22:930–4.
6. Greven C, Bashinsky A. Circumstance and outcome of ocular paintball injuries. Am J Ophthalmol. 2006;141:393.
7. Assessment and Management of Ocular Trauma. http://www.eyerounds.org/tutorials/trauma.htm. Updated January 28, 2008. Accessed November 10, 2015.

