 |
|
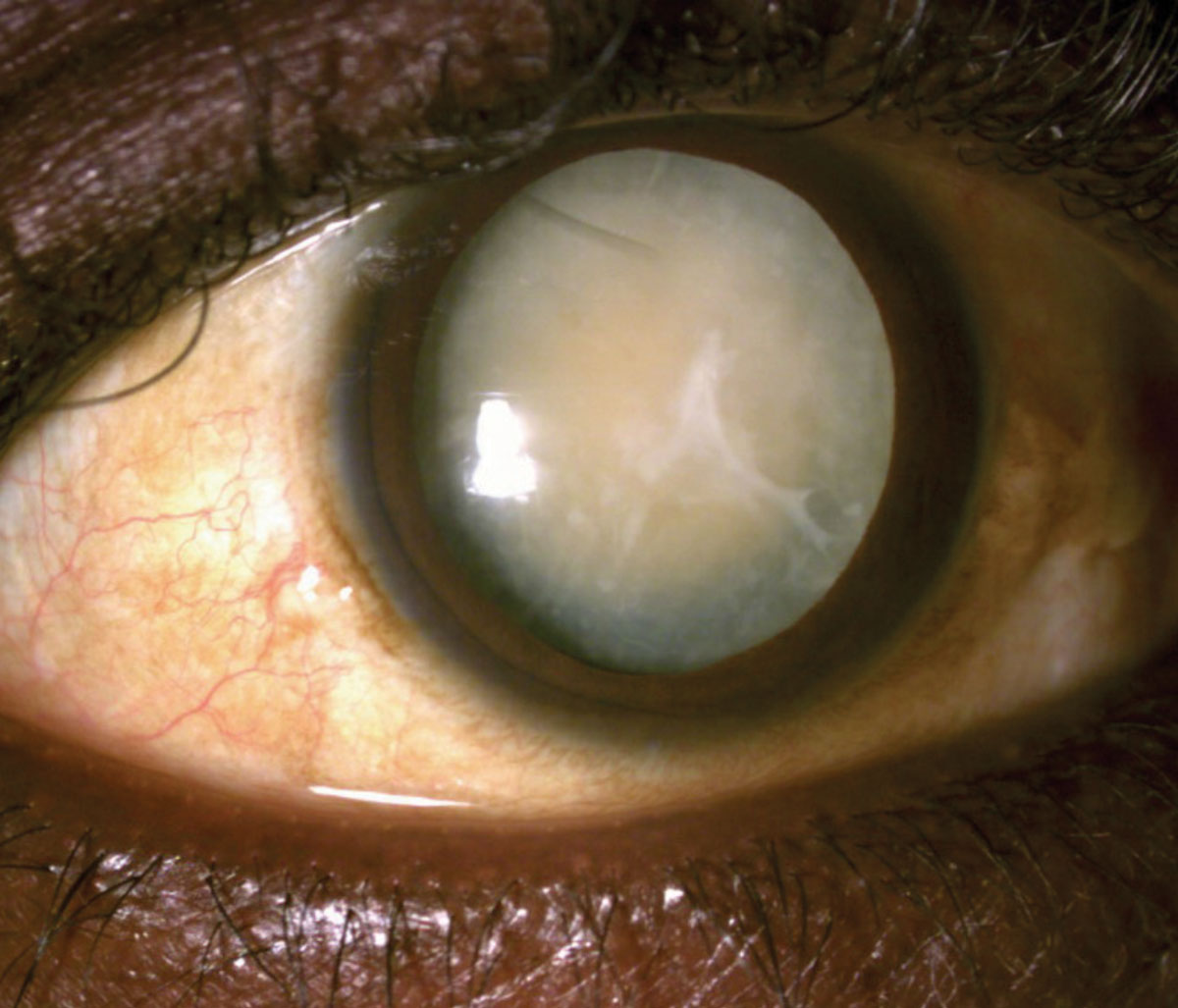
Watching videos about their options helped cataract surgery patients feel more confident and informed throughout the decision process, this study suggests. Photo: Joseph Sowka, OD |
Cataract surgery patients have several decisions to make leading up to the procedure and must be well-informed of their options so they’re able to choose the one that best suits their needs and desired outcomes. Unfortunately, the COVID-19 pandemic has made these sorts of consultations more difficult, considering the restrictions on family accompaniment and the hindrance of masks on communication, especially for those hard-of-hearing.
Patient Decision Aids (PDAs) could play an important role in improving the decision-making process for cataract surgery patients during the COVID-19 era by offering an explanation of the available options, including benefits, complications and indications of surgery, all through a video platform. A recent study confirmed that video-based PDAs (VBPDA) can effectively aid patients as they work through the decision-making process prior to cataract surgery.
Patients from a single-center practice referred for cataract surgery consultations were recruited for this study (n=147). Prior to ophthalmologist examination, each participant watched part one of two of the VBPDA. Post-examination, the patients continuing with surgery (n=111) were shown part two of the VBPDA before engaging in shared decision-making with the ophthalmologist. Decisional conflict was quantified using the Decisional Conflict Scale (DCS), a 16-item scale that measures one’s perceptions of the quality of the decision made, scored from zero to 100 (low to high decisional conflict). A DCS score below 25 indicates low decisional conflict, while a score over 25 indicates feelings of uncertainty.
The median DCS score for patients proceeding with cataract surgery was 9.38. Of the patients, 76 scored below 25 (low decisional conflict), 30 scored between 25 and 37.5 (moderate decisional conflict) and just five scored above 37.5 (high decisional conflict). In addition, 79.6% of patients believed their decision would have been more difficult without the VBPDA, and 87% found the VBPDA to be an informative tool prior to giving consent.
Although 26% of patients in the study self-reported being hard-of-hearing, 96.45% found the VBPDA to be clearly audible. While masks prevent lip-reading that some people rely on, these video-based aids may be a helpful and convenient solution.
“VBPDAs may help with the implementation of new modifications beyond cataract surgery consent,” the authors of the study wrote. “For example, the videos can provide information for other commonly performed ophthalmic procedures, including laser peripheral iridotomy, YAG capsulotomy and selective laser trabeculoplasty or even procedures outside of ophthalmology.” This study’s findings demonstrate that VBPDAs can be an effective and accessible tool for improving the patient decision-making experience, which may be especially helpful throughout the COVID-19 pandemic.
Man K, Mundra PS, Anabtawai A, et al. Improving the patient decision making experience for cataract surgery during the COVID-19 era. Can J Ophthalmol. August 11, 2021. [Epub ahead of print]. |

