 |
Q: One of my contact lens patients has a severe Pseudomonas infection with scleral extension. What options are available to salvage the eye?
Colleagues Anat Galor, MD, MSPH, and Guillermo Amescua, MD, of the Bascom Palmer Eye Institute, draw on their clinical knowledge and expertise to dissect the findings of a similar case they saw and offer a solution for affected patients.
Case Presentation
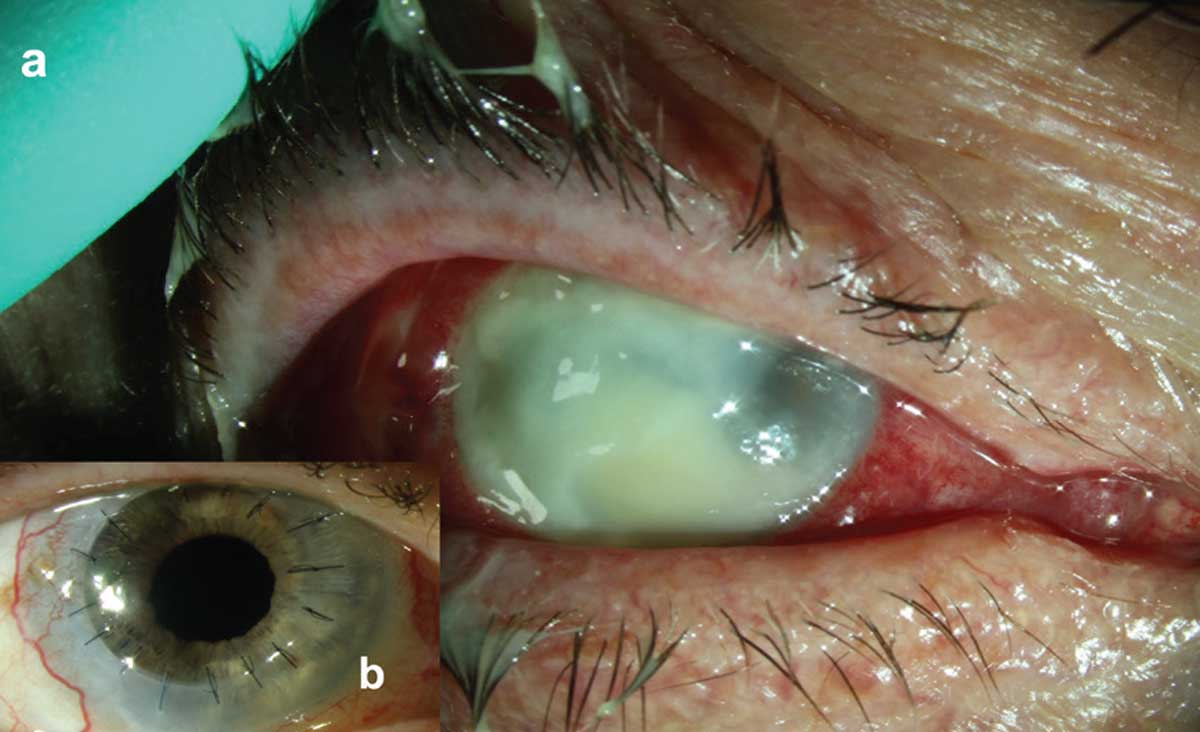 |
| Pseudomonas keratitis with associated stromal necrosis and hypopyon and early involvement of superotemporal scleral tissue (a). Clean and compact corneal graft with intact corneal epithelium and quiet ocular surface (b). Click image to enlarge. |
A 76-year-old white male presented with a four-day history of pain and redness OD. He had a large corneal ulcer extending to the temporal sclera with severe thinning of the cornea and a large hypopyon. He was started on hourly topical antibiotics (vancomycin 25mg/ml, tobramycin 14mg/ml and ciprofloxacin 0.3%) and oral ciprofloxacin 500mg BID. Cultures showed Pseudomonas aeruginosa sensitive to tobramycin and ciprofloxacin, so the vancomycin was discontinued. Despite topical and oral antibiotics, the infiltrate and corneal thinning worsened.
Prednisolone acetate 1% eye drops were started twice daily to address the inflammation, but the infection continued to progress. As such, the patient underwent rose bengal photodynamic antimicrobial therapy (RB-PDAT) four days after presenting and saw immediate improvement in pain.
Over the next few weeks, the infiltrate condensed and re-epithelialization slowly occurred with the help of autologous serum tears. A subconjunctival triamcinolone injection was given due to pupillary membrane formation.
After 2.5 months, the epithelium was fully healed with an underlying large corneal scar and the fibrous process in the anterior chamber had resolved. However, BCVA remained count fingers. Five months later, the patient underwent a PKP, iris synechiolysis, cataract extraction and IOL placement. Fortunately, BCVA eight months post-surgery was 20/25 and IOP was normal.
Treatment Option
During the last decade, CXL has been proposed as an adjuvant treatment for infectious keratitis. The initial treatment consisted of riboflavin as the photosensitizing agent coupled with UVA light, an approach used to manage progressive keratoconus.
Drs. Galor and Amescua evaluated rose bengal as the photosensitizing agent activated by a green fluorescent light built by their bioengineering team and found it to be more efficient at killing bacteria and fungi in vitro than riboflavin.1 The duo thus started using this therapy in patients with severe keratitis that was unresponsive to medical therapy.
RB-PDAT involves the topical application of rose bengal 0.1% to the de-epithelized cornea for 30 minutes followed by 15 minutes of irradiation provided by a custom-made LED light source (525nm) for a total energy of 5.4J/cm2. The proposed mechanism of action in keratitis is that photosensitization stimulates energy transfer to nearby triplet oxygen molecules, which results in the formation of reactive oxygen species (ROS) such as a singlet oxygen molecule. ROS interact with surrounding organic compounds in cells and tissues to produce a variety of effects, including eradication of a wide array of bacteria and fungi. In addition, stiffening of the collagen fibers may portend resistance to enzymatic degradation and slow corneal melting.
Drs. Galor and Amescua have had promising outcomes with RB-PDAT, coupled with medical therapy, in treating cases of severe bacterial and fungal infections. Fortunately, in patients who later undergo a PKP, they note that outcomes are generally excellent.2
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.2. Naranjo A, Arboleda A, Martinez JD, et al. Rose bengal photodynamic antimicrobial therapy for patients with progressive infectious keratitis: a pilot clinical study. Am J Ophthalmol. 2019;208:387-96.

