 |
Q:
I occasionally see patients with classic Thygeson’s superficial punctate keratopathy. I find these cases to be difficult to treat. What are today’s best management options for these cases? Also, is there anything new regarding the disease’s etiology?
A:
“Thygeson’s superficial punctate keratitis (TSPK) was first introduced by Phillips Thygeson in the mid-twentieth century,” says James Aquavella, MD, professor of ophthalmology at the University of Rochester Flaum Eye Institute. “Characteristically, it produces symptoms of photophobia, tearing and foreign body sensation.”
According to Dr. Aquavella, the disease’s slit lamp appearance is almost pathognomonic, typically with five to 10 intraepithelial satellite lesions in the central cornea. “The lesions are discrete, not confluent, limited in number to the central cornea, and the vision is usually only minimally impaired,” he says. “There is usually bilateral involvement, although the extent may vary from left to right.”
TSPK usually doesn’t cause staining, but “on occasion you will find an overlying epithelial disruption,” says Dr. Aquavella. “There is also minimal discharge and minimal or absent conjunctival injection.”
The disease is known for frequent bouts of recurrence. While this can make management frustrating, it also makes diagnosis easier when combined with the fact that TSPK is chronic and often bilateral, Dr. Aquavella says, because it separates the disease from similar conditions such as epidemic keratoconjunctivitis (EKC). “Usually TSPK patients still experience vision ranging from good to normal, while the vision in EKC is usually compromised,” Dr. Aquavella says. “Also, unlike TSPK, EKC is not quickly reversed.”
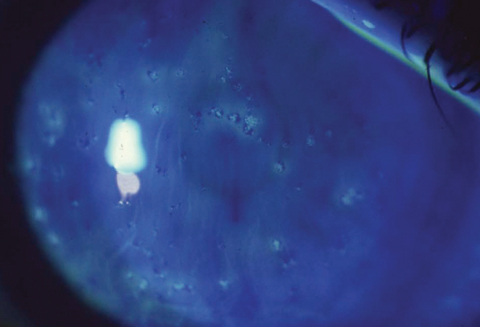 |
| Standard TSPK presentation includes small, central epithelial opacities. Photo: Ron Melton, OD, and Randall Thomas, OD |
Management
“In TSPK, pain relief is instantaneous with the application of a bandage contact lens,” says Dr. Aquavella. Here, it is standard to add a prophylactic antibiotic, he adds, but antibiotics are not indicated with other treatments.
Another approach is the use of a mild steroid such as fluorometholone, loteprednol or, on occasion, 1% methylprednisolone. According to Dr. Aquavella, these will quickly heal any TSPK lesions. From there, the steroids should be slowly tapered over about a month or so. “Perhaps start with tapering the steroid to BID and then, ultimately, once or twice a week,” says Dr. Aquavella. “If there is no pressure response, some patients will require an occasional extra drop to keep the condition in check.”
Other options that have proven effective are cyclosporine in olive oil and tacrolimus, Dr. Aquavella says.
Etiology
The jury is still out on an exact cause for TSPK. Although viral mechanisms such as herpes simplex virus and varicella zoster virus have been suggested in early, limited studies, more recent research has not been able to show viruses as the culprit.1-4 “When TSPK lesions clear there is no sign of viral involvement,” says Dr. Aquavella. “Also, post-viral conditions often linger for longer periods.”
According to Dr. Aquavella, autoimmune processes have been long suspected to play a role in TSPK, and research shows that autoimmune diseases such as Sjögren’s syndrome have a positive association with the disease.5 Still, a definitive underlying cause for TSPK remains unknown.
1. Braley AEK, Alexander RC. Superficial punctate keratitis: isolation of a virus. Arch Ophthalmol. 1953;50:147. |

