 |
 |
 |
|
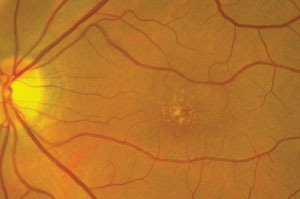
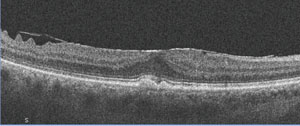
1-3. Our patient's fundus examination revealed interesting macular changes (OD top, OS middle). Additionally, what does the spectral-domain optical coherence tomography scan of our patient's right eye (bottom) reveal?
|
A 65-year-old Hispanic female presented with mild blur at distance and near in both eyes that had persisted for six months (OD>OS). Her ocular history was significant for episcleritis in her right eye five years earlier, which resolved uneventfully.
Her medical history was significant for high cholesterol, which was medically controlled (she couldn’t remember the drug’s name).
On examination, her best-corrected visual acuity measured 20/25 OD and 20/20 OS. Extraocular motility testing was normal. Her confrontation visual fields were full to careful finger counting OU. Her pupils were equally round and reactive, with no evidence of afferent defect. Her anterior segment was unremarkable. Intraocular pressure measured 15mm Hg OU.
On dilated fundus exam, the vitreous was clear OU. She exhibited moderate-sized cups, with good rim coloration and perfusion in both eyes. The peripheral retina was normal in both eyes.
Both maculae showed obvious changes (figures 1 and 2). Additionally, we obtained a spectral-domain optical coherence tomography (SD-OCT) scan of her right eye (figure 3).
Take the Retina Quiz
1. What do the yellow-white changes in both maculae represent?
a. Drusen.
b. Intraretinal flecks.
c. Exudate.
d. Crystals.
2. What does the SD-OCT scan show on her inner retina?
a. Vitreomacular traction.
b. Macular telangiectasia.
c. Epiretinal membrane (ERM).
d. Retinal striae.
3. What does the SD-OCT show in the outer retinal layers?
a. Drusen.
b. Choroidal neovascularization (CNV).
c. Disruption of the inner segment/outer segment (IS/OS) junction.
d. Pigment epithelial detachment.
4. What is the correct diagnosis?
a. Dry age-related macular degeneration (AMD).
b. Dry AMD and ERM.
c. Wet AMD with CNV.
d. Vitreomacular traction with macular edema.
5. How should this patient be managed?
a. Observation.
b. Intravitreal anti-VEGF injection.
c. Intravitreal Jetrea (ocriplasmin, ThromboGenics) injection.
d. Vitrectomy and membrane peel.
Discussion
The yellow-white deposits seen in both maculae represent drusen. Therefore, our patient has some form of macular degeneration. The SD-OCT scan detailed the irregular elevations of the drusen at the level of the retinal pigment epithelium (RPE), and revealed an intact IS/OS junction that was pushed forward from the drusen. We documented no fluid or CNV, which confirmed that the patient had dry AMD.
Aside from macular degeneration, it’s important to note that the SD-OCT showed a loss of the foveal depression and a slightly thickened macula OD. Indeed, the foveal thickness in her right eye measured 336µm, compared to 254µm in her left eye.
So, what else is going on with this patient? In addition to dry AMD, she has an ERM in her right eye. On the SD-OCT scan, the ERM can be visualized as a highly reflective entity at the level of the internal limiting membrane (ILM). More temporal to the fovea, you can see that the ILM is corrugated with focal elevations. Clinically, this is seen as retinal striae.
An ERM represents a fibrocellular membrane that grows onto the retinal surface. It is comprised of glial, RPE and collagen cells, as well as macrophages and fibrocytes.1
The exact mechanism by which RPE cells migrate onto the surface of the retina is not completely understood; however, it is believed that an ILM dehiscence might catalyze ERM development. Up to 90% of patients with ERMs also develop posterior vitreous detachments (PVDs). Thus, the process of PVD development may yield a small dehiscence in the ILM, permitting the fibrocellular membrane to form.1
Approximately 90% of ERMs remain stable and do not affect visual acuity significantly; however, the remaining 10% typically progress.1 For patients who develop symptomatic ERM, pars plana vitrectomy with membrane peel often is indicated. Surgical success is dependent on ERM extent and severity, as well as the level of the visual acuity.
There is no definitive standard to determine when surgical intervention is necessary for ERM. Spectral-domain optical coherence tomography provides a good barometer for detecting structural changes within the retina––either at the level of the IS/OS junction, or if patients develop fluid or cystic changes within the retina. Once this occurs, most retinal specialists agree that surgery is warranted.
It is important to remember that postoperative visual acuity is dependent on the extent of retinal architecture changes. Typically, the anticipated visual recovery is approximately 50% better than the entering acuity level. In other words, ERM patients who present with an entering acuity of 20/60 can expect to achieve 20/30 or better following surgery.
Our patient’s vision is still very good, and she did not report any distortion or metamorphopsia. Our hope is that she will fall into that 90% category, and won’t exhibit ERM progression.
Nevertheless, she does have early dry age-related macular degeneration. So, we recommended an AREDS2 vitamin supplement that contains both lutein and zeaxanthin. We instructed her to return in six months for additional monitoring and follow-up.
Answers:1) a; 2) c; 3) a; 4) b; 5) a.
1. Smiddy WE, Maguire AM. Idiopathic epiretinal membranes. Ultrastructural characteristics and clinicopathologic correlation. Ophthalmology. 1989 Jun;96(6):811-20.

